Intra-Aortic Balloon Pump Therapy: Treatment, Procedure, and Considerations
Comprehensive exploration of intra-aortic balloon pump therapy: mechanism, uses, procedure, and frequently asked questions for patients and professionals.
Intra-Aortic Balloon Pump Therapy
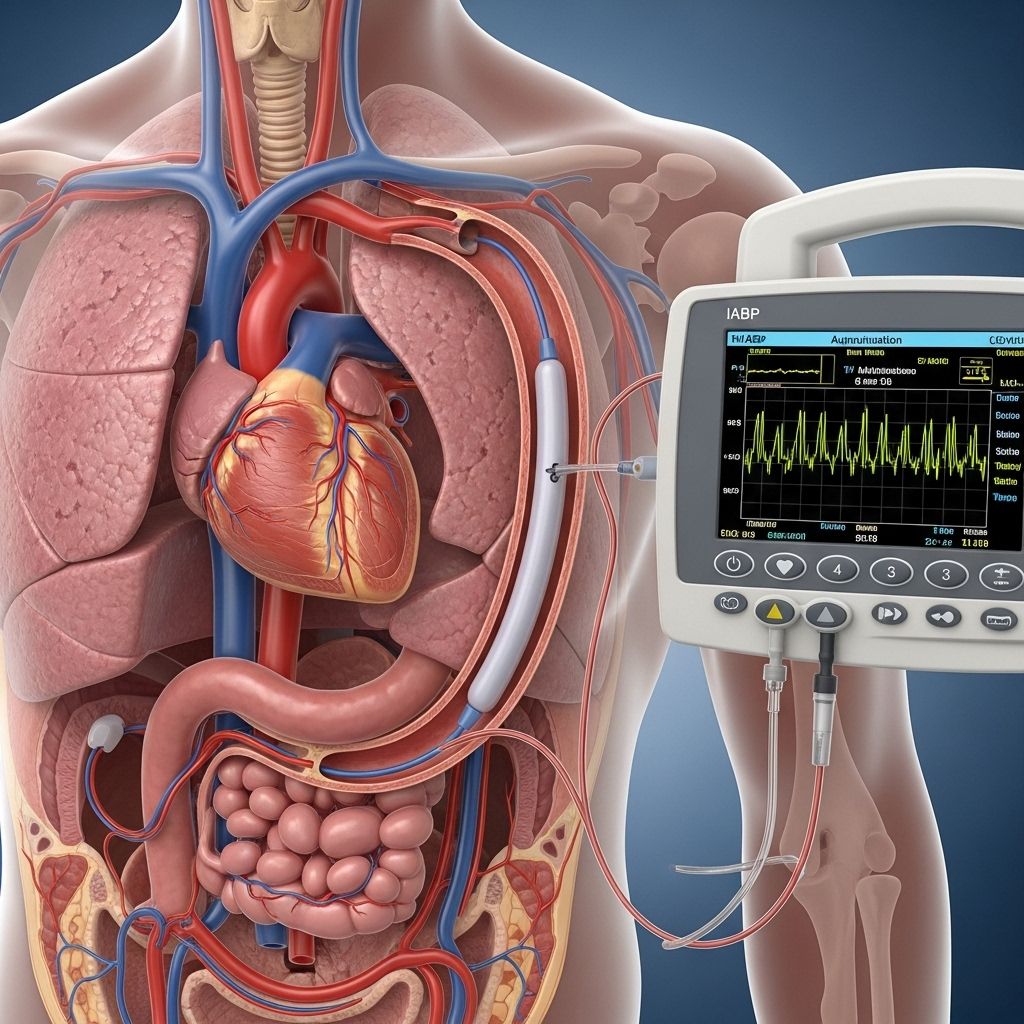
An intra-aortic balloon pump (IABP) is a specialized device designed to assist the heart in pumping more effectively, providing critical support in certain serious cardiac conditions. This therapy is instrumental when the heart struggles to circulate enough blood to meet the body’s needs, especially in acute or emergency settings.
The IABP is widely used in cardiac care, acting as a bridge during recovery or while awaiting further intervention such as surgery or stenting, and has lifesaving potential for certain patient groups.
What Is an Intra-Aortic Balloon Pump?
At its core, an IABP consists of a thin, flexible catheter with a long balloon attached to its tip. The catheter is inserted into an artery, typically through the upper thigh or groin area, and guided into the aorta—the body’s largest artery which carries oxygen-rich blood away from the heart.
The other end of the catheter connects to a console equipped with mechanisms to inflate and deflate the balloon, coordinated with the heart’s rhythm. The inflation of the balloon occurs during the heart’s relaxation phase (diastole), increasing blood flow to the coronary arteries, while deflation happens during contraction (systole), reducing workload and facilitating blood ejection from the heart.
- Inflation during diastole: Pushes blood into the coronary arteries, enhancing heart perfusion.
- Deflation during systole: Reduces resistance, lowers left ventricular workload, and supports systemic blood flow.
How Does an Intra-Aortic Balloon Pump Work?
The IABP works through a process called counterpulsation—the balloon synchronizes with the heartbeat, inflating during relaxation and deflating during contraction. This rhythmic support has several physiological benefits:
- Improves myocardial oxygenation by increasing coronary artery perfusion.
- Enhances cardiac output, thus improving circulation to vital organs.
- Decreases left ventricular workload by reducing afterload.
Helium is commonly used to inflate and deflate the balloon due to its low density and rapid movement, ensuring efficient timing with each heartbeat.
Indications for Intra-Aortic Balloon Pump Therapy
IABP therapy is indicated in a variety of critical cardiac conditions where short-term circulatory support is required. The most common indications include:
- Cardiogenic shock: When the heart is unable to supply sufficient blood to the body, often triggered by severe heart attacks or acute heart failure.
- Unstable angina: Persistent chest pain due to inadequate blood supply to heart tissue.
- Acute myocardial infarction (MI): Heart attacks that compromise pumping ability.
- Abnormal heart rhythms: Certain arrhythmias that result in poor cardiac output.
- Severe heart failure: Decompensated heart function requiring urgent support.
- Bridge to further intervention: Temporary support before surgery, such as bypass, valve repair, or percutaneous coronary intervention (angioplasty/stenting).
- Post-operative support: Cardiac surgery patients who are slow to recover adequate heart function.
- Severe ischemic heart disease: Awaiting definitive therapy.
- Miscellaneous: Some rare emergencies, such as stopping massive hemorrhage from the aorta or its branches.
Contraindications and Limitations
The use of an IABP is not suitable for all patients. Certain medical conditions or anatomical issues make IABP therapy unsafe, and alternatives are considered where necessary.
- Aortic regurgitation: Leaky aortic valve permitting backward blood flow.
- Aortic dissection: Active tear or separation in the aortic wall.
- Severe aortoiliac or peripheral vascular disease: Compromised or narrowed vessels may prevent safe insertion.
- Aneurysm or anatomical disease of the aorta: Increased rupture risk.
- Prosthetic aortic tree grafts: Artificial replacements in the aorta may be damaged.
- Local infection or sepsis: Risk of spreading infection.
- Severe coagulopathy: Increased risk of bleeding with catheter manipulation.
- Lack of experience: Requires skilled providers for safe management.
- Tachyarrhythmias: Very fast, irregular heart rhythms may hinder device timing.
- Low cardiac index (< 1.2): Device may not be effective in severely compromised hearts.
Components and Features of the Intra-Aortic Balloon Pump
The IABP is made up of several integral parts, each contributing to its precise function:
- Balloon catheter: Long, sausage-shaped polyurethane membrane with varying sizes (generally 7.5 French, balloon volume 25–50 cc adjusted to patient height).
- Pump console: Device containing the pump to inflate/deflate the balloon and synchronize with cardiac cycle.
- Pressure monitoring: Newer catheters feature fiber optics for improved pressure waveform detection and timing.
- Helium transmission: Helium gas is rapid, non-toxic and easily eliminated in the event of leakage or rupture.
- Positioning: Balloon usually occludes 80–90% of the aorta when inflated, ensuring effective pressure augmentation.
Procedure: Placement of Intra-Aortic Balloon Pump
Insertion of an IABP typically occurs in a sterile, controlled environment, though emergencies may necessitate bedside placement.
A step-by-step outline of the procedure:
- Patient positioned supine; sterile preparation (gown, gloves, drapes, disinfectant).
- Bleeding disorders or other complications are ruled out.
- The balloon is fully collapsed beforehand, typically using a vacuum syringe.
- Femoral artery accessed at 45-degree angle, often using the percutaneous Seldinger technique (needle-guidewire-sheath method); occasionally surgical cut-down.
- Guidewire advanced to thoracic aorta; sheath placed over wire if required.
- Balloon catheter is threaded over the guidewire through sheath, positioned by measuring the distance from sternal angle to umbilicus then femoral artery.
- Proper positioning confirmed to ensure the balloon tip sits 1 cm below the origin of the left subclavian artery.
- Wire is removed; return of blood through central lumen confirms proper placement.
- Central lumen flushed and connected to a pressure transducer; outer lumen attaches to helium source.
- Continuous monitoring of heart rate, blood pressure, and device function during therapy.
Key Points in Insertion
- Ensure balloon is not too high (loss of left radial pulse).
- Avoid subintimal placement to prevent aortic dissection.
- Monitor for bleeding or vascular complications at the insertion site.
Potential Risks and Complications of IABP Therapy
While the IABP is generally safe when used appropriately, certain risks and complications may arise, especially in high-risk or critically ill patients.
Key potential complications include:
- Vascular injury: Damage to arteries, bleeding, or hematoma at insertion site.
- Infection: Risk at the catheter entry point or inside the vessel.
- Balloon rupture: Can lead to helium embolism or suboptimal performance.
- Aortic dissection or rupture: Rare but life-threatening, usually in patients with predisposing aortic conditions.
- Limb ischemia: Reduced blood flow to the lower leg due to arterial occlusion.
- Thrombosis: Formation of blood clots around the catheter.
- Device malfunction: Mis-timing of balloon inflation/deflation or console failure, requiring prompt troubleshooting.
Benefits and Limitations of Intra-Aortic Balloon Pump Therapy
| Benefits | Limitations |
|---|---|
|
|
Aftercare and Recovery
Following insertion, patients require close monitoring, usually in an intensive care or cardiac unit.
During therapy and recovery:
- Vital signs and cardiac function are continuously observed.
- Careful assessment for vascular complications is performed.
- Site of insertion maintained in sterile condition to prevent infection.
- Physical activity is restricted to limit movement of the catheter.
- Anticoagulation may be used to prevent clot formation.
- When the underlying cardiac condition improves, or after definitive procedures, the balloon pump is gradually weaned and removed.
Length of therapy varies from several hours to a few days, depending on the patient’s response and recovery.
Frequently Asked Questions (FAQs) About Intra-Aortic Balloon Pump Therapy
Q: What does an intra-aortic balloon pump do?
A: An IABP assists the heart by inflating during diastole to push blood towards the coronary arteries and deflating during systole to reduce resistance, supporting cardiac function in critical situations.
Q: Who needs an intra-aortic balloon pump?
A: Patients with cardiogenic shock, unstable angina, severe heart attacks, or those undergoing certain high-risk procedures may require IABP therapy.
Q: How long does intra-aortic balloon pump therapy last?
A: The duration varies, but most therapies last from several hours to a few days, depending on individual clinical needs and recovery progress.
Q: Is the procedure painful?
A: General or local anesthesia is used during insertion, so patients typically do not experience pain during the procedure. Some discomfort may occur at the insertion site post-procedure.
Q: What are the main risks?
A: Principal risks include vascular injury, infection, bleeding, balloon rupture, and limb ischemia.
Q: Can everyone use an intra-aortic balloon pump?
A: No. Individuals with aortic regurgitation, aortic aneurysm, severe peripheral vascular disease, or certain other conditions cannot safely use the pump.
Q: How is the pump removed?
A: Removal is generally performed by the medical team once the underlying cardiac condition has stabilized, using sterile technique in a controlled setting.
Conclusion
Intra-aortic balloon pump therapy remains a key tool in the management of critical cardiac conditions, providing immediate yet temporary circulatory support for patients in need. Understanding its mechanism, procedural approach, benefits, risks, and patient selection criteria is essential for clinicians and patients alike when considering this advanced therapy option.
Always consult specialized cardiac care teams for individualized assessment and guidance regarding IABP therapy.
References
- https://litfl.com/intra-aortic-balloon-pump-ccc/
- https://www.urmc.rochester.edu/encyclopedia/content?contenttypeid=135&contentid=341
- https://my.clevelandclinic.org/health/treatments/23527-intra-aortic-balloon-pump
- https://www.getinge.com/int/products-and-solutions/cardiovascular-procedures/iabp-counterpulsation/
- https://pubmed.ncbi.nlm.nih.gov/33616109/
- https://www.youtube.com/watch?v=Lycn_4fgeSc
Read full bio of Sneha Tete












