Insulin Mechanism of Action: How It Works in the Body
Explore how insulin regulates blood glucose, supports metabolism, and impacts diabetes management.
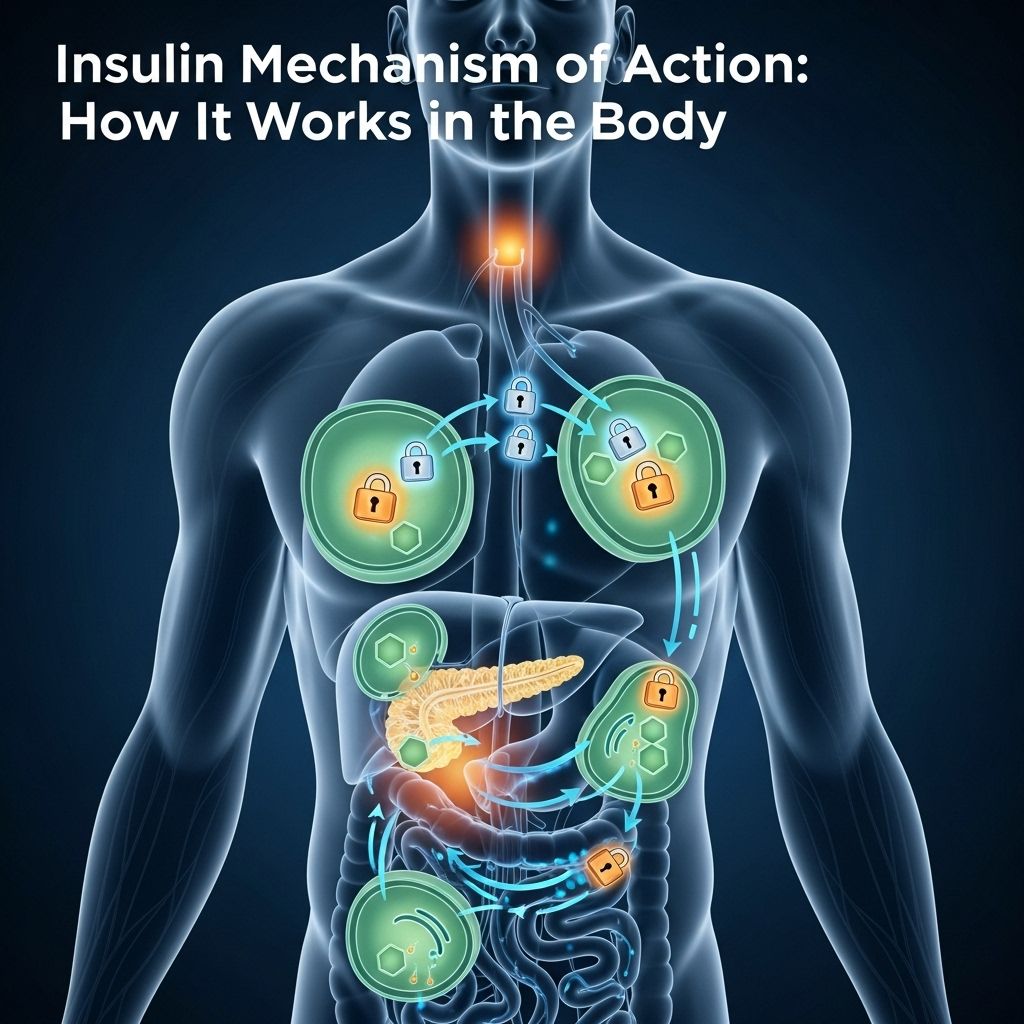
Insulin is a vital hormone produced by the pancreas, essential for regulating blood glucose levels and enabling the body to store and use nutrients efficiently. Understanding how insulin works provides insight into the management of diabetes and highlights the hormone’s broader impact on overall health.
What Is Insulin?
Insulin is a peptide hormone produced by the beta cells of the pancreatic islets. It plays a key role in carbohydrate, fat, and protein metabolism by promoting the absorption and storage of glucose from the blood into liver, muscle, and fat cells. Without enough insulin, or if it cannot function properly, blood glucose levels rise to unhealthy levels, resulting in conditions like diabetes.1
- Source: Beta cells of the pancreas
- Function: Facilitates glucose uptake and metabolism
- Major targets: Liver, muscle, adipose (fat) tissue
The Role of Insulin in Glucose Metabolism
Insulin directly regulates how the body processes glucose and other nutrients:
- Promotes glucose uptake by cells, especially muscle and adipose tissue
- Stimulates conversion of glucose to glycogen in the liver and muscles (glycogenesis)
- Supports conversion of glucose to fatty acids (lipogenesis) for long-term storage
- Inhibits breakdown of glycogen (glycogenolysis) and formation of new glucose (gluconeogenesis) in the liver
- Enhances protein synthesis and inhibits protein breakdown
The net effect is a drop in blood glucose levels and storage of energy for later use.2
How Is Insulin Produced?
Insulin synthesis in the beta cells is a multi-stage process:
- Synthesis of Preproinsulin: An inactive precursor protein, preproinsulin, is produced in the rough endoplasmic reticulum.
- Formation of Proinsulin: After removal of a signal peptide, it folds to form proinsulin, which contains three domains: the A-chain, B-chain, and connecting C-peptide.
- Maturation to Active Insulin: Proinsulin passes through the Golgi apparatus, where enzymes remove the C-peptide, leaving the mature insulin molecule composed of the A- and B-chains joined by disulfide bonds.
- Storage: Mature insulin is stored in secretory granules, ready to be released upon stimulation.
Insulin release is closely regulated by blood glucose levels. Increased glucose stimulates insulin secretion, while low glucose suppresses it. Other signals include amino acids, neural input, and certain hormones.1
How Does Insulin Work? The Mechanism of Action
Insulin’s action hinges on a series of highly coordinated cellular and molecular events:
Step 1: Insulin Binds to Its Receptor
Each insulin molecule binds to an insulin receptor on the surface of target cells (skeletal muscle, liver, adipose tissue). The insulin receptor is a protein composed of two alpha and two beta subunits. Insulin binds to the alpha subunits, triggering activation of the beta subunit’s tyrosine kinase enzyme activity.2
Step 2: Signal Transduction Cascade
Activation of the tyrosine kinase activity leads to autophosphorylation (a kind of self-activation) and further phosphorylation of insulin receptor substrates (IRS) and other adaptor proteins inside the cell.
- This triggers multiple signaling pathways, notably the PI3 kinase/Akt pathway, which are vital for glucose metabolism.2
Step 3: Effects Inside the Cell
The main outcome is the movement of GLUT4 (glucose transporter type 4) vesicles from inside the cell to fuse with the plasma membrane. This increases the cell’s capability to take up glucose from the bloodstream.3
- In muscle and fat cells, this is the critical step for glucose removal from the blood.
- Other effects: Increased protein synthesis, enhanced lipid synthesis, reduced breakdown of fat, and inhibition of gluconeogenesis (new glucose production by the liver).
Table: Key Effects of Insulin on Major Tissues
| Tissue | Effect of Insulin |
|---|---|
| Liver | Stimulates glycogen synthesis, inhibits gluconeogenesis |
| Muscle | Increases glucose uptake, promotes protein synthesis |
| Adipose (Fat) Tissue | Promotes uptake of glucose and synthesis of fatty acids, inhibits lipolysis (fat breakdown) |
Insulin Resistance: When the System Fails
Insulin resistance occurs when the cells of the body do not respond properly to insulin. As a result, higher levels of insulin are required for the same response, leading the pancreas to work overtime and resulting in hyperinsulinemia. Over time, blood glucose rises dramatically, a hallmark of type 2 diabetes.4
- Obesity, sedentary lifestyle, and genetics are risk factors for insulin resistance.
- Chronic insulin resistance can lead to pancreatic beta-cell burnout, resulting in insufficient insulin production.
- Insulin sensitivity can be improved by weight loss, regular exercise, and certain medications.
Insulin and Diabetes: The Connection
Insulin dysfunction is fundamental to the development of two main forms of diabetes:5
- Type 1 Diabetes: An autoimmune process destroys pancreatic beta cells, leading to an absolute deficiency of insulin. Patients require lifelong insulin therapy.
- Type 2 Diabetes: The body gradually develops insulin resistance, combined with inadequate compensatory insulin secretion. Early stages can be managed with lifestyle changes and medications, though insulin is eventually required for many patients.
How Is Insulin Used as a Medication?
For people who lack the ability to make enough insulin (such as those with type 1 diabetes and many with type 2 diabetes), exogenous (external) insulin must be administered.2
- Injected subcutaneously (under the skin) using syringes, pens, or insulin pumps
- Different preparations: Rapid-acting, short-acting, intermediate-acting, and long-acting insulins
- Goal: Mimic the natural pattern of insulin secretion to achieve near-normal blood glucose levels
What Happens If You Don’t Have Enough Insulin?
A lack of insulin or failure of insulin action has serious health implications:
- High Blood Glucose (Hyperglycemia): Leads to symptoms such as excessive thirst, frequent urination, fatigue, and blurred vision
- Diabetic Ketoacidosis: Life-threatening complication due to breakdown of fats for fuel, producing acidic ketone bodies (mainly in type 1 diabetes)
- Chronic Complications: Damage to the eyes, kidneys, nerves, and blood vessels over time
Other Roles of Insulin in the Body
Besides glucose regulation, insulin is vital for overall metabolic health:
- Stimulates cell growth and DNA replication
- Promotes amino acid uptake for protein synthesis
- Modulates fat metabolism, encouraging storage and limiting breakdown
Insulin vs. Glucagon: A Balancing Act
Insulin isn’t the only hormone involved in glucose regulation. Its key counterpart, glucagon, is secreted by alpha cells in the pancreas. While insulin lowers blood glucose, glucagon raises it by stimulating glycogen breakdown and gluconeogenesis in the liver. The coordinated interplay of these two hormones maintains healthy glucose levels.1
Summary Table: Insulin’s Mechanism at a Glance
| Step | Process | Main Outcome |
|---|---|---|
| 1 | Glucose rises in blood | Stimulates pancreatic beta cells to release insulin |
| 2 | Insulin binds to target cells | Activates insulin receptor and intracellular signaling |
| 3 | Translocation of GLUT4 to plasma membrane | Increased glucose uptake into cells |
| 4 | Intracellular actions | Glycogen, protein, and fat synthesis; inhibition of breakdown |
Frequently Asked Questions (FAQs)
What triggers the release of insulin?
The main trigger for insulin release is a rise in blood glucose after eating. Certain amino acids and hormones, as well as neural signals, can also promote its release.1
What happens to glucose once insulin is active?
When insulin binds to receptors on muscle and fat cells, glucose is taken up from the blood and used for energy or stored as glycogen or fat, reducing blood sugar levels.3
What is insulin resistance?
Insulin resistance is a condition in which the body’s cells become less responsive to insulin, requiring higher insulin concentrations for glucose uptake. It is a central feature of type 2 diabetes.4
Do all tissues respond to insulin the same way?
No. While insulin strongly stimulates glucose absorption by muscle and fat, the liver’s uptake of glucose is less affected by insulin; however, insulin inhibits glucose production and release by the liver.2
Why is insulin important for people with diabetes?
For people with type 1 diabetes (and sometimes advanced type 2 diabetes), insulin therapy is necessary to achieve normal blood sugar levels and prevent complications.
What happens if insulin is too high?
Excess insulin can cause hypoglycemia (low blood sugar), which can lead to shakiness, confusion, fainting, and, in severe cases, seizures or coma. Tight glucose control is essential, especially for people taking insulin therapeutically.
References
- Insulin – Wikipedia.
- Insulin human: Uses, Interactions, Mechanism of Action – DrugBank.
- Insulin : mechanism of action and diabetes – YouTube.
- Mechanisms of Insulin Action and Insulin Resistance – PMC.
- Insulin Mechanism of Action: How Does It Work? – Healthline.
References
- https://en.wikipedia.org/wiki/Insulin
- https://go.drugbank.com/drugs/DB00030
- https://www.youtube.com/watch?v=6zvl_AGaSfM
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6170977/
- https://www.healthline.com/health/diabetes/insulin-mechanism-of-action
- https://my.clevelandclinic.org/health/body/22601-insulin
- https://www.osmosis.org/learn/Insulin:_Nursing_Pharmacology
Read full bio of medha deb












