Is Diabetic Retinopathy Reversible? Causes, Treatments, and Prevention
Understand if diabetic retinopathy can be reversed, current treatments, and effective prevention strategies to preserve your vision.
Diabetic retinopathy is a leading cause of vision loss among adults, especially for those living with diabetes. It develops as a result of prolonged high blood sugar levels damaging the blood vessels in the retina—the light-sensitive tissue at the back of the eye responsible for vision. Given the risks, many individuals are eager to know: Is diabetic retinopathy reversible? This article explores whether reversal is possible, reviews available treatment options, outlines prevention strategies, and addresses commonly asked questions.
What Is Diabetic Retinopathy?
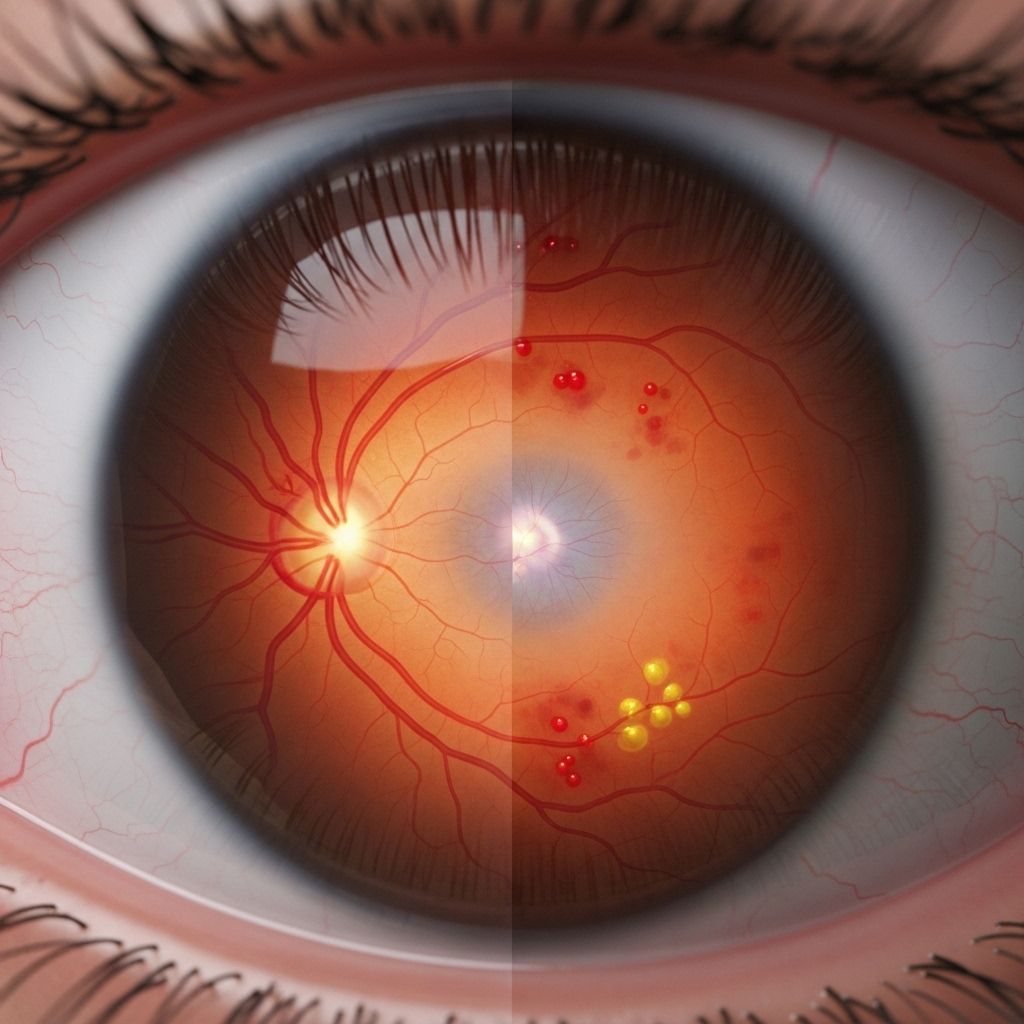
Diabetic retinopathy is a complication of both type 1 and type 2 diabetes mellitus. Chronically high blood sugar levels damage the small blood vessels in the retina. Over time, these vessels can leak fluid, bleed, or grow abnormally, impairing vision and potentially leading to blindness if not appropriately managed.
- Nonproliferative diabetic retinopathy (NPDR): Early stage marked by blood vessel weakening, microaneurysms, and occasional leakage.
- Proliferative diabetic retinopathy (PDR): Later stage where abnormal new blood vessels form and may bleed into the vitreous (the gel inside the eye), increasing risk of scarring and retinal detachment.
Symptoms of Diabetic Retinopathy
- Blurred or distorted vision
- Floaters (dark spots or strings in your vision)
- Difficulty seeing at night
- Sudden vision loss (advanced stages)
In early stages, symptoms can be subtle or absent, making regular eye exams crucial for people with diabetes.
Can Diabetic Retinopathy Be Reversed?
The answer is complex and depends on the stage of the disease. While some complications can be managed or even reversed if caught early, advanced diabetic retinopathy is generally not fully reversible.*
- Early Stages: Damage may be stabilized, and vision sometimes improves with prompt blood sugar control and appropriate therapy. In mild cases, strict management of blood sugar, blood pressure, and cholesterol levels can halt or sometimes reverse swelling and minor bleeding.
- Advanced Stages: Once significant retinal damage or vision loss occurs—particularly after the development of abnormal new blood vessels or scar tissue—full reversal is unlikely, although treatments may preserve remaining vision and resolve complications.
- Type of Diabetes Matters: There is some evidence that very early retinopathy in type 1 diabetes may improve with consistent, rigorous blood sugar control, but in type 2 diabetes, reversal is less likely.*
Note: Even if the disease cannot be “cured,” active treatments and healthy lifestyle changes can stop or substantially slow its progression, protecting vision over the long term.
Causes and Risk Factors
The primary cause of diabetic retinopathy is prolonged high blood glucose (hyperglycemia). Several additional risk factors can influence onset or severity:
- Long duration of diabetes (risk increases with years since diagnosis)
- Poor glycemic control (consistently high A1C levels)
- High blood pressure (hypertension)
- High cholesterol levels
- Smoking
- Kidney disease
- Pregnancy (can accelerate retinopathy)
Treatments for Diabetic Retinopathy
Treatment depends on the stage and specific complications present. Early detection and ongoing management are critical for the best outcomes.
Common Treatments for Diabetic Retinopathy
- Medication (Anti-VEGF Injections): Medications such as anti-VEGF agents are injected directly into the eye to reduce swelling and inhibit growth of abnormal blood vessels. These injections can halt or reverse some vision changes, especially for individuals with diabetic macular edema.
- Laser Therapy (Photocoagulation): Laser photocoagulation seals leaking blood vessels and shrinks abnormal new vessels. While it does not restore lost vision, it can prevent further deterioration.
- Vitrectomy Surgery: For advanced cases with bleeding (vitreous hemorrhage) or scar tissue, vitrectomy surgery may be needed to remove blood from the vitreous and repair retinal detachment, potentially improving vision.
- Cataract Surgery: Diabetic eye disease increases the risk of early cataracts. While surgery can restore clear vision by removing the cloudy lens, it does not reverse retinopathy itself.
Effectiveness of Treatments
| Treatment | Primary Goal | Stage Most Effective | Potential for Vision Improvement |
|---|---|---|---|
| Anti-VEGF Injections | Stop abnormal blood vessel growth & reduce swelling | Mild to moderate, macular edema | Moderate (can reverse some blurring) |
| Laser Photocoagulation | Seal leaky vessels, prevent further bleeding | Moderate to advanced | Low (prevents worsening, stabilizes) |
| Vitrectomy | Remove blood, repair retina | Severe, with hemorrhage or scarring | Possible (can restore some vision) |
| Cataract Surgery | Restore lens clarity | Any, if cataract present | High (for cataract, not for retinopathy itself) |
Lifestyle Management
For all stages, managing diabetes with lifestyle adjustments is essential:
- Blood sugar control: Target an A1C (average three-month blood sugar) as recommended by your healthcare provider. Even small improvements can slow progression.
- Healthy diet: Emphasize vegetables, whole grains, lean proteins. Limit processed foods and sugary drinks.
- Regular exercise: Aim for at least 150 minutes of moderate activity per week, tailored as advised.
- Monitor blood pressure and cholesterol: Both strongly influence the risk of eye complications.
- Avoid smoking: Smoking increases the risk of blood vessel damage.
Prevention: Protecting Your Eyesight
The best way to preserve vision is through preventive strategies and early disease detection:
- Annual dilated eye exams: Early detection of changes allows for prompt treatment before vision is affected.
- Strict blood glucose monitoring: Maintaining targets drastically cuts the risk of retinopathy.
- Controlling blood pressure: Reduces strain on the retinal vessels.
- Managing cholesterol: Lowers risk of vessel leakage and further complications.
- Healthy lifestyle overall: Regular exercise, healthy eating, quitting smoking, and managing body weight all reduce your risk.
Frequently Asked Questions (FAQs)
Can diabetic retinopathy be reversed after vision loss?
Once substantial vision loss or retinal damage has occurred, complete reversal is not possible. Early cases might be stabilized or modestly improved with lifestyle changes and prompt treatment, but advanced stages are not fully reversible. However, current therapies can halt worsening, resolve some complications, and in some cases modestly improve vision.
What treatments can help reverse symptoms?
Anti-VEGF injections and laser therapy can address swelling and abnormal blood vessel growth, sometimes improving blurry vision. Vitrectomy surgery may help when there is significant bleeding or scar tissue.
Does diet play a role in slowing or reversing retinopathy?
While diet alone cannot reverse established disease, healthy nutrition is essential for stabilizing blood sugar and blood pressure, thereby preventing progression and possibly improving early symptoms. Emphasize complex carbohydrates, fiber-rich foods, fresh vegetables, and lean proteins, and avoid excessive sugar and processed foods.
Is diabetic retinopathy always present in both eyes?
Yes, the condition typically develops in both eyes, but severity may differ from one eye to the other.
How often should people with diabetes get eye exams?
At least once a year, or more frequently if recommended by your eye care specialist. Early detection through exams is key for the best outcomes.
Are there future cures or new treatments on the horizon?
Ongoing research seeks new therapies, including improved drugs and regenerative medicine approaches. While promising, as of now, established treatments and prevention remain the primary defense against vision loss.
When to See a Doctor
Schedule an immediate appointment with an ophthalmologist or retinal specialist if you experience:
- Suden vision changes
- Floaters, flashing lights, or spots in your vision
- Blurring or difficulty seeing at night
- Pain or pressure in the eyes
Annual comprehensive eye exams are essential for all people with diabetes, even if no symptoms are present.
Summary: Key Takeaways
- Diabetic retinopathy is a serious eye complication of diabetes that can lead to vision loss if not properly managed.
- Complete reversal is generally not possible, but early intervention and aggressive management can preserve sight and, in some cases, improve symptoms.
- Controlling blood sugar, blood pressure, and cholesterol, avoiding smoking, regular eye exams, and following treatment plans are critical steps in preventing progression.
- Advancements in treatment offer hope, but prevention and early detection remain the most effective strategies for long-term vision health in people with diabetes.
References
- https://neoretina.com/blog/diabetic-retinopathy-can-it-be-reversed/
- https://www.floridaeyespecialists.com/blog/2024/11/can-diabetic-retinopathy-be-reversed/
- https://www.eyesurgeonsofindiana.com/can-diabetic-retinopathy-be-reversed/
- https://www.medicalnewstoday.com/articles/reversing-diabetic-retinopathy
- https://www.diabetes.org.uk/about-us/news-and-views/research-reveals-new-routes-reverse-retinopathy
- https://pubmed.ncbi.nlm.nih.gov/38718792/
- https://www.nhs.uk/conditions/diabetic-retinopathy/
- https://stanfordhealthcare.org/medical-conditions/eyes-and-vision/diabetic-retinopathy/treatments.html
Read full bio of Sneha Tete












