Understanding Iritis: Causes, Symptoms, Diagnosis, and Treatment
Learn the warning signs, triggers, diagnosis process, and effective treatments for iritis to protect your vision and eye health.
Iritis: An In-Depth Guide
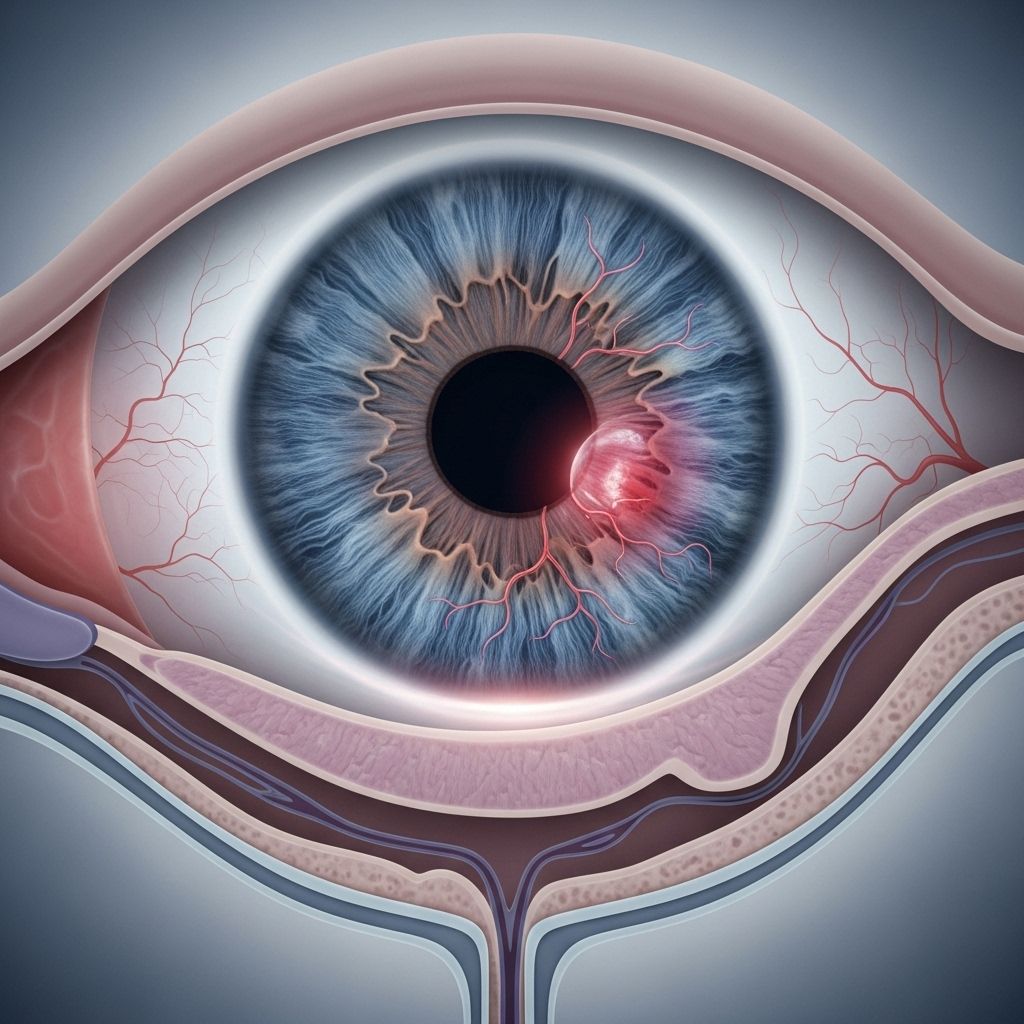
Iritis, also known as anterior uveitis, is a form of eye inflammation that specifically affects the iris—the colored ring around your pupil at the front of your eye. As one of the most common causes of eye pain and vision problems, iritis is potentially serious and warrants prompt attention. This guide breaks down the essential aspects of iritis, including causes, symptoms, risk factors, diagnostic steps, complications, treatments, and frequently asked questions.
What Is Iritis?
The iris plays a critical role in controlling the amount of light entering your eye by adjusting the size of the pupil. When the iris becomes inflamed and swollen, the condition is termed iritis. The iris is a key component of the uvea—the middle layer of the eye—which is why iritis is sometimes classified as anterior uveitis.
Iritis can be acute (beginning suddenly and resolving with treatment), chronic (lasting for months or even years), or recurrent (experiencing repeated episodes over time).
Key Causes of Iritis
Pinpointing the exact cause of iritis is not always possible; in fact, more than 30% of iritis cases are deemed idiopathic, meaning no specific cause can be identified. However, several conditions and triggers have been linked to iritis:
- Infections: Both viral (e.g., herpes simplex, herpes zoster), bacterial (e.g., Lyme disease, tuberculosis, syphilis), fungal, and even parasitic infections can trigger iritis.
- Autoimmune Diseases: Conditions where the body’s immune system attacks itself can inadvertently target the eye. Examples include rheumatoid arthritis, multiple sclerosis, inflammatory bowel disease (Crohn’s, ulcerative colitis), sarcoidosis, lupus, and ankylosing spondylitis.
- Genetic Factors: Certain genetic mutations (e.g., HLA-B27) are linked to increased risk of iritis, particularly in individuals with autoimmune conditions.
- Juvenile Idiopathic Arthritis (JIA): Especially common in children, JIA is a frequent underlying cause and may result in symptomless eye inflammation until vision is already affected.
- Trauma to the Eye: Physical injury, such as a corneal abrasion or improper contact lens use, can lead to inflammation of the iris.
- Cancer: Rarely, intraocular cancers like lymphoma can be the trigger.
- Behçet’s Disease: A rare disorder causing systemic inflammation, including in the eyes, joints, and mouth.
- Other Medical Conditions: Leukemia, Kawasaki syndrome, and nephritis may also be associated.
It is important to note that stress has not been shown to directly cause iritis, although it may contribute to triggering an episode in susceptible individuals.
Symptoms: How to Recognize Iritis
Iritis symptoms often begin abruptly and are usually noticeable due to their impact on vision and comfort. Typical signs include:
- Eye pain: Often described as aching, especially around the iris.
- Redness: Pronounced particularly around the iris, distinct from general conjunctivitis.
- Light sensitivity (photophobia): Discomfort in bright conditions, sometimes causing squinting or avoiding light.
- Blurred or cloudy vision: Making it difficult to see clearly.
- Tearing: Increased lacrimation is common.
- Decreased vision: Ranging from mild to severe impairment.
- Headache: May accompany eye pain.
- Irregular-shaped pupil: Less commonly seen, often the result of adhesions (synechiae).
Symptoms can emerge in one eye, both eyes, or alternate between eyes with recurring attacks. Chronic iritis may cause fewer symptoms but pose greater long-term risks for vision loss.
Risk Factors and Who Gets Iritis?
Anyone can develop iritis, but certain groups have higher risk:
- Individuals with autoimmune diseases or a family history of autoimmune disorders.
- Children with juvenile idiopathic arthritis (JIA), particularly young girls.
- People with genetic markers such as HLA-B27.
- Those who have recently suffered eye trauma or surgery.
- Individuals with specific infections affecting other parts of the body.
For children, iritis may go undetected since symptoms can be minimal. Routine screening is vital for at-risk populations, such as those diagnosed with JIA or other inflammatory conditions.
Diagnosis: How Iritis Is Identified
Early and accurate diagnosis is crucial to prevent complications and vision loss. If iritis is suspected, an eye care professional—typically an ophthalmologist—will undertake several steps:
- Medical history: Discuss symptoms, recent illnesses, trauma, medications, and family medical history.
- Physical examination: Using a slit lamp microscope, the eye specialist inspects the anterior chamber for signs of inflammation. White blood cells may be visible in this area, and signs such as iris swelling, redness, or abnormal pupil shape are noted.
- Vision tests: Visual acuity and eye pressure assessments help determine the impact of inflammation.
- Pupil dilation: Enables a closer look at the back of the eye to rule out other conditions.
- Screening for systemic diseases: If an underlying cause is suspected, additional tests—including blood work, CT or MRI imaging, urine tests, or fluid sampling—may be performed.
- Cultures: In rare cases, samples from eyelid, cornea, or intraocular fluid may be taken to identify infection.
Iritis may present in only one eye, both eyes, or repeatedly in the same eye. Recurrent or bilateral iritis often prompts further systemic evaluation to identify underlying causes.
Complications of Untreated Iritis
Iritis is not only uncomfortable—it can also have serious consequences. If untreated or undertreated, it can progress and damage vital structures in the eye. Significant complications include:
- Permanent vision loss or blindness: Iritis contributes to approximately 30,000 cases of blindness annually.
- Macular edema: Swelling of the retina, leading to central vision impairment.
- Synechiae: Abnormal adhesions between the iris and lens, which can distort pupil shape and impede eye function.
- Retinitis: Inflammation spreading to the retina, affecting vision.
- Cataracts: Clouding of the eye’s lens, often accelerated by chronic inflammation.
- Glaucoma: Increased eye pressure, which can further threaten vision.
Prompt consultation with an eye doctor is recommended if you notice any new or persistent vision changes, pain, or redness. The longer iritis remains untreated, the greater the risk of lasting complications.
Treatment Options for Iritis
Most cases of iritis respond well to prompt, appropriate treatment. The primary goals are to relieve symptoms, reduce inflammation, prevent complications, and address any underlying causes. Treatment is tailored according to severity and cause, but commonly includes:
- Corticosteroid eye drops: The mainstay of iritis therapy, they rapidly reduce inflammation and pain.
- Pupil-dilating drops (mydriatics): Relax the iris, reduce pain from light sensitivity, and prevent synechiae formation.
- Oral or injected corticosteroids: Reserved for severe cases and iritis that does not respond to topical treatment.
- Treatment of underlying cause: If infection or systemic disease is found, specific therapy such as antibiotics, antivirals, immunosuppressants, or other targeted medications are used.
- Pain relievers: May be prescribed to improve comfort.
Regular follow-up appointments are critical to monitor response to treatment, prevent relapse, and modify medications as needed. Treatment duration varies but may span weeks to months depending on the type and recurrence of iritis.
Self-Care and Prevention Tips
- Follow your eye specialist’s instructions: Take all prescribed medications as directed and always attend scheduled check-ups.
- Manage underlying health conditions: Keep autoimmune diseases or infections under control with help from your doctor.
- Protect your eyes: Use eye protection to prevent traumatic injury and avoid contact lens-related problems.
- Avoid triggers: Discuss with your provider any known allergies or factors that have previously triggered iritis.
Prognosis
With early attention and appropriate management, most people with iritis recover fully without permanent vision loss. Chronic or recurrent cases require ongoing care to prevent complications.
Frequently Asked Questions (FAQs) About Iritis
What is the difference between iritis and uveitis?
Iritis refers to inflammation of only the iris, the colored part of the eye. Uveitis encompasses inflammation of any part of the uvea, including the iris (iritis), ciliary body (intermediate uveitis), and choroid (posterior uveitis).
Can iritis affect both eyes?
Yes, iritis can affect only one eye or both eyes. Bilateral involvement is more likely in cases linked to an underlying systemic condition.
What is the prognosis if iritis is untreated?
Untreated iritis can lead to sight-threatening complications, such as chronic pain, glaucoma, cataracts, retinal swelling, and even blindness.
Is iritis contagious?
No, iritis itself is not contagious. However, underlying infections (such as herpes viruses) may be transmissible through direct or indirect contact.
Can children develop iritis?
Yes, iritis can occur in children. Juvenile idiopathic arthritis is a leading cause. Children may not report symptoms, so regular eye exams are necessary for those at risk.
How quickly do iritis symptoms develop?
Iritis generally has a rapid onset, often developing over hours or days. Acute cases may resolve with prompt treatment, while chronic forms are slower to heal and may require long-term therapy.
Is there a cure for iritis?
While most cases can be controlled and symptoms alleviated, recurrent or chronic forms may require lifelong management to prevent or limit complications.
Table: Common Causes of Iritis
| Cause | Description |
|---|---|
| Autoimmune Disease | Body’s immune system attacks the eye (e.g., rheumatoid arthritis, lupus, sarcoidosis) |
| Infection | Bacterial, viral, fungal, or parasitic pathogens |
| Genetic Markers | HLA-B27 gene association, increases risk alongside autoimmune conditions |
| Trauma | Injury to the eye, including surgery or corneal abrasion |
| Cancer | Lymphoma or other intraocular tumors |
| Idiopathic | No identifiable cause; common in many cases |
When to See an Eye Doctor
Immediate evaluation by an eye specialist is essential if you experience:
- Sudden or severe eye pain
- Loss of vision
- Extreme light sensitivity
- Red eye that does not resolve
- History of autoimmune disease or recent trauma
Early treatment maximizes the likelihood of complete recovery and minimizes risk of complications.
Summary
Iritis is a potentially serious inflammation of the iris that can develop quickly and result in significant discomfort and vision issues. Causes range from infections and autoimmune conditions to trauma and idiopathic origins. Given the risk of long-term complications and vision loss, early recognition, diagnosis, and treatment by an eye care professional are vital. With prompt care, most people make a full recovery and can successfully manage or even prevent recurrent episodes.
References
Read full bio of medha deb












