Is IBS an Autoimmune Disease? Examining the Link Between IBS and Immune Disorders
Unraveling the complex relationship between irritable bowel syndrome (IBS) and autoimmune processes, with insights on causes, diagnosis, and treatment.
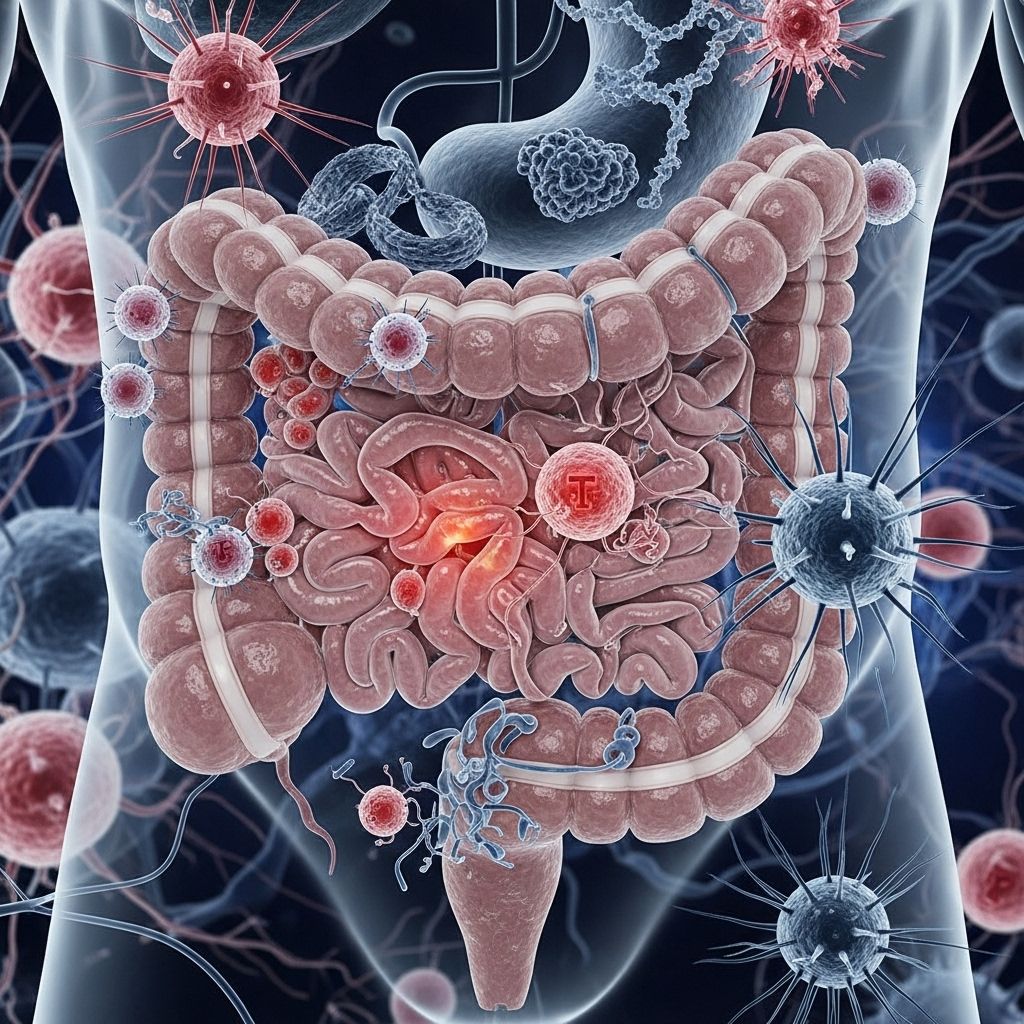
Is IBS an Autoimmune Disease? Understanding the Immune Connection
Irritable bowel syndrome (IBS) is one of the most common gastrointestinal disorders, affecting millions of people worldwide. While the symptoms can be persistent and significantly impact daily life, the underlying causes of IBS are still under active investigation. A recurring question from patients and researchers alike is: Is IBS an autoimmune disease? In this in-depth article, we’ll explore the current understanding of IBS, analyze the evidence surrounding autoimmune involvement, and clarify how IBS compares to true autoimmune conditions like Crohn’s disease and ulcerative colitis.
What is IBS?
Irritable bowel syndrome (IBS) is a functional gastrointestinal disorder characterized by symptoms such as:
- Abdominal pain or discomfort
- Bloating and gas
- Changes in bowel habits (diarrhea, constipation, or both)
- Urgency or incomplete evacuation after a bowel movement
Unlike some digestive conditions, IBS does not cause visible inflammation or structural abnormalities detectable by standard medical imaging or endoscopy. The symptoms are real and can be debilitating, but for years, doctors classified IBS as a “diagnosis of exclusion”—a condition identified after ruling out other clear-cut causes.
Is IBS an Autoimmune Disease?
Autoimmune diseases occur when the immune system mistakenly targets and attacks healthy tissues in the body. Inflammatory bowel diseases (IBD) such as Crohn’s disease and ulcerative colitis are classic examples of autoimmune or immune-mediated conditions of the gut. However, the situation with IBS is much more nuanced.
- IBS is not classified as an autoimmune disease.
- The primary difference: IBS lacks the characteristic tissue inflammation and direct immune-mediated destruction seen in classic autoimmune diseases.
However, recent research suggests that the immune system may play a role in the development or persistence of IBS symptoms in some individuals. This connection is complex, situating IBS between pure functional disorders and overt autoimmune conditions.
How Does the Immune System Affect IBS?
Over the past two decades, a growing body of research has highlighted various ways the immune system might be involved in IBS. Rather than an autoimmune response, some studies point to a phenomenon known as immune activation or immune dysregulation:
- Post-infectious IBS (PI-IBS): Many people report the onset of IBS symptoms after a significant gastrointestinal infection or food poisoning. These cases often show lingering low-grade inflammation or altered gut immunity.
- Lymphocyte Infiltration: Biopsies from IBS patients (especially those with diarrhea-predominant IBS, or IBS-D) have revealed increased numbers of certain immune cells (e.g., T cells, mast cells) in the colon and gut mucosa compared to healthy controls.
- Proinflammatory Cytokines: Elevated levels of immune signaling molecules, such as TNF-α, IL-1β, and IL-6, have been found in the blood and tissues of some IBS patients.
- Humoral Immunity: There is evidence of increased immunoglobulin (antibody) production, which may contribute to gut dysfunction and symptoms in some people.
Despite these findings, the immune changes observed in IBS tend to be subtle compared to the robust inflammation typical of Crohn’s disease and ulcerative colitis. There is also variability among patients—some show signs of immune involvement while others do not.
Autoantibodies and IBS: A Complex Picture
Autoantibodies are antibodies that mistakenly target the body’s own proteins, often playing a role in autoimmune diseases. Recent studies have detected various autoantibodies in a fraction of IBS patients. Some of these include:
- Antibodies to celiac disease-associated antigens
- Anti-CdtB and anti-vinculin (implicated in post-infectious IBS and potentially affecting nerve function in the gut)
- Anti-neuronal antibodies (may contribute to gastrointestinal motility problems)
However, no single autoantibody is consistently present in all IBS patients, and their significance remains controversial. Most researchers believe that, unlike in classic autoimmune diseases, autoantibodies are not the main driver in IBS but may contribute to symptoms in some subgroups.
Immune Activation vs. Autoimmunity: Key Distinctions
| Feature | IBS | Autoimmune Disease (e.g., Crohn’s, UC) |
|---|---|---|
| Primary cause | Multifactorial (gut-brain axis, microbiome, stress, minor immune changes) | Immune system attacks self-tissue |
| Visible inflammation | Rare/minimal | Prominent and persistent |
| Structural damage on biopsy | Absent or very mild | Present (ulcers, tissue destruction, granulomas) |
| Autoantibodies | Occasionally present, not disease-defining | Often present and diagnostic |
| Treatment response | Diet, stress management, gut-directed therapies | Immunosuppressive or biologic therapy |
Can IBS Turn Into an Autoimmune Disease?
There is no evidence that having IBS increases a person’s risk of developing an autoimmune disease, such as Crohn’s disease or ulcerative colitis. While some symptoms, like abdominal pain and bowel changes, may overlap, these are distinct conditions with different underlying mechanisms and treatments.
IBS itself is not a precursor to autoimmune disease, though both may have links to changes in the gut microbiome, chronic stress, or genetic predisposition. It’s also possible for someone to have both an autoimmune disease and IBS, but one does not directly cause the other.
Why Do People Confuse IBS With Autoimmune Diseases?
The confusion often arises because:
- The gut immune system appears to be overactive in both IBS and autoimmune diseases, though the degree and nature of activation differ.
- Both IBS and autoimmune bowel diseases (IBD) can cause similar digestive symptoms, such as pain, diarrhea, and urgency.
- Some research has found autoantibodies or immune cell changes in subsets of IBS patients.
However, it is crucial to distinguish these conditions, since treatment plans, prognosis, and required medical monitoring can vary widely.
Other Theories About What Causes IBS
While the role of the immune system has gained attention, it’s only one piece of the puzzle. Additional factors implicated in IBS include:
- Visceral hypersensitivity: Increased sensitivity of the nerves in the gut, leading to pain from normal digestive processes.
- Altered motility: Abnormal contraction of gastrointestinal muscles causes diarrhea, constipation, or fluctuating symptoms.
- The gut-brain axis: Psychological stress, anxiety, or depression can influence gut function and symptom severity.
- Gut microbiome: Imbalances in intestinal bacteria may contribute to or worsen IBS. Some studies have connected small intestinal bacterial overgrowth (SIBO) to IBS symptoms.
- Food sensitivities: Some people with IBS have immune responses to certain foods, particularly those high in certain carbohydrates (FODMAPs) or fermentable sugars. However, elevated food-specific antibodies may reflect dietary exposure rather than a true allergic or autoimmune response.
Diagnosing IBS vs. Autoimmune Digestive Disorders
Diagnosis of IBS typically involves assessing symptoms, reviewing medical history, and ruling out other causes. Diagnostic criteria—such as the Rome IV—focus on patterns of abdominal pain with bowel changes for at least six months. There are no definitive blood tests or biomarkers for IBS.
In comparison, autoimmune bowel diseases usually present with laboratory findings and imaging showing inflammation, tissue damage, and elevated specific antibodies. Blood tests, stool samples, colonoscopy, and biopsies are often required to confirm the diagnosis and rule out other serious conditions.
Treatment Approaches: IBS and Immune-Involved Gut Disorders
Because IBS is not considered an autoimmune disease, standard treatments focus on:
- Dietary modifications (e.g., low-FODMAP diet, elimination diet for specific sensitivities)
- Stress management (mindfulness, cognitive behavioral therapy)
- Medications targeting symptoms (antispasmodics, laxatives, anti-diarrheals, some antidepressants)
- Gut-directed therapies (probiotics, fiber supplements)
For autoimmune bowel diseases, treatment may include:
- Anti-inflammatory drugs (such as corticosteroids)
- Immunosuppressive medications
- Biologic drugs targeting inflammatory molecules
- In some cases, surgery
Frequently Asked Questions (FAQs)
Q: Is IBS a form of autoimmune disease?
A: No, IBS is not considered an autoimmune disease. While some immune involvement is observed in certain IBS patients, the condition lacks the pronounced immune attack on healthy tissue seen in classic autoimmune diseases.
Q: Does IBS cause immune deficiency or raise the risk of other autoimmune diseases?
A: Research does not support an increased risk of immune deficiency or future autoimmune disease for people with IBS.
Q: Could symptoms of autoimmune bowel diseases be misdiagnosed as IBS?
A: Yes, especially early on when inflammation may not be severe, IBD symptoms can resemble those of IBS. However, further testing usually clarifies the diagnosis.
Q: Can stress cause IBS or autoimmune diseases?
A: Chronic psychological stress is a recognized trigger for IBS symptoms and may change immune responses, but it is not directly considered a cause of autoimmune diseases. Stress management is beneficial in IBS therapy.
Q: Are there biomarkers available to diagnose IBS as an autoimmune disorder?
A: No, although certain autoantibodies (like anti-CdtB and anti-vinculin) have been studied, they are not exclusive to IBS and are not used for diagnosis at this time.
Takeaway: IBS and Autoimmunity
Although IBS shares some overlapping immune features with autoimmune disorders, current evidence indicates that it is not an autoimmune disease. Subtle immune activation and post-infectious changes may play roles in some cases, but the absence of significant tissue destruction and inflammation sets IBS apart from conditions like Crohn’s disease and ulcerative colitis. Individuals with IBS should work closely with their healthcare providers to create effective management plans, focusing on diet, symptom relief, and overall gut health.
References
- https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2024.1359003/full
- https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2020.00468/full
- https://pubmed.ncbi.nlm.nih.gov/20479895/
- https://health.clevelandclinic.org/ibd-vs-ibs
- https://nyulangone.org/conditions/irritable-bowel-syndrome/diagnosis
Read full bio of Sneha Tete












