Kidney Ablation: Options, Procedures, Recovery, and Risks
A comprehensive guide to kidney ablation for small kidney tumors, including procedures, preparation, recovery, risks, and FAQs.
Kidney ablation is a minimally invasive treatment that uses extreme temperatures—either heat or cold—to destroy abnormal tissues, most commonly small kidney tumors. For people who are not ideal candidates for traditional kidney surgery or wish to preserve kidney function, ablation offers an effective alternative with faster recovery times and fewer complications. This guide covers all essential aspects of kidney ablation for kidney cancer and other conditions, including how the procedures work, who is eligible, what to expect, recovery details, risks, and frequently asked questions.
What is Kidney Ablation?
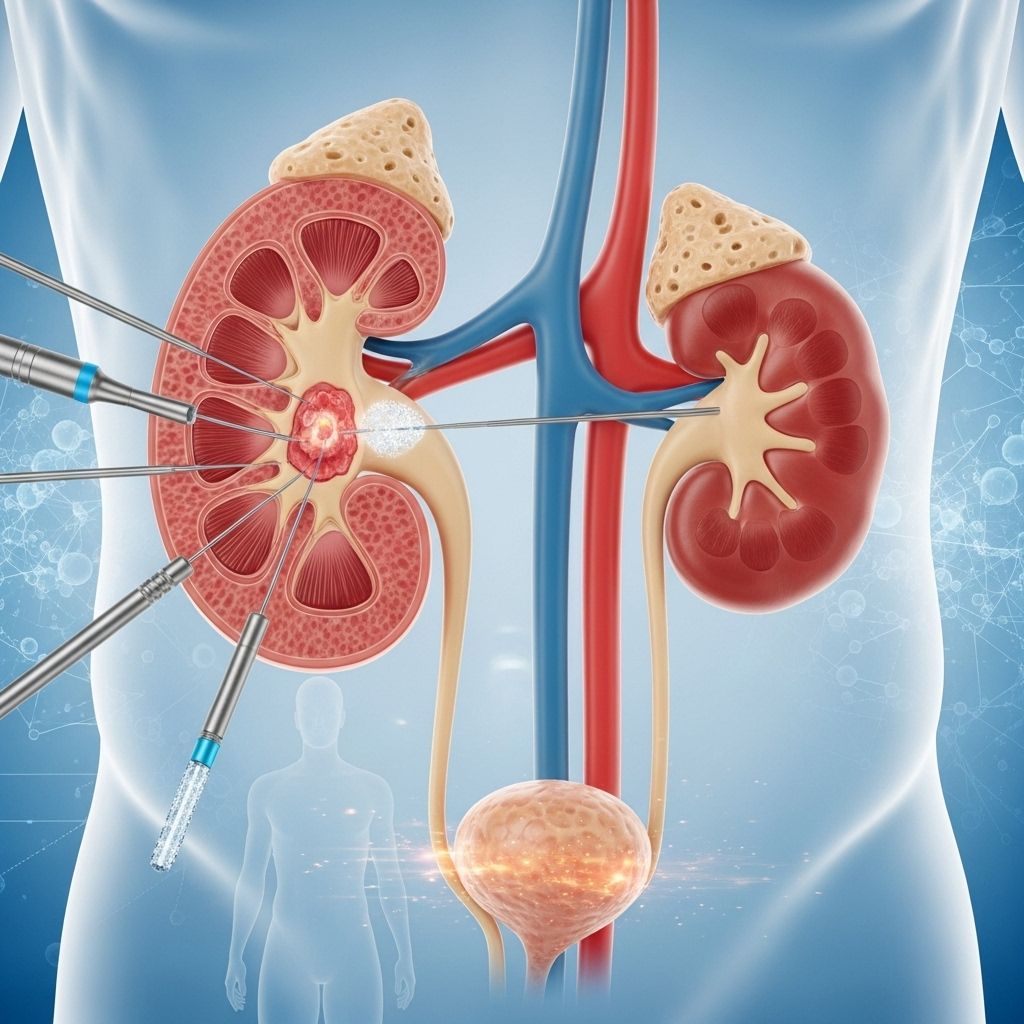
Kidney ablation, also called renal ablation or tumor ablation, refers to procedures that use targeted heat or cold to destroy kidney tumors and abnormal tissue. Unlike surgery, ablation typically does not require large incisions and can often be performed with needles (probes) inserted through the skin under image guidance.
Common reasons for considering kidney ablation include:
- Presence of a small kidney tumor (usually less than 4 cm in size)
- Need to preserve kidney function, especially if only one kidney is present
- Health conditions that make surgery risky or inadvisable
- Patient preference to avoid major surgery
Ablation may also be considered for individuals with inherited conditions causing multiple kidney tumors or when cancer affects both kidneys.
Types of Kidney Ablation Procedures
There are several methods of ablation used to treat kidney tumors. The procedure chosen depends on the size, location, and characteristics of the tumor, as well as patient health and medical history.
Cryoablation
Cryoablation uses extremely cold temperatures to freeze and kill tumor cells. During the procedure, a radiologist inserts a thin, needle-like probe (cryoprobe) directly into the tumor under imaging guidance. A special gas, commonly argon, is pumped into the probe to freeze the tissue. The freeze-thaw cycle may be repeated several times to ensure thorough destruction of abnormal cells. Cryoablation is most often used for kidney tumors close to the outer part of the kidney or for tumors in patients who cannot undergo surgery.
Radiofrequency Ablation (RFA)
Radiofrequency ablation (RFA) deploys highly focused electrical energy through a needle inserted directly into the tumor. This generates heat (often up to 80–100°C) that causes cellular death within the tumor and a small margin of surrounding tissue. RFA is a commonly used technique for small kidney cancers and is less likely to harm healthy nearby structures.
Other Ablation Techniques
- Microwave Ablation: Uses microwaves to quickly heat and destroy tumor cells, sometimes used in clinical trials or if other techniques are not suitable.
- Laser Ablation: Employs laser energy delivered via fiber-optic probes to destroy the tumor.
- High-Intensity Focused Ultrasound (HIFU): Non-invasively focuses intense ultrasound waves to ablate tissue deep inside the body. Still mainly experimental for kidney tumors.
- Radiation Ablation: Stereotactic or external radiation may be considered in select high-risk cases when needle-based ablation poses unacceptable risks.
Who is a Good Candidate for Kidney Ablation?
Ablation is most suitable for patients with the following characteristics:
- Small, localized kidney tumor (<4 cm or Stage I renal cell carcinoma)
- Not a candidate for partial nephrectomy (surgical removal of part of the kidney)
- Elderly patients or individuals with significant comorbidities that make surgery too risky
- Impaired kidney function or only one working kidney
- Tumors in locations accessible to ablation without high risk to surrounding organs
- Multiple tumors due to inherited syndromes or recurrent disease
| Criteria | Preferred Treatment |
|---|---|
| Tumor <4 cm, surgery not feasible | Ablation |
| Solitary kidney or poor kidney function | Ablation |
| Multiple tumors, inherited conditions | Ablation often considered |
| Tumor near center of kidney or large | Partial or total nephrectomy |
How to Prepare for Kidney Ablation
If you and your healthcare team decide that kidney ablation is appropriate, you will typically undergo preparation similar to that for other minor surgical procedures:
- Preoperative assessment: Includes blood tests, imaging, and medication review.
- Fasting: Most procedures require you to avoid eating or drinking for 6 to 12 hours beforehand.
- Medication adjustments: Some blood thinners or diabetes medications may need to be stopped or adjusted. Always inform your doctor of all medications and supplements you take.
- Consent and questions: You will be asked to sign consent forms and have the opportunity to ask questions about risks, benefits, and expected outcomes.
- Personal arrangements: Plan for time off work, transportation after the procedure, and supportive care at home, if needed.
What Happens During the Kidney Ablation Procedure?
The details of kidney ablation can vary based on the specific technique and individual patient needs, but most ablation procedures share common features:
- Location: Performed in a hospital or specialized outpatient facility, most often by an interventional radiologist or urologist trained in ablative therapies.
- Anesthesia: Procedures may require local anesthesia with sedatives or, in some cases, general anesthesia, depending on complexity and patient comfort.
- Imaging guidance: Continuous imaging (usually CT or ultrasound, and sometimes MRI) is used to accurately locate the tumor and guide probe placement.
- Probe insertion: After numbing the skin, one or more thin needle-like probes are inserted through the skin (percutaneously) or by keyhole (laparoscopic) surgery to reach the tumor.
- Ablation: The selected technology (cryo, radiofrequency, microwave, laser, or HIFU) is activated to freeze or heat the tumor, destroying the abnormal tissue along with a small margin of healthy tissue to ensure thorough treatment.
- Monitoring: Imaging ensures the correct area is ablated. Additional tumor samples (biopsies) may also be taken during the procedure for confirmation.
- Duration: Total time is typically 1–3 hours, including preparation and recovery; the ablation phase itself often lasts less than an hour.
Keyhole (Laparoscopic) Ablation
In some cases, ablation is performed using keyhole surgery. Here, small incisions are made to accommodate a laparoscope—a thin tube with a light and a camera—so surgeons can visualize and access tumors that are tricky to reach percutaneously. This approach is preferred for tumors deep within the kidney or near vital structures.
What to Expect After Kidney Ablation
Recovery after kidney ablation is usually quicker compared to traditional surgery. Here’s what you can typically expect:
- Pain and discomfort: Mild to moderate pain or soreness at the ablation site is common. This is usually well managed with oral pain medication and subsides within a few days.
- Hospital stay: Most patients can return home the same day or after an overnight observation.
- Activity: Gentle movement is encouraged as tolerated, but avoid strenuous exercise, heavy lifting, or swimming for up to two weeks or as advised.
- Follow-up visits: Imaging studies (like CT or MRI) are scheduled in the weeks to months after ablation to assess treatment success and monitor for recurrence.
- Urinary catheter: Some may be discharged with a temporary urinary catheter, usually removed within a day or two.
Risks and Complications of Kidney Ablation
While kidney ablation is generally safe, every procedure carries some risks. Potential complications include:
- Bleeding or hematoma at the ablation site
- Infection at the probe insertion site or surrounding tissues
- Damage to nearby structures (such as bowel, blood vessels, or ureter)
- Leakage of urine from the ablated area if the collecting system is injured
- Incomplete ablation requiring additional treatment sessions
- Small risk of kidney function decline
- Rare allergic reaction to medications or contrast dyes used in imaging
Most side effects are mild and temporary. Severe complications are uncommon, especially in experienced centers using image guidance.
Advantages and Limitations of Ablation for Kidney Tumors
| Advantages | Limitations |
|---|---|
| Minimally invasive; usually requires no large incision or only small keyhole ports | Slightly higher risk of incomplete treatment compared to surgical excision |
| Shorter hospital stays and recovery times | Not suitable for large or centrally located tumors |
| Often preserves kidney function | Long-term outcomes less certain than traditional surgery |
| Can be repeated if new or recurring tumors appear | Requires follow-up imaging to monitor for recurrence |
| Less pain and fewer complications than open surgery | May not remove all malignant tissue if tumor is irregular |
Frequently Asked Questions (FAQs) About Kidney Ablation
What is the success rate of kidney ablation?
For small kidney tumors (<4 cm), success rates for complete ablation are typically 85–95%. Success depends on tumor size, location, technique, and patient characteristics.
Does ablation cure kidney cancer?
Ablation can cure early-stage, localized kidney tumors when all cancerous cells are destroyed. However, ongoing monitoring is essential, as there is a risk of incomplete ablation or recurrence.
Is the procedure painful?
Most patients experience only mild to moderate discomfort during and after ablation, managed effectively with medication. Sedation or anesthesia is used during the procedure for comfort.
Will I need additional treatments?
Some patients may require repeat ablation if imaging reveals that the tumor was not fully destroyed after the first procedure. Further treatment is generally less invasive than an initial surgery.
How is kidney function affected?
Ablation is designed to spare as much healthy kidney tissue as possible. The impact on kidney function is usually minimal with proper candidate selection and care.
What is the difference between ablation and surgery?
Ablation is minimally invasive and often done percutaneously or through keyhole incisions, destroying tissue with heat or cold. Surgery (such as nephrectomy) involves removal of all or part of the kidney, with longer recovery and more significant risks, but with a lower risk of recurrence in some cases.
Who performs kidney ablation?
Typically, interventional radiologists (experts in imaging and minimally invasive therapies) or urologists with ablation experience perform these procedures, often in specialized cancer or kidney treatment centers.
How soon will I know if the procedure worked?
Follow-up imaging (such as MRI or CT scans) at one month, three months, and periodically thereafter are essential to confirm that the tumor is destroyed and detect any regrowth early.
Takeaway
Kidney ablation is an important treatment alternative to surgery for individuals with small kidney tumors who are not suitable for nephrectomy or wish to spare kidney tissue. With careful patient selection and expert care, ablation provides high rates of success and preserves quality of life. If you are considering kidney ablation, consult your healthcare provider to understand your options, potential benefits, and risks based on your unique situation.
References
- https://www.macmillan.org.uk/cancer-information-and-support/treatments-and-drugs/tumour-ablation-for-kidney-cancer
- https://www.urmc.rochester.edu/encyclopedia/content?contenttypeid=34&contentid=bkidt5
- https://cancerblog.mayoclinic.org/2024/03/26/treating-kidney-cancer-without-surgery/
- https://radiology.ucsf.edu/patient-care/services/kidney-tumor-ablation
- https://www.youtube.com/watch?v=lC_YLQ7upKc
- https://www.cancer.org/cancer/types/kidney-cancer/treating/ablation.html
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3126069/
- https://ajronline.org/doi/10.2214/AJR.15.14752
Read full bio of medha deb












