Thrombosis of the Inferior Vena Cava: Causes, Symptoms, Diagnosis, and Treatment
Explore the critical risks, symptoms, and treatments of IVC thrombosis to recognize warning signs and improve outcomes.
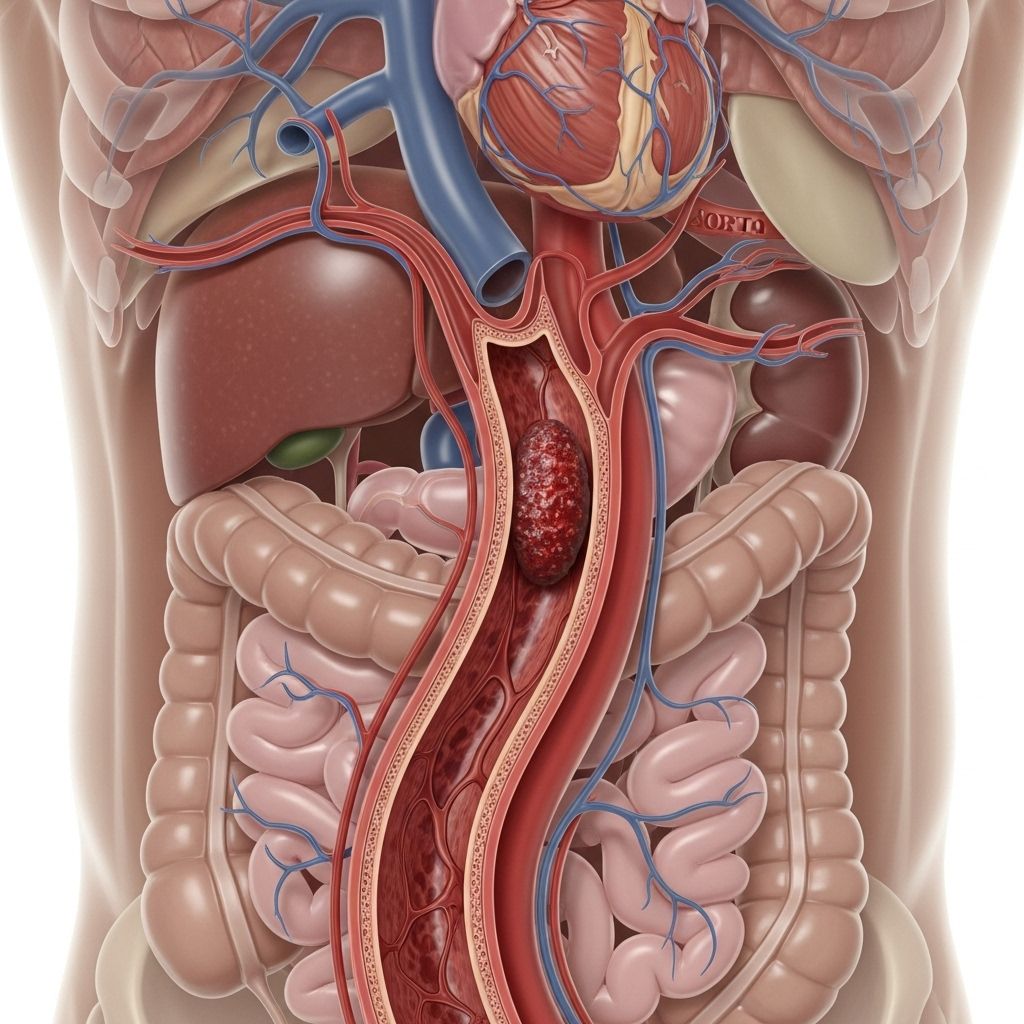
Thrombosis of the Inferior Vena Cava (IVC)
The inferior vena cava (IVC) is the largest vein in the body, responsible for carrying deoxygenated blood from the lower body back to the heart. IVC thrombosis refers to a blood clot (thrombus) forming within the IVC. This condition can be life-threatening and requires prompt detection and treatment to avoid severe health complications.
What Is IVC Thrombosis?
IVC thrombosis occurs when a blood clot develops and obstructs flow in the inferior vena cava. Because this vein is essential for returning lower body blood to the heart, a blockage here can result in major circulatory problems, and in some cases, can be fatal. Quick diagnosis and intervention are critical for optimal outcomes. The severity and effects of IVC thrombosis largely depend on the clot’s size, location, speed of formation, and underlying causes.
Symptoms of IVC Thrombosis
The symptoms of IVC thrombosis vary, influenced by where the clot forms and how much of the vein is obstructed. Some people may have mild symptoms, while others can develop serious or life-threatening complications.
- Leg pain or cramping: Usually in one or both legs, often sudden and unexplained.
- Swelling and heaviness: Especially in the legs, ankles, or feet, which may worsen with time.
- Skin discoloration: The skin over the legs may appear reddish, bluish, or darkened.
- Chronic ulcers: Non-healing sores or ulcers on the legs due to blood pooling, especially around the ankles.
- Abdominal or back pain: Discomfort or pain may occur above the occluded segment of the IVC.
- Swelling of the scrotum: This can occur in males due to blood backing up in veins draining the pelvis and groin.
- Shortness of breath, chest pain: These may result if the clot breaks loose and travels to the lungs, causing a potentially fatal blockage called pulmonary embolism.
Since many of these symptoms can mimic other health problems, a prompt, accurate diagnosis is crucial for effective management.
Causes and Risk Factors of IVC Thrombosis
IVC thrombosis can be caused by multiple factors, often related to disruptions in normal blood flow or increased blood clotting tendency. Recognizing risk factors and common triggers helps guide prevention and early detection.
- Inherited blood clotting disorders: Genetic mutations (e.g., Factor V Leiden, prothrombin gene mutation) can make you more prone to developing venous blood clots.
- Cancer: Malignancies, particularly abdominal or pelvic cancers (such as pancreatic cancer), can compress the IVC or increase clotting factors, raising the risk of thrombosis.
- IVC filter placement: These devices, used to prevent pulmonary embolism by catching clots from the legs, can themselves cause clot formation around the filter.
- Trauma or surgery: Injuries or surgical interventions, especially involving the abdomen, pelvis, or lower extremities, can cause direct injury to the IVC and promote thrombosis formation.
- Pregnancy and hormone therapy: Increases in clotting factors during pregnancy, postpartum, or during certain hormone replacement therapies can heighten risk.
- Long periods of immobility: Extended bed rest, long travel, paralysis, or post-surgical recovery can all slow blood flow and predispose to clot formation.
- Obesity: Excess body weight can increase pressure on veins and alter blood chemistry, raising the likelihood of thrombosis.
- Chronic illnesses: Conditions such as congestive heart failure, kidney disease, or liver disease create a pro-thrombotic state and sometimes promote sluggish blood flow.
Diagnosis of IVC Thrombosis
No single test definitively diagnoses IVC thrombosis. Doctors rely on clinical evaluation combined with a set of advanced imaging studies to confirm the presence, severity, and extent of the blood clot, and to detect any related complications.
- Catheter Venography: This imaging test involves injecting a contrast dye into the veins and then taking X-rays to visualize areas of blockage or narrowing.
- Computed Tomography (CT): CT scans provide detailed cross-sectional images of the abdomen and pelvis, often identifying IVC clots and any associated swelling or signs of inflammation.
- Magnetic Resonance Imaging (MRI): MRI can visualize soft tissues and blood vessels in detail and is often used when exposure to radiation or contrast dye is a concern.
- Ultrasound: Doppler ultrasound exams (particularly of the pelvis or lower limbs) can detect changes in blood flow and reveal the presence of a clot.
When an IVC clot is detected, doctors may also order additional imaging (such as CT pulmonary angiography) to look for clots that may have migrated to the lungs, causing a pulmonary embolism.
Treatment Options for IVC Thrombosis
Effective management of IVC thrombosis aims to dissolve or remove the clot, prevent its migration, and lower the risk of recurrence or complications. The choice of treatment depends on the location, size, chronicity of the clot, and the patient’s underlying health condition.
1. Medication
- Heparin: An injectable anticoagulant given initially to rapidly inhibit further blood clotting and lower the risk of clot extension.
- Anticoagulant therapy: Oral or injectable blood thinners such as warfarin, apixaban, or rivaroxaban are often used for prolonged periods to prevent new clots from forming.
Some patients may require ongoing blood thinning for life, especially if they have persistent risk factors or recurrent thrombosis.
2. Thrombectomy
Certain patients with large, obstructive clots may be candidates for thrombectomy, a minimally invasive procedure to physically remove or break up the clot. During a thrombectomy:
- A catheter is navigated to the IVC using image guidance.
- Special devices or suction mechanisms are used to withdraw the clot or break it apart for removal.
This approach can provide rapid relief of symptoms and quickly restore blood flow, particularly for extensive or recent clots that have not yet caused significant vein damage.
3. Percutaneous Transluminal Angioplasty with Stenting
In chronic cases (clots present longer than 28 days or recurring), a combination of angioplasty (using a balloon to widen the narrowed or blocked section of the IVC) and stenting (placing a tiny metal mesh tube to hold the vein open) may be offered. This approach is considered when IVC narrowing or chronic scarring prevents adequate blood flow.
4. Other Interventions
- Systemic Thrombolysis: Some patients may be candidates for powerful clot-dissolving medications (thrombolytics like urokinase or tPA), though these carry a risk of serious bleeding and are reserved for selected cases.
- Supportive Therapies: Compression stockings, leg elevation, and physical activity are often encouraged to reduce symptoms and lower recurrence risks.
Prognosis and Outlook for IVC Thrombosis
The outcome for people with IVC thrombosis emphasizes the importance of early recognition and customized care. Several factors affect recovery and long-term health:
- The underlying cause of the thrombosis (e.g., inherited condition vs. a complicating cancer) significantly impacts prognosis.
- Prompt initiation of anticoagulation and other medical treatments, along with individualized follow-up, improves outcomes.
- If untreated or complicated by other conditions (such as aggressive cancer), IVC thrombosis has a considerably higher mortality rate than lower-extremity DVT (deep vein thrombosis).
- Studies suggest the mortality risk for IVC thrombosis is about double that for standard DVT, with especially poor outcomes when associated with malignancy. Early treatment and management of underlying risks can improve prognosis.
Prevention of IVC Thrombosis
For those at risk or with a personal or family history of venous thrombosis, several proactive steps can be taken to help prevent IVC thrombosis:
- Consistent use of anticoagulation: For high-risk individuals, long-term blood thinners can help prevent new clot formation.
- Compression garments: Wearing compression stockings, especially during prolonged immobility (e.g., during airline travel or after surgery), can lower the risk of clots developing in the legs and traveling to the IVC.
- Healthy weight maintenance: Keeping a moderate weight can reduce vein pressure and the chance of thrombosis.
- Regular exercise: Physical activity improves blood flow and reduces the risk of clotting, especially for those who spend long periods sitting or lying down.
- Managing underlying conditions: Careful management of existing medical issues (like cancer, heart failure, or hormone disorders) with the help of a healthcare provider may lower risk.
- Avoiding unnecessary IVC filters: Because IVC filters themselves increase clot risk, their use should be carefully weighed against potential benefits and only used when strongly indicated.
Frequently Asked Questions (FAQs)
Is IVC Thrombosis Life Threatening?
Yes, IVC thrombosis can be fatal if untreated. The risk of death or serious complications is about double that of lower-limb DVT. However, with early detection and intervention, most people can be effectively treated and resume normal activities.
What Causes IVC Thrombosis?
Blood clots in the IVC are most commonly caused by inherited clotting disorders, cancer (especially abdominal), IVC filter devices, trauma, major surgery, hormone changes (pregnancy or replacement therapy), obesity, and prolonged immobility. Lifestyle and medical management can greatly reduce risks.
Can IVC Thrombosis Lead to Pulmonary Embolism?
Yes. If a clot or part of a clot in the IVC breaks free, it can travel through the heart and lodge in the arteries of the lungs, resulting in a dangerous, sometimes fatal, pulmonary embolism. This is why fast diagnosis and treatment are critical.
Can IVC Thrombosis Be Prevented?
- Anticoagulant therapy can be used in at-risk individuals to help prevent blood clot formation.
- Compression stockings, especially during long travel or immobility, lower risk in those with a history of venous clots.
- Maintaining a moderate weight, staying physically active, and managing underlying diseases can all help prevent IVC thrombosis.
- Discuss the necessity and risks of IVC filters before placement to determine if the benefits outweigh the risks.
Summary Table: Key Facts about IVC Thrombosis
| Aspect | Detail |
|---|---|
| What is it? | Blood clot in the inferior vena cava, impairing circulation. |
| Main symptoms | Leg swelling, pain, skin color changes, possible abdominal or back pain. |
| Diagnosis methods | Venography, CT, MRI, Ultrasound |
| Treatment options | Anticoagulants, thrombectomy, angioplasty/stenting, compression therapy |
| Primary risks | Genetic disorders, cancer, IVC filters, immobility, surgery, trauma, obesity |
| Outlook | Depends on underlying cause; risk of death higher than regular DVT |
When to Seek Medical Help
If you experience unexplained swelling, pain, or discoloration in your legs, or sudden shortness of breath or chest pain, seek immediate medical attention. Early evaluation can be life-saving, especially when IVC thrombosis or other clot-related events are suspected.
References and Resources
- Consult your primary healthcare provider or a vascular specialist for individual risk assessment and advice on preventing or managing blood clots.
- For general information, visit reputable resources such as the American Heart Association and the Centers for Disease Control and Prevention (CDC).
References
- https://www.healthline.com/health/heart-health/thrombosis-ivc
- https://journals.sagepub.com/doi/10.1177/1358863X12471967
- https://www.healthline.com/health/thrombosis
- https://www.ncbi.nlm.nih.gov/books/NBK537175/
- https://www.medicalnewstoday.com/articles/thrombosis
- https://pmc.ncbi.nlm.nih.gov/articles/PMC2293317/
- https://www.medicalnewstoday.com/articles/153704
- https://capriniriskscore.org/news/what-are-common-deep-vein-thrombosis-treatments-high-level-overview/
Read full bio of Sneha Tete












