Inflammatory Glaucoma: Causes, Symptoms, and Treatment
Understand inflammatory glaucoma—a type linked to uveitis—including causes, symptoms, risk factors, and the latest treatments.
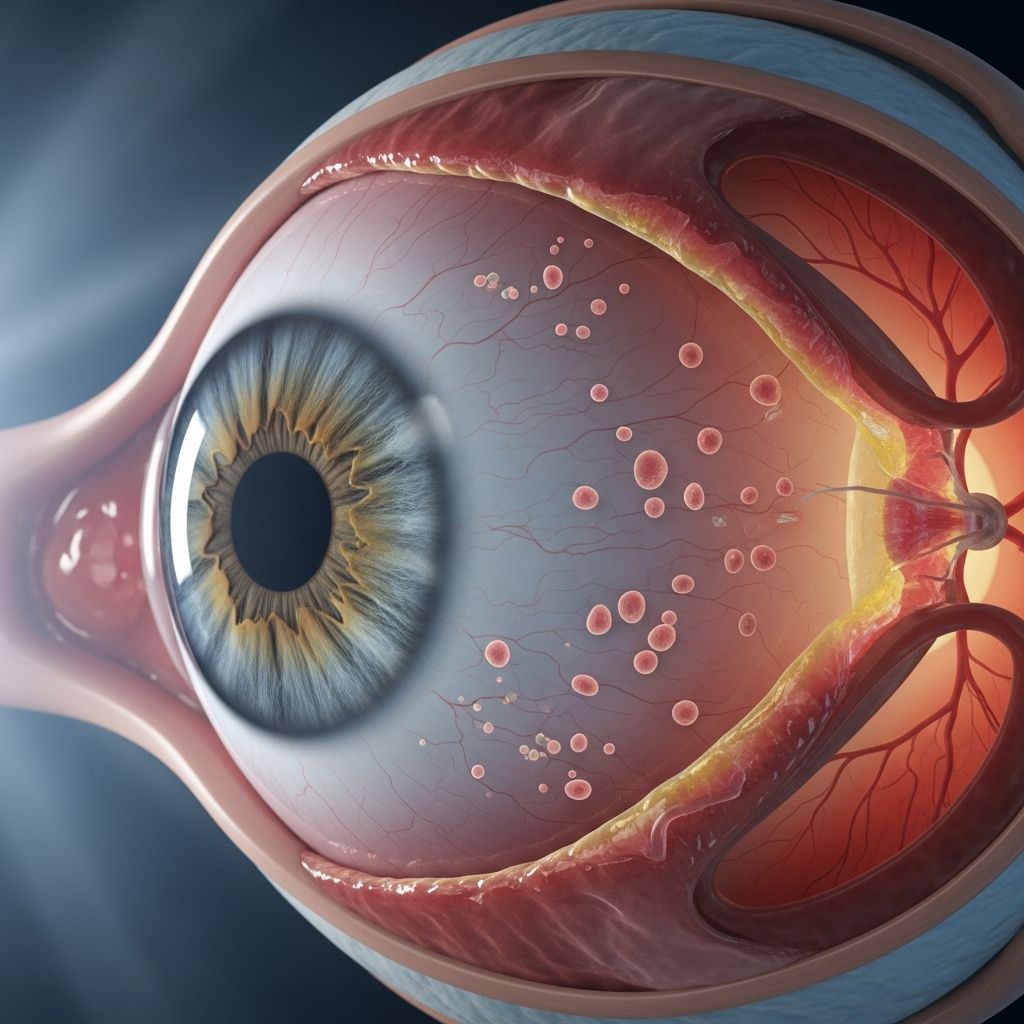
Inflammatory glaucoma—often called uveitic glaucoma—is a distinct yet serious type of glaucoma that results from intraocular inflammation. This condition can threaten vision due to elevated eye pressure and inflammation-induced damage, so early recognition and treatment are critical.
What Is Inflammatory Glaucoma?
Inflammatory glaucoma is a form of secondary glaucoma that develops as a direct consequence of uveitis, an inflammatory process affecting the uveal tract of the eye (iris, ciliary body, and choroid). The inflammation disrupts normal fluid dynamics within the eye, leading to increased intraocular pressure (IOP) and characteristic damage to the optic nerve.
- Also known as uveitic glaucoma.
- Most often develops in one eye but can affect both.
- Elevated IOP can be persistent or fluctuate with the course of inflammation.
Symptoms of Inflammatory Glaucoma
Symptoms can vary widely in their onset and severity. Some people may experience mild, gradual symptom development, while others might notice sudden and severe changes. Recognizing symptoms early is vital for prompt intervention.
Early Symptoms
- Eye redness
- Sensitivity to light (photophobia)
- Blurry vision
- Eye pain
- Eye floaters (seeing small shapes drifting in your field of vision)
- Mild vision loss
Progressive and Severe Symptoms
- Severe eye pain
- Headaches
- Nausea and vomiting (when eye pressure rises rapidly)
- Halos around lights
- Blind spots in the visual field
- Loss of peripheral (side) vision
- Significant or complete vision loss
Symptoms may affect one or both eyes. Fluctuations are common, especially as inflammation relapses or is treated.
Causes and Risk Factors
Inflammatory glaucoma arises specifically from inflammation in the eye, most commonly uveitis. However, the underlying triggers for the inflammation are diverse.
Common Causes
- Infections (e.g., herpes simplex virus, cytomegalovirus, tuberculosis, toxoplasmosis)
- Autoimmune conditions such as sarcoidosis, rheumatoid arthritis, or lupus
- Eye injuries or trauma
- Complications from eye surgery
- Idiopathic (in some cases, the specific inflammatory cause is unknown)
How Inflammation Leads to Glaucoma
Under normal circumstances, fluid (aqueous humor) produced in the eye drains out smoothly, keeping IOP at healthy levels. Inflammatory processes can disrupt this balance by:
- Blocking or clogging the eye’s drainage angle with inflammatory cells and debris
- Altering the normal composition of eye fluid, making it harder to drain
- Scar tissue formation at the drainage site, permanently decreasing outflow
- Drug-induced increases in eye pressure (some corticosteroids used to treat inflammation can paradoxically raise IOP)
Diagnosis
Diagnosis of inflammatory glaucoma requires careful assessment by an eye care professional. The process usually involves a combination of examination techniques, imaging, and laboratory tests.
- Comprehensive eye exam — Checks for redness, swelling, inflammatory signs, and measures of IOP.
- Gonioscopy — Special lens is used to examine the eye’s drainage angle for clogging or scarring.
- Slit lamp examination — Detects inflammatory cells and debris floating inside the front chamber of the eye.
- Visual field test — Detects damage to peripheral vision associated with glaucoma.
- Optical coherence tomography (OCT) — Measures thickness of the optic nerve and retinal layers to assess damage.
- Lab tests — May be performed to identify underlying infections or autoimmune diseases.
Possible Complications of Inflammatory Glaucoma
Without timely intervention, inflammatory glaucoma can lead to several serious complications, many of which are vision-threatening:
- Permanent vision loss
- Chronic eye pain
- Cataract formation (clouding of the eye’s lens)
- Retinal damage
- Scarring and distortion of eye tissues
- Secondary infections
Prompt and effective treatment greatly improves the outlook for most people diagnosed with this condition.
Treatment Options
Treatment of inflammatory glaucoma addresses both the inflammation (underlying uveitis) and the elevated intraocular pressure. The management plan is often multifaceted, and may include medications, interventions, and/or surgery.
Medications
- Anti-inflammatory medications: Topical corticosteroids (eye drops), oral steroids, or immunosuppressive drugs are used to control inflammation. If an infection is present, anti-infective medications are needed instead of steroids.
- Intraocular pressure-lowering drops: Several classes of medicated eye drops (beta-blockers, alpha agonists, prostaglandin analogs, carbonic anhydrase inhibitors) reduce the production of fluid or increase its outflow.
- Antibiotics or antivirals: Prescribed if an infectious cause, such as herpes virus or tuberculosis, is identified.
- Immunosuppressive drugs: Used in cases of autoimmune uveitis to prevent further inflammatory attacks.
Procedures and Surgery
- Laser therapy: Laser trabeculoplasty or iridotomy may be performed to improve eye fluid drainage.
- Surgical drainage procedures: In cases where pressure remains high despite medication, a glaucoma drainage device or conventional glaucoma surgery (trabeculectomy) may be required.
- Implantation of shunts: Tiny tubes may be implanted to help excess fluid drain away from the eye.
- Cataract surgery: Sometimes indicated if cataracts develop due to chronic inflammation or corticosteroid use.
| Treatment | Purpose | Risks/Considerations |
|---|---|---|
| Topical steroids | Reduce inflammation | May cause IOP elevation, cataract formation |
| Glaucoma drops | Lower intraocular pressure | Potential side effects, sometimes less effective if inflammation severe |
| Surgery | Long-term control when other methods fail | Infection, scarring, risk of vision loss, prolonged healing |
| Antibiotics/Antivirals | Treat underlying infection | Side effects depend on agent, only effective if infectious cause |
| Immunosuppressants | Control autoimmune inflammation | Systemic side effects, increased infection risk |
Managing and Living With Inflammatory Glaucoma
Successful management of inflammatory glaucoma requires a collaborative approach between patient and healthcare team. Regular follow-ups and adherence to therapy are essential to preserve vision and quality of life.
Self-Care and Monitoring
- Take all medications exactly as prescribed—missing doses increases risk of vision loss.
- Attend all scheduled eye exams, even if vision is stable.
- Report sudden changes in vision, new eye pain, or side effects to your doctor immediately.
- Maintain a medical diary to track symptoms, medications, and flare-ups for ongoing care coordination.
Frequently Asked Questions (FAQs)
What is the difference between inflammatory glaucoma and primary glaucoma?
Inflammatory glaucoma (uveitic glaucoma) is caused by intraocular inflammation that raises eye pressure, while primary glaucomas develop without prior inflammation and often have a genetic or age-related background.
Can inflammatory glaucoma be cured?
While the underlying inflammation can often be treated or controlled, the optic nerve damage from glaucoma is usually permanent. Early intervention reduces the risk of vision loss and other complications.
Are there lifestyle changes to help control inflammatory glaucoma?
Medication adherence and regular follow-ups are key. Maintaining overall health (controlling underlying autoimmune disease, managing infections promptly) supports better outcomes, but lifestyle changes alone can’t reverse the condition.
Can children get inflammatory glaucoma?
Yes. Children, particularly those with juvenile idiopathic arthritis or other systemic inflammatory diseases, can develop this type of glaucoma.
Is vision loss from inflammatory glaucoma reversible?
Vision loss from glaucoma is usually not reversible, but timely diagnosis and aggressive management can prevent further damage.
Key Takeaway
Inflammatory glaucoma is a vision-threatening complication of eye inflammation that can affect anyone. Early recognition of symptoms—such as eye pain, redness, blurry vision, and floaters—makes a significant difference. Modern ophthalmic therapy can preserve vision in most cases if started promptly and managed carefully.
References
- https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1577200/full
- https://www.healthline.com/health/eye-health/inflammatory-glaucoma
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3110445/
- https://www.healthline.com/health/glaucoma
- https://www.medicalnewstoday.com/articles/248423
- https://www.healthline.com/health/video/how-to-get-rid-of-bags-under-eyes
- https://www.healthline.com/health/video/can-anti-inflammatory-foods-ease-menopause-joint-pain
- https://www.britannica.com/science/uveitis
- https://en.wikipedia.org/wiki/Uveitic_glaucoma
Read full bio of Sneha Tete












