Kidney Failure and Constipation: Causes, Symptoms, and Treatments
Understand the link between kidney failure and constipation, key causes, symptoms, and effective treatments for digestive relief.
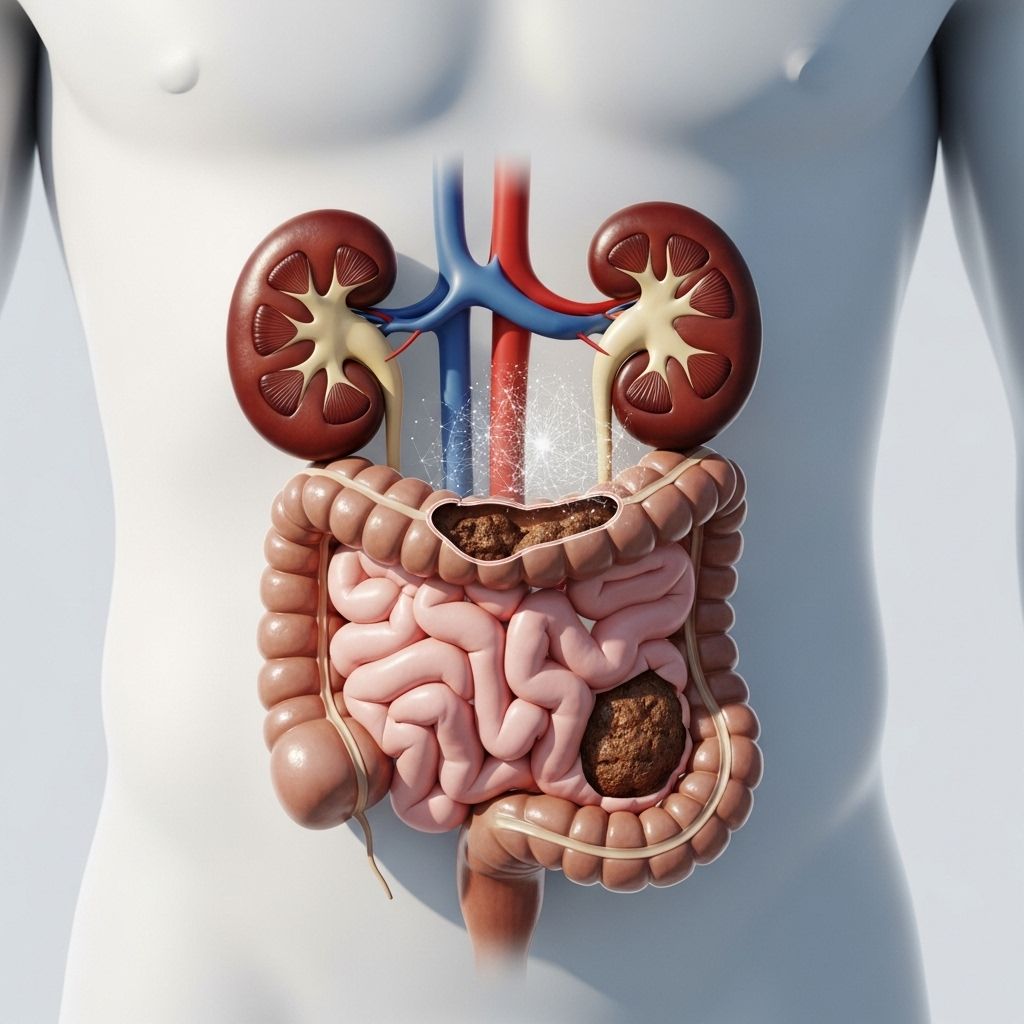
Kidney Failure and Constipation: Understanding the Connection
Chronic kidney disease (CKD) and kidney failure are well-known for their impact on various bodily systems, but their relationship to constipation is often overlooked. Many individuals living with CKD or kidney failure experience digestive disturbances, including constipation, for a variety of reasons. This article explores how kidney disease leads to constipation, the main symptoms to watch for, and what treatment options exist to help people achieve digestive comfort.
Why Does Chronic Kidney Disease Cause Constipation?
CKD can result in constipation due to several interconnected factors. The following sections discuss these causes in detail:
- Renal Diet Limitations: Kidney-friendly diets often restrict high-fiber foods, which are crucial for healthy digestion. Traditional renal diets banned many kidney-safe fruits and vegetables, but newer dietary recommendations are somewhat less restrictive, permitting many fiber-rich options where appropriate.
- Fluid Restrictions: Later-stage kidney disease sometimes necessitates strict limits on fluid intake, especially in dialysis patients. Low hydration can slow digestion and make stool harder to pass, increasing the risk of constipation.
- Secondary Health Conditions: Conditions frequently seen alongside kidney disease—such as diabetes, hypothyroidism, or hypercalcemia—can slow digestive system motility and contribute to constipation.
- Gut Microbial Imbalance (Dysbiosis): CKD can impair the kidneys’ ability to filter toxins, including bacteria that affect intestinal balance. This leads to dysbiosis, an abnormal mix of gut bacteria often linked to constipation and increased production of harmful gut-derived toxins.
- Medication Side Effects: People living with CKD often take medications for anemia, bone health, hypertension, and other CKD-related complications. Drugs such as antihypertensives, iron supplements, calcium-based medications, and anti-nausea agents are notorious for causing or worsening constipation.
Table: Common Causes of Constipation in CKD Patients
| Cause | Description |
|---|---|
| Renal Diet | Reduced intake of fiber-rich foods due to dietary restrictions |
| Fluid Restrictions | Low fluid intake required for kidney health or dialysis |
| Co-occurring Conditions | Diabetes, hypothyroidism, hypercalcemia can slow digestion |
| Gut Dysbiosis | Imbalance of gut bacteria due to poor kidney filtration |
| Medications | Drugs for CKD complications may reduce gut motility |
Symptoms of Constipation and Kidney Disease
Constipation is not always a direct symptom of kidney failure; however, some digestive symptoms commonly occur with CKD. Early and advanced kidney disease can manifest as changes in bowel habits and other systemic signs:
- Digestive Symptoms: Loss of appetite, nausea, vomiting, diarrhea (sometimes bloody), bloating, and abdominal pain.
- Typical Signs of Constipation: Infrequent bowel movements, hard or dry stools, straining during bowel movements, abdominal discomfort.
- Other CKD-Associated Symptoms:
- Itchy or very pale skin
- Unexplained weakness or muscle cramps
- Bone pain
- Change in urine output (no urine or excessive urine)
- Unusual bleeding, nosebleeds
- Swelling throughout the body
- Stomach mass, back pain
- Bad breath or metallic taste in mouth
- Loss of appetite
- Difficulty hearing
Complications and Impact of Constipation on Kidney Health
Constipation has more consequences for people with CKD than simple discomfort. Chronic constipation can worsen kidney function by:
- Increasing gut-derived uremic toxins, which accumulate as renal function declines, fueling a negative cycle.
- Promoting gut dysbiosis and shifting metabolism toward increased protein breakdown in the colon.
- Elevating the risk for developing advanced CKD and accelerating the progression to end-stage renal disease (ESRD) requiring dialysis.
Researchers have found constipation is highly prevalent among CKD patients—up to 37% of patients transition from CKD to ESRD showing regular use of laxatives. Moreover, constipation itself may be a predictor of kidney function decline, making management critical for overall kidney health.
Treatments for Constipation in CKD and Kidney Failure
Treating constipation in people with kidney failure requires a multi-faceted approach. Not every remedy is appropriate, and consultation with a healthcare provider is essential. Treatments are generally divided into lifestyle modifications, dietary adjustments, and medication interventions.
Lifestyle and Dietary Solutions
- Increase Dietary Fiber: Fiber enhances stool bulk and promotes regularity. Safe sources for CKD patients include apples, pears, oats, beans, lentils, whole grains, and vegetables. Always consult with your dietitian to find kidney-safe options.
- Exercise: Physical activity stimulates digestion, boosts gut motility, and aids in constipation relief.
- Hydration: Within kidney guidelines, try to maximize allowed fluid intake for softer stools.
- Healthy Bowel Habits: Establish regular times for bowel movements and avoid delaying the urge to go.
Medication-Based Solutions
If lifestyle changes are ineffective, healthcare providers may recommend medications. Common treatments include:
- Laxatives: Certain types, like osmotic or bulk-forming laxatives, may be appropriate, but magnesium-containing products can be risky due to fluid imbalance or high magnesium levels. Always get approval from your nephrologist before starting any laxative.
- Guanylate Cyclase-C Agonists: Linaclotide and plecanatide are well-tolerated due to limited absorption, reducing risk for CKD patients.
- Lactulose and Lubiprostone: These act as stool softeners and also show reno-protective benefits, making them viable options.
- Sodium/Hydrogen Exchanger Inhibitors: Tenapanor decreases phosphate absorption and reduces sodium uptake, helping both constipation and hyperphosphatemia.
- Prokinetic Agents: Prucalopride can be prescribed at reduced dosages (1mg daily) for patients with kidney function below 30 mL/min.
Cautions for CKD Patients Using Laxatives
- Never self-prescribe a laxative without medical guidance.
- Laxatives may interact with kidney medications or exacerbate electrolyte imbalances.
- If symptoms persist or worsen, or if complications like severe abdominal pain or vomiting arise, seek immediate medical attention.
Alternative and Surgical Interventions
Most forms of constipation in CKD can be treated with conservative approaches. However, for severe, unresponsive cases, alternative options may be discussed:
- Biofeedback: Training and therapy to improve pelvic floor muscle function.
- Surgical Options: Rarely required, but may be considered in cases of obstructive or refractory constipation.
Frequently Asked Questions (FAQs)
Is constipation a symptom of kidney failure?
Constipation is not a classic symptom of kidney failure, but occurs frequently among CKD patients due to medications, dietary modification, co-occurring conditions, and fluid imbalance.
Why do kidney patients need a low-fiber diet?
Traditional CKD diets restricted fiber sources due to concerns over potassium and phosphorus, but newer guidelines are often less restrictive, permitting more fruits and vegetables in moderation.
Can I use over-the-counter laxatives if I have kidney disease?
Not safely—never take any laxative without your nephrologist’s approval. Some laxatives can cause dangerous fluid or electrolyte shifts; others may interact with your CKD medications.
What lifestyle changes help relieve constipation in CKD?
- Increase dietary fiber within kidney-friendly limits
- Exercise regularly
- Maintain regular bathroom habits
What should I do if constipation does not go away?
If constipation persists despite lifestyle and medication adjustments, consult your healthcare team to review your medications, check for underlying causes, and discuss advanced treatment options.
Key Takeaways
- CKD and kidney failure frequently lead to constipation due to diet, fluid restriction, medications, and secondary conditions.
- Effective management starts with lifestyle and dietary changes, progressing to medication under medical supervision if needed.
- Constipation may contribute to worsening kidney function; careful treatment protects digestive and renal health.
- Always consult your healthcare provider before starting any new treatment for constipation.
References
- Constipation in Patients With Chronic Kidney Disease (PMC)
- Kidney Failure Constipation: Causes and Treatments (Healthline)
- Relieving Constipation – AAKP
- Constipation in Patients With Chronic Kidney Disease (JNM)
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10577456/
- https://www.healthline.com/health/kidney-disease/kidney-failure-constipation
- https://aakp.org/relieving-constipation/
- https://www.jnmjournal.org/view.html?uid=1876&vmd=Full
- https://www.albertahealthservices.ca/assets/info/nutrition/if-nfs-tips-to-reduce-constipation-on-your-kidney-diet.pdf
- https://www.nhs.uk/conditions/kidney-disease/treatment/
- https://homedialysis.org/life-at-home/articles/constipation-on-dialysis
Read full bio of medha deb












