Intra-Aortic Balloon Pump (IABP): Purpose, Procedure, Risks, and Recovery
An in-depth look at the intra-aortic balloon pump (IABP), how it assists the heart, when it's used, procedural steps, recovery, and potential risks.
What Is an Intra-Aortic Balloon Pump (IABP)?
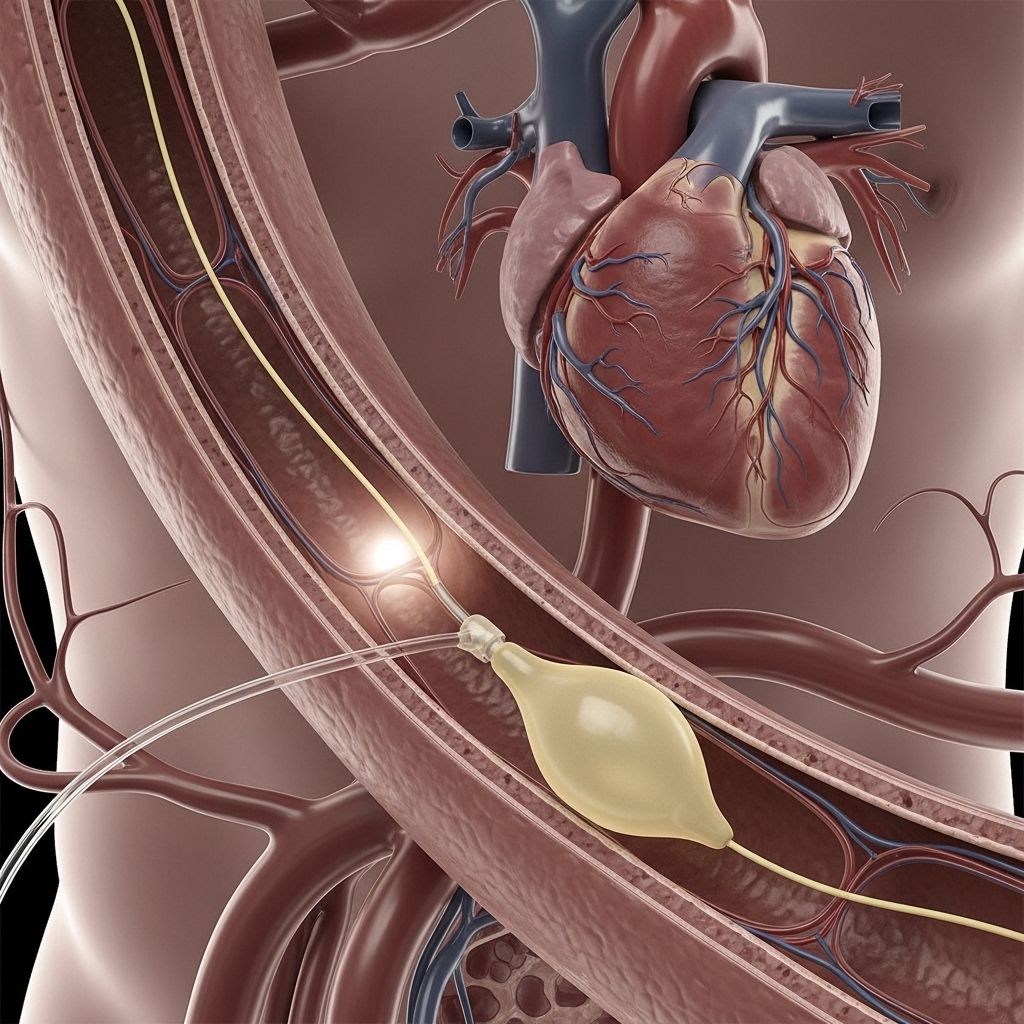
An intra-aortic balloon pump (IABP) is a specialized mechanical device designed to temporarily support the heart when it is unable to pump enough blood to meet the body’s needs. It involves a thin catheter with a balloon at the end, which is placed inside the largest artery in the body—the aorta. By inflating and deflating in rhythm with the heartbeat, the IABP enhances blood flow and reduces the workload on the heart, offering a life-saving bridge for people with severe cardiac compromise.
Why Is an IABP Used?
An IABP is reserved for people whose hearts cannot supply enough blood to vital organs due to severe heart disease, cardiogenic shock, or as a bridge to other treatments. It is not a permanent solution, but rather a temporary means of stabilizing patients. The device is most commonly used in the following circumstances:
- Following a major heart attack that compromises heart function.
- Sudden, severe heart failure unresponsive to standard therapies.
- Patients awaiting heart transplantation or other advanced cardiac procedures.
- In some cases, during high-risk cardiac surgeries or procedures such as percutaneous coronary intervention (PCI).
How Does an IABP Work?
The IABP enhances heart function through a process known as counterpulsation. The device consists of a thin, flexible catheter with an inflatable balloon. The procedure works as follows:
- The IABP is inserted into the aorta, typically via the femoral artery in the groin.
- During diastole (when the heart rests between beats), the balloon inflates. This inflation helps push oxygen-rich blood back toward the coronary arteries, supplying the heart muscle itself with more blood and oxygen.
- As systole (when the heart contracts) begins, the balloon rapidly deflates. This creates more space within the aorta, lowering the resistance against which the left ventricle must pump. The result is decreased workload (afterload) on the heart and improved blood delivery to the rest of the body.
| Phase of Heartbeat | Balloon Action | Result |
|---|---|---|
| Diastole (rest) | Balloon inflates | Boosts coronary circulation |
| Systole (contraction) | Balloon deflates | Reduces afterload, eases pumping |
This dual action maximizes blood supply to the heart muscle while minimizing the work the heart must perform, especially in times of critical need.
Indications for IABP Use
- Cardiogenic shock: A life-threatening state where the heart fails to supply enough blood to the body’s vital organs, often due to a major heart attack or advanced heart failure.
- High-risk cardiac procedures: Such as complex angioplasty or coronary artery bypass surgeries in unstable patients.
- Temporary support before transplant: For patients awaiting heart transplantation or the implantation of a left ventricular assist device (LVAD).
- Weaning from cardiopulmonary bypass: After heart surgery, to support a heart not yet strong enough to function on its own.
How To Prepare for an IABP Procedure
If your doctor recommends an IABP, you will likely be admitted to a hospital intensive care unit. Here’s what to expect:
- You will undergo routine blood tests, chest X-rays, and an electrocardiogram (ECG) to assess heart function.
- The insertion site—usually the groin—will be cleaned and possibly shaved to minimize infection risk.
- You may receive sedatives or painkillers, but won’t need general anesthesia unless combined with a larger surgical procedure.
- An intravenous (IV) line will provide fluids and medications during the procedure.
Your healthcare team will explain the procedure and obtain your consent. Inform them of any allergies (especially to latex, iodine, or medications) and provide a list of your medications.
What Happens During the IABP Procedure?
- The doctor will numb the insertion site, usually in the upper thigh (femoral artery), using a local anesthetic.
- A thin, flexible catheter is then advanced through the artery and into the descending aorta, guided by X-ray imaging (fluoroscopy) to ensure precise positioning.
- Once in place, the balloon is connected to a bedside machine that controls its inflation and deflation, synchronized with your heartbeat.
The entire process usually takes between 30 and 60 minutes. The catheter and balloon remain outside your body, attached to the drive console at the bedside so adjustments can be made as needed.
After the Procedure: Recovery and Monitoring
After IABP insertion, you will recover in the intensive care or coronary care unit for close monitoring. Key points to expect include:
- Your heart rhythm, blood pressure, and oxygen levels will be continuously monitored.
- Blood tests will be performed regularly to track heart and kidney function.
- The leg with the catheter insertion must be kept as straight and still as possible to avoid dislodging the device or causing bleeding.
- Pain, swelling, or signs of infection at the insertion site will be closely watched.
- You may receive antibiotics to minimize infection risk and blood thinners to prevent clot formation.
Most patients require the IABP for a period ranging from several hours to a few days, depending on their condition and response to treatment.
Benefits of the Intra-Aortic Balloon Pump
- Improved coronary blood flow: Delivers more oxygen-rich blood to the heart muscle, aiding recovery and reducing damage.
- Reduced heart workload: By lowering afterload, the heart’s oxygen demand decreases, helping the failing muscle rest.
- Enhanced systemic circulation: Increases overall blood flow and can lead to improved kidney and end-organ function.
- Temporary support: Buys time for patients to recover or undergo further treatments like surgery or transplant.
Risks and Potential Complications
Although the IABP can be life-saving, it carries some risks and possible complications, including:
- Infection at the catheter insertion site or in the bloodstream.
- Bleeding or hematoma (collection of blood) at the insertion site, especially in people taking blood thinners.
- Blood clots may form and potentially travel to the brain (causing stroke), lungs, or other organs.
- Lower limb ischemia due to reduced blood supply to the leg where the device was inserted.
- Damage to the aorta, such as tearing or balloon rupture (rare).
- Problems with the device, such as incorrect timing settings or malfunction, which requires prompt attention.
Most complications can be minimized with expert monitoring and prompt intervention. The risk of infection increases the longer the IABP remains in place, which is why it is used for as short a duration as possible.
Who Should Not Have an IABP?
The IABP is not suitable for everyone. Contraindications may include:
- Significant aortic regurgitation (a heart valve disorder where blood leaks back toward the heart).
- Severe, widespread disease or obstruction of the aorta or major arteries.
- Irreversible brain damage or end-stage disease where recovery is not possible.
Alternatives to the IABP
Some patients may require more advanced circulatory support if the IABP is not sufficient. Other devices and procedures include:
- Ventricular assist devices (VADs): Mechanical pumps that help support or replace one or both ventricles of the heart.
- Extracorporeal membrane oxygenation (ECMO): A machine that adds oxygen to blood outside the body and pumps it back in, for short-term, full cardiac and respiratory support.
- Advanced medications (inotropes, vasopressors): To stimulate heart muscle contraction and maintain blood pressure.
Long-Term Outcomes and Prognosis
The IABP is designed as a temporary solution, providing critical support during periods of severe cardiac dysfunction. The outcome depends on the underlying heart condition, the patient’s response to the device, and the ability to transition to further intervention. For patients with acute heart failure or during recovery from high-risk procedures, the IABP can be life-saving. However, survival and recovery rates are strongly determined by the patient’s overall health, the extent of underlying heart disease, and the timeliness of definitive treatment.
Frequently Asked Questions (FAQs)
Q: Is an intra-aortic balloon pump a permanent device?
A: No. An IABP is designed for temporary support—typically for a few hours to several days—until the heart recovers or further procedures (like surgery or a ventricular assist device) can be performed.
Q: Will I feel the balloon working in my body?
A: Most patients do not feel the balloon’s inflation and deflation, but you might be aware of the presence of the catheter. Numbness, tingling, or pain in the leg should be reported immediately.
Q: Can you move around with an IABP in place?
A: Movement is usually restricted during IABP therapy. Patients are required to stay mostly still, particularly the leg where the catheter enters the body, to prevent dislodging the device and avoid bleeding complications.
Q: Does an IABP require surgery to remove?
A: No major surgery is required. The device is removed in a hospital setting, and the site is closed—often with manual pressure—to ensure bleeding does not occur.
Q: What are signs of complications to watch for?
A: Contact your healthcare team immediately if you or a loved one notice chest pain, difficulty breathing, fever, significant swelling, numbness, loss of sensation, or bleeding from the catheter site.
Summary: Key Takeaways About Intra-Aortic Balloon Pump
- The IABP temporarily supports the heart by boosting blood flow and reducing workload, providing a critical bridge for people with severe cardiac dysfunction.
- It is used in cases of heart attack, cardiogenic shock, significant heart failure, or as an aid during high-risk cardiac surgeries.
- The procedure involves inserting a catheter with a balloon into the aorta, which inflates and deflates in sync with heartbeats.
- Risks include bleeding, infection, and blood vessel complications, but careful medical management can minimize these.
- The IABP is a temporary solution, designed to stabilize patients until they can receive definitive treatment such as surgery or transplantation.
References
- https://www.cham.org/HealthwiseArticle.aspx?id=tx4071abc
- https://www.youtube.com/watch?v=Lycn_4fgeSc
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5971668/
- https://medmovie.com/library_id/3172/topic/cvml_0106i/
- https://www.medicalnewstoday.com/articles/intra-aortic-balloon-pump
- https://www.healthline.com/health/heart-failure
- https://litfl.com/intra-aortic-balloon-pump-ccc/
- https://encyclopedia.nm.org/Library/HealthSheets/3,S,90535
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3801197/
Read full bio of medha deb












