Intrathecal Pain Pump: Targeted Pain Management for Chronic Conditions
Comprehensive overview of intrathecal pain pump therapy: benefits, procedure, risks, and patient suitability for chronic pain relief.
Intrathecal Pain Pump Therapy: Comprehensive Guide
Chronic pain and severe spasticity are life-altering conditions that often fail to respond to conventional treatments. Intrathecal pain pumps, also known as intrathecal drug delivery systems (IDDS), provide a targeted solution by delivering medication directly into the fluid-filled space surrounding the spinal cord, revolutionizing pain management for those with persistent conditions.
What is an Intrathecal Pain Pump?
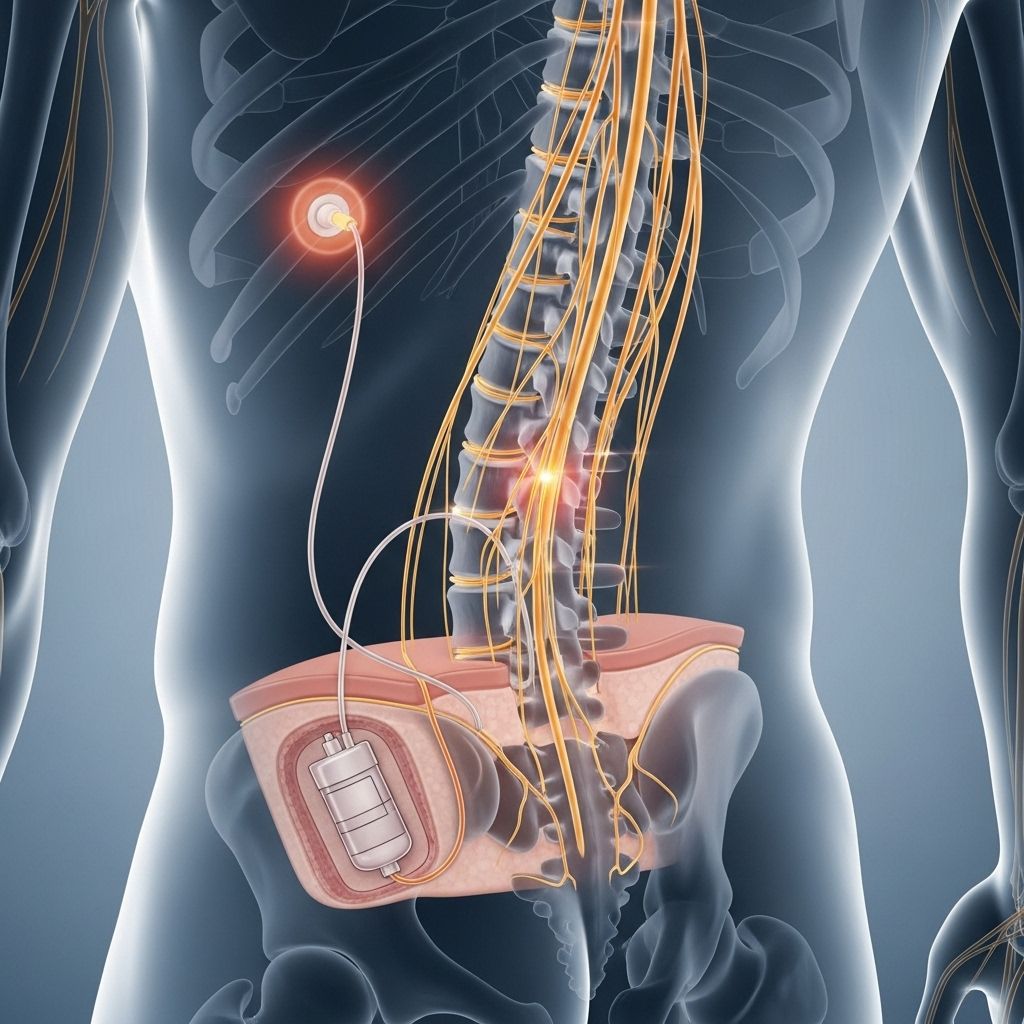
An intrathecal pain pump is a small, programmable medical device implanted under the skin—usually in the abdominal area. It stores and releases prescribed amounts of medication through a thin catheter, delivering it precisely into the intrathecal space around the spinal cord.
- Pump: Disk-shaped, about 1 inch thick and 3 inches wide, hidden beneath the skin.
- Catheter: A thin, flexible tube connected to the pump, directing medication into the spinal fluid.
This targeted system allows pain medication to reach the central nervous system rapidly and efficiently, blocking pain signals before they reach the brain. Due to the focused delivery, doses are significantly lower than oral medications, reducing systemic side effects and improving daily functioning.
Conditions Treated with Intrathecal Pumps
- Failed back surgery syndrome
- Cancer pain
- Nerve pain
- Spasticity associated with cerebral palsy, multiple sclerosis, stroke, brain injury, or spinal cord injury
- Chronic pain not responsive to other treatments
How Does an Intrathecal Pain Pump Work?
The pump is programmed to release precise doses of medication—such as morphine, baclofen, or other pain-blocking agents—at scheduled intervals or variably throughout the day depending on individual needs. Physicians can externally program dose adjustments and change medications based on the patient’s evolving condition.
- Delivers medication directly into the intrathecal space around the spinal cord
- Blocks pain signals at the source
- Reduced risk of systemic side effects compared to oral or intravenous drugs
When the pump’s reservoir is empty, refills are done as an outpatient procedure by inserting a needle through the skin into the pump’s fill port, minimizing disruption to patient life.
Trial Phase Prior to Implantation
Before permanent implantation, a trial injection or temporary pump is used to assess the medication’s efficacy and tolerability. Only patients who respond positively during the trial become candidates for permanent placement.
- Ensures effectiveness
- Prevents unnecessary surgery in non-responders
The Implantation Procedure
- A small incision is made in the back for catheter placement into the intrathecal space of the spine.
- The catheter is tunneled under the skin to the abdomen, where the pump is implanted.
- The device is hidden and typically does not affect appearance.
- The procedure is performed under anesthesia by a neurosurgeon or pain specialist.
After surgery, patients can return home once they recover from anesthesia, with specific instructions for wound care and pump management.
Benefits and Advantages of Intrathecal Pain Pumps
- Targeted pain relief: Delivers medication directly to spinal pain receptors for rapid, dramatic improvement.
- Lower medication doses: Uses much smaller doses than oral therapy, sharply reducing systemic effects like constipation, drowsiness, and nausea.
- Customizable therapy: Pump programming and refill schedules can be tailored to patient needs.
- Reduced dependency risk: The limited, targeted dosing lowers the risk of addiction associated with higher oral opioid doses.
- Improved quality of life: Enhanced daily function, mobility, activity participation, and sleep.
- Reversible treatment: If undesirable effects occur or no longer needed, the pump can be removed.
- Long-term cost savings: Fewer hospitalizations, reduced medication costs, and improved management of chronic pain may offset upfront device expense.
Who Is a Candidate for Intrathecal Pain Pump Therapy?
Selection criteria are strict to ensure patient safety and efficacy.
- Chronic, severe pain or spasticity not controlled by other treatments or medications
- Failure to benefit from conservative therapies or surgery
- Need for high-dose oral pain medications
- No psychological problems interfering with pain management
- No medical contraindications (such as infection, bleeding disorders, or severe cardiopulmonary disease)
- No allergies to pump medications
- Positive response to trial phase
Potential Risks and Side Effects
While intrathecal pumps are generally safe and well-tolerated, individuals must be aware of possible complications:
- Infection at the surgical site
- Cerebrospinal fluid leakage
- Catheter problems: Dislocation, blockage, or breakage leading to inadequate drug delivery
- Pump malfunction: rare but may result in over- or under-dose delivery
- Possible drug side effects, such as drowsiness, nausea, and muscle weakness
- Risk of withdrawal or overdose if pump fails or programming errors occur
- Allergic reactions to medications
- Serious risks are minimized by regular follow-up and device maintenance
Life with an Intrathecal Pain Pump
Most patients experience better pain control, increased activity, improved sleep, and fewer medication-related side effects. Regular clinic visits are required to refill the pump, monitor device function, and adjust programming as needs evolve.
- Pump refills every few months
- Device programming by healthcare provider
- No restrictions on most daily activities—can travel, work, and exercise with care
- Notify healthcare team of new symptoms or pump issues
Medication Types Used in the Pump
- Opioids (morphine, hydromorphone)
- Baclofen (for severe muscle spasticity)
- Local anesthetics
- Combinations for tailored therapy
- Medication and dose adjusted individually
Frequently Asked Questions (FAQs)
Q: Who is a suitable candidate for intrathecal pain pump therapy?
A: Candidates must have chronic pain or spasticity unmanageable with oral medications or other therapies, no contraindicating health issues, and a positive response to the preliminary trial phase.
Q: What medications can be delivered by an intrathecal pain pump?
A: Common medications include morphine, baclofen, and hydromorphone, as well as combinations for specific pain or spasticity profiles.
Q: How is the pump refilled?
A: Refills are performed by health professionals, typically every few months, using a needle inserted into a reservoir port under the skin. The pump remains implanted permanently or until no longer needed.
Q: Can the pump be removed?
A: Yes. The therapy is fully reversible if the patient chooses or if side effects outweigh benefits.
Q: What are the main risks and complications?
A: Infection, pump malfunction, catheter issues, and drug side effects. These are rare but are minimized by careful patient selection and ongoing monitoring.
Q: How does the pump affect daily life?
A: Most daily activities, work, travel, and moderate exercise are possible with care. The hidden implant allows normal appearance, but regular check-ups are required.
Comparing Intrathecal Pain Pump to Oral Pain Medications
| Feature | Intrathecal Pain Pump | Oral Pain Medication |
|---|---|---|
| Delivery Method | Direct to spinal fluid | Systemic, via bloodstream |
| Dose Required | Low, targeted | High, generalized |
| Side Effects | Fewer, localized | More, systemic |
| Efficacy for chronic pain/spasticity | High | Variable |
| Adjustment capability | Programmable | Limited |
Summary: Is an Intrathecal Pain Pump Right for You?
For those living with severe, chronic pain or spasticity unresponsive to other treatments, an intrathecal pain pump offers hope for improved comfort, mobility, and quality of life. Patients considering this therapy should consult with a pain management specialist or neurosurgeon to discuss their specific diagnosis, medical history, goals, and eligibility for a trial. Individualized device programming and careful monitoring maximize safety and benefit, offering a highly customizable approach to long-term pain relief.
References for Further Reading
- UPMC: Understanding an Intrathecal Drug Pain Pump Implant
- Pain Care Florida: What Is an Intrathecal Pain Pump Implant?
- Improving Pain: Pain Pump, Intrathecal Drug Pump Types, Pros and Cons
References
- https://www.upmc.com/services/neurosurgery/spine/treatment/pain-management/intrathecal-pump
- https://paincareflorida.com/what-is-an-intrathecal-pain-pump-implant/
- https://www.improvingpain.com/pain-pump-intrathecal-drug-pump-types-pros-and-cons/
- https://paincareflorida.com/pain-care-treatments/intrathecal-pump-implantation/
- https://pure.johnshopkins.edu/en/publications/introduction-and-background-for-intrathecal-pumps-used-for-pain-a
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4200017/
- https://pure.johnshopkins.edu/en/publications/best-practices-for-intrathecal-drug-delivery-for-pain-4
- https://files.wearesrna.org/newsletters/j2/journal-2-09.htm
Read full bio of medha deb












