Injections for Macular Degeneration: Treatment, Effectiveness, and Risks
Explore how injections for age-related macular degeneration help slow vision loss, what to expect during treatment, and important safety considerations.
Injections for Macular Degeneration: Options, Effectiveness, and Safety
Age-related macular degeneration (AMD) is a leading cause of vision loss, particularly in older adults. While there are two primary forms—dry and wet AMD—it is the wet type that most often requires intravitreal injections as a primary treatment. Recent medical advances, especially anti-VEGF injections, have revolutionized the management of this disease, helping to slow or even prevent the progression of vision loss.
Read on to understand the available options, details of the injection procedure, effectiveness, possible risks, and answers to common questions about injections for macular degeneration.
Understanding Macular Degeneration and Injections
Macular degeneration is a chronic, progressive eye condition primarily affecting the central portion of the retina, known as the macula. The two types are:
- Dry AMD: The more common and less severe form, typically managed with lifestyle changes, nutritional supplements, and newer injectable options.
- Wet AMD: Characterized by abnormal blood vessel growth beneath the macula that can leak or bleed, leading to rapid vision loss if untreated. This form is commonly treated with injections.
Why Injections?
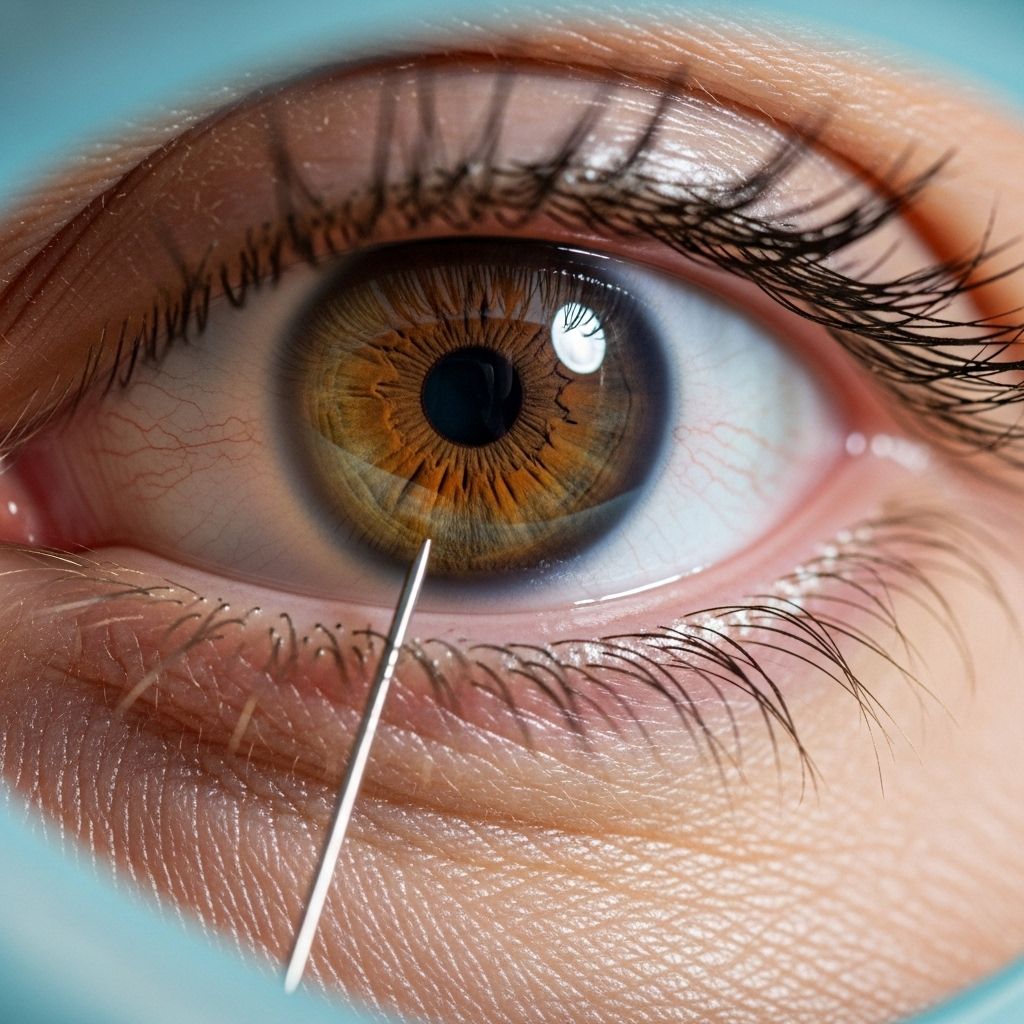
Intravitreal injections—those delivered directly into the eye’s vitreous humor—are mainly used to deliver anti-VEGF medications. VEGF, or vascular endothelial growth factor, is a protein that promotes the growth of abnormal blood vessels. By inhibiting VEGF, these drugs slow or prevent further vessel growth and leakage.
About Anti-VEGF Injections
Anti-VEGF therapy revolutionized the management of wet AMD. These medications work by blocking VEGF activity and have demonstrated strong evidence in slowing vision loss and, in some cases, improving vision. Some anti-VEGF drugs are also now approved for select cases of dry AMD as research advances.
Common Anti-VEGF Medications
- Ranibizumab (Lucentis®)
- Aflibercept (Eylea®)
- Brolucizumab (Beovu®)
- Bevacizumab (Avastin®) – used “off label” for AMD but widely accepted by experts
Each drug has its own dosing schedule, characteristics, and relative cost, but they all target VEGF-driven vessel growth.
Expanding Medication Options
- Ranibizumab and aflibercept: FDA-approved for wet AMD, injected usually every 4–8 weeks, with treatment intervals adjusted over time.
- Brolucizumab: Newer option, sometimes dosed every 8–12 weeks after three initial monthly doses.
- Bevacizumab (Avastin): Off-label for AMD, often used due to lower cost, similar clinical effectiveness.
- Emerging therapies: Some newer drugs and extended-release delivery systems may allow for less frequent injections.
The Injection Procedure: What to Expect
The idea of an eye injection can understandably cause anxiety, but in expert hands, the procedure is quick and is generally painless or causes only mild discomfort. Here’s what typically happens:
- Anesthetic eye drops numb the surface of the eye to prevent pain.
- Cleaning with antiseptic minimizes the risk of introducing infection.
- An eyelid speculum is gently inserted to keep your eyelids open and prevent blinking during the procedure.
- You are instructed to look away from the area where the injection will be given.
- The injection is administered through the sclera (white of the eye) into the vitreous cavity. This step takes only a few seconds.
- The doctor rinses the injection site with saline and may lubricate the eye afterwards.
After the Injection
- Most people experience little to no pain during or after the procedure.
- Some report mild discomfort, a sensation of grittiness, or temporary redness near the injection site.
- Rarely, small spots of bleeding may be seen on the eye, which usually resolve on their own.
- You can resume normal activities shortly after the visit, typically with only minor restrictions suggested by your eye care provider.
Injection Frequency
The frequency of injections depends on the drug, severity of disease, and individual response. Most regimens start with monthly or bi-monthly injections; over time, if the condition stabilizes, the intervals may be extended. Some patients may eventually be able to stop injections or shift to less frequent dosing based on close monitoring of their condition.
How Effective Are Injections for Macular Degeneration?
Anti-VEGF injections are considered the most effective therapy for the majority of wet AMD cases. Efficacy depends on early diagnosis, consistent treatment, and individual factors. Key points include:
- Improved or stabilized vision in approximately one-third of people receiving regular injections.
- Prevention of further vision loss in up to 90% of treated wet AMD cases.
- Some people with dry AMD may benefit from newer injectable therapies designed to slow atrophy, but most data support use in wet AMD.
- The potential for partial vision recovery in select individuals, although improvement is not guaranteed.
Regular monitoring with eye exams and retinal imaging is essential, as further treatment or adjustments may be needed to maintain or maximize visual results.
Risks and Potential Complications
While generally safe and well tolerated, intravitreal injections do carry certain risks, which include:
- Minor discomfort or irritation as the anesthetic wears off.
- Subconjunctival hemorrhage: Localized bleeding or redness on the white of the eye, usually harmless and temporary.
- Infection (endophthalmitis): A rare but serious complication (less than 0.1% per injection) that requires urgent medical attention; symptoms include persistent pain, increasing redness, and vision changes.
- Traumatic cataract: Rare, may occur if the lens is inadvertently injured during injection.
- Retinal tears or detachment: Extremely rare but possible.
- Inflammation or allergic reaction to medication, also very uncommon.
Overall, the benefits of treatment typically far outweigh the risks for people with active wet AMD. Your eye doctor will review possible complications and how to monitor for warning signs after each injection.
Care After Injections and When to Call a Doctor
- Minor grittiness, mild soreness, or redness is common for a day after the procedure and typically resolves without treatment.
- Artificial tears may help soothe mild irritation.
- Do not rub your treated eye after injection.
- Seek prompt medical attention if you experience severe pain, sudden decrease in vision, marked redness, or discharge.
Follow-up appointments are essential to monitor efficacy and safety, and to determine the frequency of future injections based on your response.
Can You Stop Eye Injections for Macular Degeneration?
While consistent anti-VEGF therapy is important for controlling AMD, not all patients will need injections indefinitely. Stopping injections might be possible in select cases, especially with close monitoring. Recent research described a treat-extend-stop protocol:
- Injections are spaced out more gradually if the disease remains stable without new fluid or bleeding.
- Once stable for several cycles, injections may be paused, but regular monitoring continues.
- Approximately 30–37% of patients could safely stop injections, though this should always be guided by a retina specialist and not attempted on your own.
- If new signs of activity develop, treatment can be resumed, often regaining previously stabilized vision.
Your care team may also look for specific markers in eye fluid or retinal imaging to help determine when injections might be safely reduced or stopped.
Frequently Asked Questions (FAQs)
Q: Who is eligible for anti-VEGF injections for macular degeneration?
A: These injections are primarily recommended for people with active wet AMD showing evidence of abnormal blood vessel growth or leakage. Some newer injectable therapies may be used in dry AMD under certain conditions. Those with advanced AMD and severe vision loss may benefit less.
Q: What should I expect during my first injection?
A: Your eye will be numbed, cleansed, and stabilized with a small speculum. You will be asked to look away, and the doctor will quickly administer the injection. Most patients report little or no pain.
Q: Are these injections safe in the long run?
A: Long-term safety data are reassuring. While rare complications like infection or bleeding can occur, routine precautions and follow-up significantly minimize risk.
Q: What are signs of a complication after injection?
A: Sudden vision loss, severe persistent eye pain, increasing redness, or discharge from the eye require urgent medical evaluation to rule out serious problems such as infection.
Q: Can I stop my injections if my vision is stable?
A: Never stop injections on your own. Your ophthalmologist may gradually reduce frequency if your condition remains stable, and may consider a carefully supervised stop protocol after monitoring. Even after stopping, ongoing checkups are needed to catch recurrences early.
Key Takeaways
- Anti-VEGF injections are the standard of care for wet macular degeneration and can also benefit certain dry AMD cases.
- Modern therapies can slow, stop, or in some cases reverse vision loss if started early and administered regularly.
- The injection procedure is quick, safe, and minimally painful for most people when performed by a trained specialist.
- Risks are low but include infection, minor bleeding, and rare complications; knowing warning signs is important.
- With advances in medication and personalized approaches, some people may ultimately require less frequent injections or be able to stop, with close supervision.
When to Consult a Specialist
If you are over age 50 and notice changes in your central vision, blurriness, or distortion, schedule a comprehensive dilated eye exam promptly. Early diagnosis and proactive treatment are crucial for preserving sight in AMD. If you have been diagnosed with macular degeneration and are anxious or have questions about injections, talk openly with your retina specialist—they can offer detailed information specific to your situation and help you make the best decisions for your long-term vision.
References
- https://www.healthline.com/health/eye-health/injections-for-macular-degeneration
- https://www.healthline.com/health/what-happens-if-you-stop-eye-injections-for-macular-degeneration
- https://www.brightfocus.org/resource/injections-for-wet-macular-degeneration-what-you-need-to-know/
- https://www.medicalnewstoday.com/articles/injections-for-macular-degeneration
- https://theretinainstitute.org/macular-degeneration
- https://www.medicalnewstoday.com/articles/wet-macular-degeneration-treatment
- https://www.nvisioncenters.com/macular-degeneration/treatment-breakthroughs/
Read full bio of medha deb












