Insulin and Glucagon: Balancing Blood Sugar for Health
Understanding how insulin and glucagon regulate blood sugar to maintain metabolic health and prevent complications.
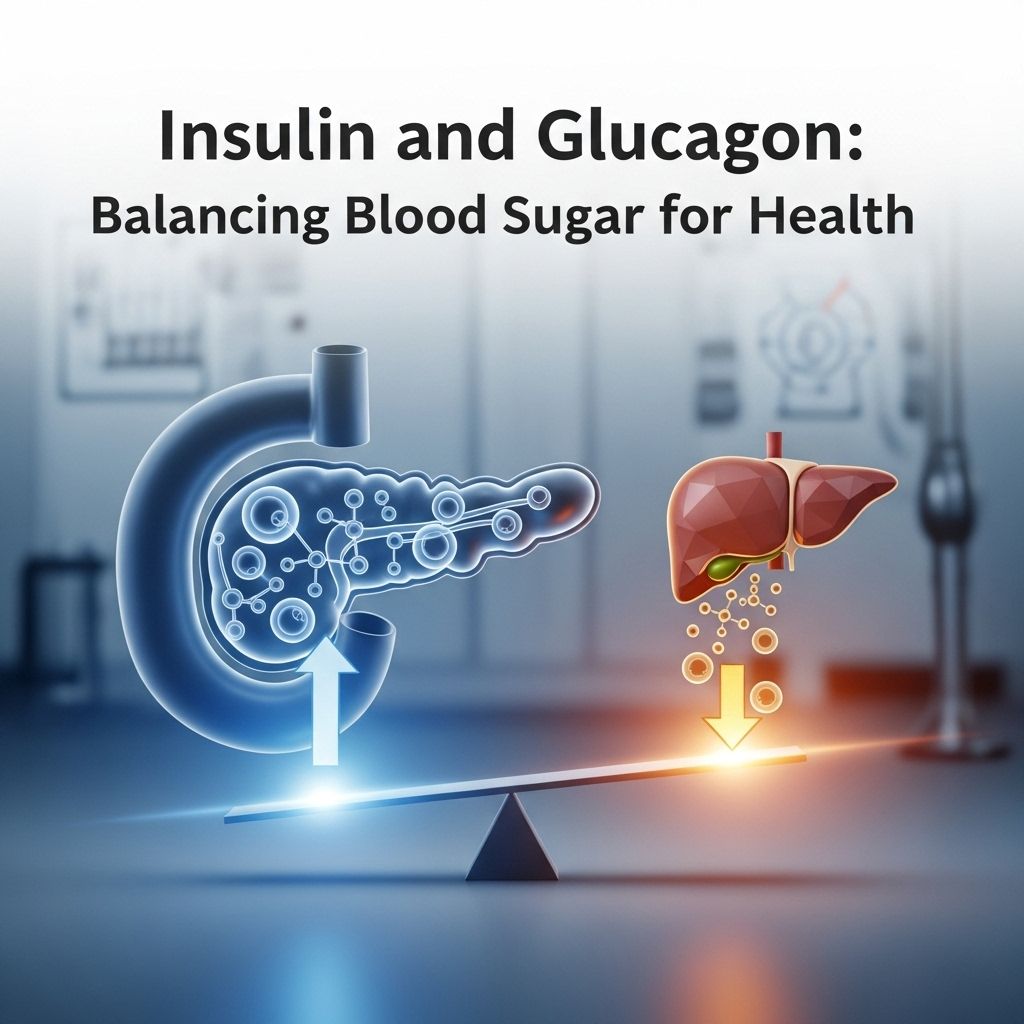
Insulin and Glucagon: The Twin Pillars of Blood Sugar Regulation
Maintaining balanced blood sugar is essential for overall energy, organ function, and long-term health. Two key hormones, insulin and glucagon, work in concert to keep blood glucose within a healthy range, ensuring your cells receive the energy they need while protecting against dangerous highs and lows.
How Insulin and Glucagon Work Together
Insulin and glucagon are both produced in the pancreas by different groups of cells. Beta cells release insulin, while alpha cells secrete glucagon.
- Insulin lowers blood sugar by signaling cells to absorb glucose from the blood.
- Glucagon raises blood sugar by prompting the liver to release stored glucose.
- Together, they maintain homeostasis, preventing persistent highs or lows that can harm the body.
When you eat carbohydrates, your body converts them into glucose. Some of this glucose is used immediately for energy, while excess is stored as glycogen in the liver and muscles. When more energy is needed, glucagon triggers the release of glucose from these stores, and insulin guides it into cells.
The Cycle of Blood Sugar Regulation
- If blood sugar rises after a meal: Insulin is released.
- If blood sugar drops (between meals, or after activity): Glucagon is released.
- The process repeats to maintain steady energy levels.
What Is Insulin?
Insulin is a hormone that enables glucose (sugar) in the bloodstream to enter your body’s cells. Without enough insulin or proper cell response, blood sugar remains high, which is damaging over time.
Functions of Insulin
- Moves glucose into cells for energy production.
- Helps store excess glucose as glycogen in the liver.
- Plays a role in breaking down fats and proteins for energy.
- Maintains healthy fat and protein metabolism.
Low levels of insulin are always present, but the pancreas secretes more after you eat, helping store glucose and prevent spikes in blood sugar.
If insulin levels are insufficient or cells become less responsive (insulin resistance), blood sugar remains elevated. This is the root cause of diabetes.
Types of Insulin (When Used as Medication)
| Type | Description | Duration |
|---|---|---|
| Rapid-acting | Starts working within minutes, peaks quickly. | 2 to 4 hours |
| Short-acting | Begins within 30 minutes, lasts longer than rapid type. | 3 to 6 hours |
| Intermediate-acting | Slower onset, prolonged action. | 12 to 18 hours |
| Long-acting | Stable, low-level effect for an extended period. | 16 to 24 hours |
- Choice of type depends on individual needs, blood sugar patterns, and doctor’s recommendation.
What Is Glucagon?
Glucagon is a hormone that acts as the body’s emergency sugar-raiser. When blood glucose is too low (hypoglycemia), glucagon signals the liver to convert stored glycogen back into glucose and release it into the bloodstream.
Key Functions of Glucagon
- Prevents dangerously low blood sugar.
- Triggers glycogenolysis (breakdown of glycogen in the liver).
- Promotes gluconeogenesis (production of glucose from non-carbohydrate sources).
- Helps maintain blood sugar between meals and during sleep.
When a person’s blood glucose drops (due to skipped meals, excess activity, or insulin error), glucagon steps in to rapidly restore safe levels.
How Insulin Works in the Body
After you eat, carbohydrates are broken down into glucose. This signals the pancreas to release insulin, which:
- Enables cells to absorb glucose for immediate energy or store it for later use as glycogen.
- Signals the liver to absorb excess glucose and convert it to glycogen, lowering blood sugar.
If insulin function is impaired, blood sugar remains high, leading to symptoms of diabetes and risk for long-term complications.
How Glucagon Works in the Body
Glucagon’s main role is defending against hypoglycemia. When blood sugar falls below a healthy threshold, the pancreas releases glucagon, which:
- Instructs the liver to break down glycogen and release glucose.
- Stimulates gluconeogenesis: making new glucose from other molecules as needed.
- Helps the kidneys and other organs boost glucose supply in emergencies.
This process is vital during sleep, fasting, or between meals.
Blood Sugar Levels: How They Fluctuate and Are Controlled
Your blood sugar levels naturally vary through the day, but remain within a narrow range thanks to insulin and glucagon. Their balance keeps you energized while protecting against the negative consequences of too high or too low glucose.
| State | Hormone Released | Effect |
|---|---|---|
| After Eating | Insulin | Absorbs glucose, lowers blood sugar |
| Between Meals | Glucagon | Releases stored glucose, raises blood sugar |
| During Exercise | Glucagon (& Insulin adjusts) | Prevents hypoglycemia, supplies energy |
| Sleep/Fasting | Glucagon | Keeps glucose available for vital organs |
- High blood sugar (hyperglycemia) results if not enough insulin is present, risking organ damage over time.
- Low blood sugar (hypoglycemia) occurs when insulin levels are excessive or intake/activity don’t match, risking faintness, seizures, or worse.
Diabetes: The Impact of Imbalanced Insulin and Glucagon
Diabetes develops if the control systems for blood sugar break down.
- Type 1 diabetes: The immune system destroys pancreatic beta cells, stopping insulin production. Patients must rely on external insulin to survive.
- Type 2 diabetes: Cells become resistant to insulin or there’s a shortfall in the amount produced. This leads to persistent high blood sugar and related health problems.
In both cases, insulin replacement is key. Glucagon may also be required for emergency treatment of severe lows.
Chronic High Blood Sugar: Risks and Complications
- Damage to eyes, kidneys, nerves, and blood vessels.
- Increased risk of heart attacks and strokes.
- Slower healing and risk of infections.
Low Blood Sugar: Recognizing and Managing Hypoglycemia
- Symptoms include shakiness, confusion, sweating, dizziness, and fainting.
- Severe hypoglycemia can lead to seizures, unconsciousness, or death.
- Rapid treatment is critical: for emergencies, glucagon injection is effective and life-saving.
Those taking insulin should always have glucagon available as a rescue medication for sudden severe lows.
Using Prescription Insulin and Glucagon: What You Need to Know
Insulin Treatment
- Dose and delivery vary by individual and daily needs.
- Requires careful monitoring and coordination with healthcare providers.
- Too much or too little can trigger dangerous blood sugar swings.
Patients should follow their treatment plans meticulously to prevent both hyperglycemia and hypoglycemia.
Glucagon for Emergencies
- Glucagon is fast-acting and reserved for severe hypoglycemia, often when a patient cannot consume glucose by mouth.
- Should be part of every household emergency plan for anyone using insulin.
- Caregivers and patients should learn how to administer it and ensure it’s stored properly.
Managing Blood Sugar: Lifestyle Tips
- Eat regular, balanced meals to prevent sugar spikes and valleys.
- Monitor blood glucose as directed by your healthcare provider.
- Be physically active—exercise improves insulin sensitivity.
- Carry fast-acting carbohydrates for mild lows, and glucagon for severe emergencies.
- Discuss your medication options and safety plans with your doctor.
Making glucagon part of everyday preparedness is increasingly recommended by diabetes specialists and advocates.
Frequently Asked Questions
Q: How do insulin and glucagon interact to control blood sugar?
A: Insulin lowers blood sugar by helping cells absorb glucose; glucagon raises it by telling the liver to release stored sugar. Together they keep levels steady.
Q: Who needs to carry glucagon?
A: Anyone who uses insulin, especially those with type 1 diabetes or type 2 diabetes requiring insulin, should carry glucagon in case of severe hypoglycemia.
Q: What are the signs of high or low blood sugar?
High blood sugar (hyperglycemia) can cause thirst, frequent urination, and blurry vision.
Low blood sugar (hypoglycemia) causes shakiness, confusion, sweating, dizziness, and can be life-threatening.
Q: Can changing diet help insulin function?
A: Yes. Eating balanced meals with non-starchy vegetables, whole grains, and healthy fats can help manage insulin levels and sensitivity.
Q: How do people with diabetes use insulin and glucagon?
A: Insulin is used daily for blood sugar control. Glucagon is used only in emergencies for severe lows, as a fast-acting antidote to hypoglycemia.
Summary Table: Insulin vs. Glucagon
| Aspect | Insulin | Glucagon |
|---|---|---|
| Main function | Lowers blood sugar | Raises blood sugar |
| Origin (pancreas cells) | Beta cells | Alpha cells |
| Effect on liver | Stores glucose as glycogen | Releases glucose from glycogen |
| Role in diabetes | Controls everyday glucose levels | Emergency rescue from lows |
Key Takeaways
- Insulin and glucagon are critical hormones for blood sugar control.
- Disruptions in their balance lead to diabetes and other health risks.
- Insulin is central to daily management; glucagon is vital for emergencies.
- Lifestyle, diet, and medication come together for effective blood sugar management.
- Talk to your healthcare provider about insulin, glucagon, and personalized strategies to prevent complications.
References
- https://www.medicalnewstoday.com/articles/316427
- https://beyondtype1.org/glucagon-diabetes-hypoglycemia-safety/
- https://www.medicalnewstoday.com/articles/323760
- https://www.healthline.com/health/type-2-diabetes/insulin
- https://www.healthline.com/health/video/the-complete-guide-to-insulin-and-how-to-use-it
- https://pmc.ncbi.nlm.nih.gov/articles/PMC1204764/
- https://medlineplus.gov/bloodglucose.html
- https://my.clevelandclinic.org/health/diseases/7104-diabetes
Read full bio of Sneha Tete












