Intraventricular Hemorrhage: Causes, Symptoms, and Care
Comprehensive guide to intraventricular hemorrhage, exploring causes, symptoms, diagnosis, treatment, and long-term outlook for patients.
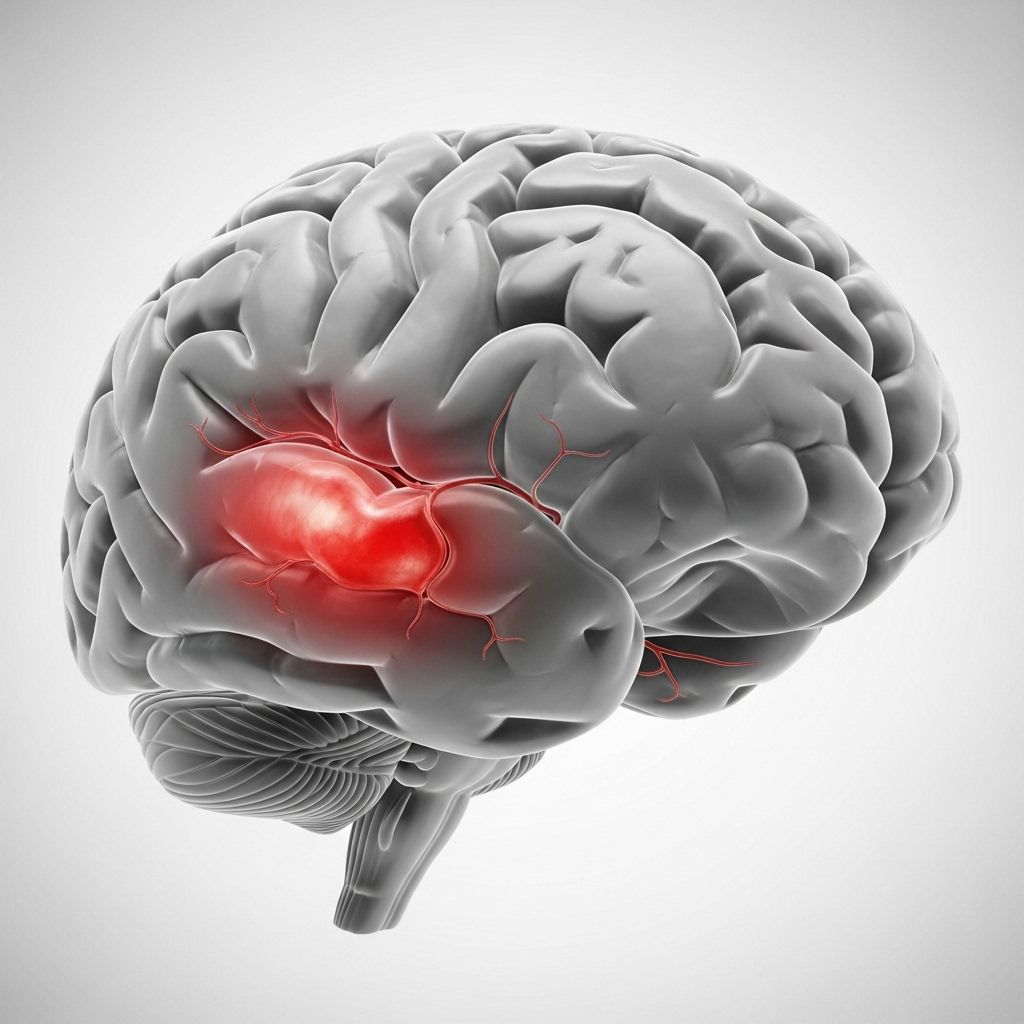
Intraventricular hemorrhage (IVH) is a serious neurological condition characterized by bleeding into the brain’s ventricular system—the interconnected spaces filled with cerebrospinal fluid (CSF) that cushion and support the brain. While IVH can affect individuals of all ages, it most commonly occurs in premature infants due to the fragility of developing blood vessels. Timely detection, prompt treatment, and diligent long-term monitoring are crucial in managing this complex disorder and minimizing its complications.
What is Intraventricular Hemorrhage?
Intraventricular hemorrhage is defined as bleeding within the ventricular system—the spaces inside the brain that produce and circulate CSF. The ventricles act as the plumbing of the brain, providing cushioning and waste removal. When blood leaks into these spaces, it can obstruct fluid flow, damage brain tissue, and cause swelling or pressure, leading to significant neurological problems.
Premature babies, especially those born before 32 weeks of gestation, are at the highest risk for IVH. In these infants, the walls of the ventricles contain a fragile and richly vascularized area called the germinal matrix, which is highly susceptible to rupture. Although less common, IVH can also develop in older children and adults, usually as a result of trauma, vascular anomalies, or underlying health issues.
Why is IVH a Concern?
The primary danger of IVH is that bleeding in the brain can compress nerve cells, disrupt normal brain development, and block the flow of CSF. This may result in:
- Cerebral injury and loss of brain function
- Development of hydrocephalus (fluid accumulation in the brain)
- Increased intracranial pressure
- Long-term cognitive and motor impairments—especially in severe cases
In the most severe forms, IVH can cause lasting disabilities, developmental delays, or death.
Grades of Intraventricular Hemorrhage
IVH is classified into four grades, according to the severity and location of bleeding:
| Grade | Extent of Bleeding | Typical Prognosis |
|---|---|---|
| Grade I | Bleeding is confined to the germinal matrix, a small area near the ventricles | Usually mild with good outcomes; minimal complications |
| Grade II | Bleeding extends slightly into the ventricles without causing enlargement | Often mild; many infants recover without disabilities |
| Grade III | Significant bleeding with enlargement (dilatation) of the ventricles due to blood accumulation | Risk of complications; higher chance of hydrocephalus and neurological issues |
| Grade IV | Severe bleeding extends beyond ventricles into surrounding brain tissue | Most serious; likely to result in long-term neurological impairment or death |
Causes of Intraventricular Hemorrhage
The causes of IVH vary by age group, but the underlying mechanism is always the rupture of fragile blood vessels that bleed into the ventricles. Common causes include:
- Prematurity: The leading cause in newborns, especially babies born before 32 weeks. Their brain blood vessels are underdeveloped and can tear easily.
- Respiratory distress syndrome and other prematurity complications: Increases the risk of fragile vessel rupture.
- Brain trauma or head injury: More common in older children and adults; direct injury can cause vessel rupture.
- Arteriovenous malformations (AVMs): Abnormal tangles of blood vessels in the brain can burst and bleed.
- Aneurysms: Weak, bulging spots in a vessel wall may rupture, leading to IVH.
- Blood-thinning medications (such as warfarin or aspirin): Increase bleeding risk if a vessel ruptures.
- Brain tumors (occasionally): Can erode or press on blood vessels, causing bleeding.
- Cerebral amyloid angiopathy (CAA): Protein buildup in vessel walls (usually in older adults) increases fragility.
- Hypertension: Uncontrolled high blood pressure weakens vessels over time.
- Infections (like meningitis): Can inflame blood vessels, making rupture more likely.
Risk Factors for Developing IVH
Certain maternal and infant health conditions can increase the risk of IVH in newborns:
- Premature birth (before 32 weeks gestation)
- Low birth weight (less than 1,500 grams or 3.3 pounds)
- Maternal high blood pressure, diabetes, anemia, or infection
- Rapid or difficult labor and delivery
- Babies with respiratory distress or needing mechanical ventilation
- Advanced maternal age
- Familial/genetic factors
- Alcohol or drug use during pregnancy
Symptoms of Intraventricular Hemorrhage
The symptoms of IVH can vary dramatically depending on the patient’s age, the degree of bleeding, and whether other areas of the brain are affected. In premature babies, signs are often subtle or may only be detected by screening. In adults and older children, symptoms tend to be abrupt and severe.
Common Symptoms in Premature Infants
- Apnea (stopping of breathing) and bradycardia (slow heart rate)
- Pale or blue skin coloration (cyanosis)
- Poor or weak sucking reflex
- High-pitched, unusual cry
- Seizures
- Swelling or bulging of fontanelles (soft spots on the baby’s head)
- Anemia (low blood count)
- Sudden or ongoing lethargy
- Poor muscle tone
- Difficulty feeding
Symptoms in Older Children and Adults
- Severe headache
- Nausea and vomiting
- Sudden vision changes
- Loss of consciousness or confusion
- Weakness or paralysis (especially on one side of the body)
- Difficulty speaking or thinking clearly
- Seizures
- Coma
Symptoms can escalate rapidly if the bleeding is severe or if it causes hydrocephalus (fluid buildup), which increases intracranial pressure and threatens brain tissue.
Diagnosis of Intraventricular Hemorrhage
Early diagnosis is crucial for effective management and reducing long-term damage. Evaluation usually includes:
- Clinical history and physical examination: Checks for neurological signs, head circumference, and overall health.
- Cranial ultrasound: The standard method to detect IVH in infants. Ultrasound waves create images of the brain through the fontanelles.
- CT (computed tomography) scan: Offers more detailed brain images, often used in older children and adults.
- MRI (magnetic resonance imaging): Provides precise images for follow-up and to assess for associated injuries.
Imaging not only confirms the presence of IVH but also determines the grade, guides treatment decisions, and monitors progress.
Treatment and Management of IVH
There is no cure for IVH, and treatment is largely supportive, aiming to minimize the progression of the bleed and manage any resulting complications. The intensity of treatment depends on the severity of bleeding, presence of hydrocephalus, and underlying causes.
Supportive Care in the Neonatal Intensive Care Unit (NICU)
- Continuous monitoring of vital signs and neurological status
- Ensuring adequate oxygen, blood pressure, and glucose levels
- Minimizing stimuli to reduce further stress or injury
- Intravenous fluids and nutrition support if feeding is difficult
- Blood transfusions in cases of significant anemia
Managing Hydrocephalus and Raised Intracranial Pressure
- Monitoring head growth and regular imaging
- Temporary drainage with a ventricular reservoir or ventriculostomy catheter
- Permanent shunt placement (ventriculoperitoneal shunt) for ongoing or severe hydrocephalus
Other Treatments
- Treating underlying causes (e.g., controlling infections or hypertension)
- Seizure management with anti-epileptic drugs, if required
- Rehabilitation and therapy for developmental or motor delays
Corticosteroid medications (given to mothers at risk of preterm delivery) have been shown to reduce the risk of IVH in premature babies. However, there are no specific interventions to stop or reverse the bleeding once it begins.
Complications and Long-term Outlook
Potential Complications
- Hydrocephalus: The most common complication; persistent accumulation of CSF may require surgery.
- Developmental delays, intellectual disabilities, and learning difficulties
- Speech and language problems
- Movement disorders (cerebral palsy)
- Seizure disorders
- Vision or hearing impairments
- Paralysis (in severe cases)
Long-term Prognosis
The long-term outcome depends mainly on the grade of IVH, extent of injury, and overall health:
- Grades I and II: Many infants recover well with few to no lasting effects if no hydrocephalus develops.
- Grades III and IV: Higher risk of neurological or developmental complications; aggressive management and early therapy are essential.
- Early intervention services are vital for maximizing developmental potential.
Prevention and Risk Reduction
IVH prevention focuses on identifying at-risk pregnancies and minimizing preterm births. Steps that may reduce the risk include:
- Avoiding premature deliveries when safely possible
- Providing mothers at risk of preterm labor with corticosteroids
- Optimal management of maternal health issues (e.g., blood pressure, infections)
- Gentle handling and minimizing stress for premature infants after birth
Frequently Asked Questions (FAQs)
Q: What is the most common group affected by intraventricular hemorrhage?
A: Premature infants, especially those born before 32 weeks of gestation and/or with a birth weight less than 1,500 grams, have the highest risk.
Q: What are the early signs of IVH in newborns?
A: Common early signs include apnea, bradycardia, pallor, a bulging fontanelle, seizures, and a weak suck or cry. Some cases may show no immediate symptoms and are discovered through routine brain imaging.
Q: Can IVH be completely prevented?
A: While advances in obstetric and neonatal care have reduced the rates of severe IVH in preterm babies, not all cases are preventable. Corticosteroids given to mothers at risk for early delivery can lower the risk.
Q: What is the outlook for babies diagnosed with IVH?
A: Many infants with mild (grades I or II) IVH achieve normal development. Those with more severe forms may require long-term therapies and may have developmental or neurological challenges.
Q: What should parents expect if their baby is diagnosed with IVH?
A: Parents can expect intensive monitoring in the NICU, regular imaging to assess for progression, possible interventions for hydrocephalus, and supportive therapies. Early intervention programs can help maximize developmental outcomes.
Supporting Families and Looking Ahead
Diagnosis of intraventricular hemorrhage can be a distressing and frightening experience for families. Support from a multidisciplinary medical team—including neonatologists, neurologists, therapists, and social workers—can help guide families through treatment choices and ongoing care. Early recognition, timely intervention, and access to resources and therapies can significantly improve the outlook for many children affected by IVH.
References
- https://www.aurorahealthcare.org/services/neuroscience/brain-skull-base-care/brain-hemorrhage/intraventricular-hemorrhage
- https://www.chop.edu/conditions-diseases/intraventricular-hemorrhage
- https://www.cerebralpalsyguide.com/birth-injury/intraventricular-hemorrhage/
- https://medlineplus.gov/ency/article/007301.htm
- https://my.clevelandclinic.org/health/diseases/14480-brain-bleed-hemorrhage-intracranial-hemorrhage
- https://pubmed.ncbi.nlm.nih.gov/11096707/
- https://radiopaedia.org/articles/intraventricular-haemorrhage?lang=us
- https://www.stlouischildrens.org/conditions-treatments/intraventricular-hemorrhage
Read full bio of medha deb












