Inflammatory Bowel Disease: Understanding Causes, Symptoms, and Management
A comprehensive guide to inflammatory bowel disease exploring its causes, symptoms, diagnosis, and modern treatment options.
Inflammatory Bowel Disease (IBD): Comprehensive Overview
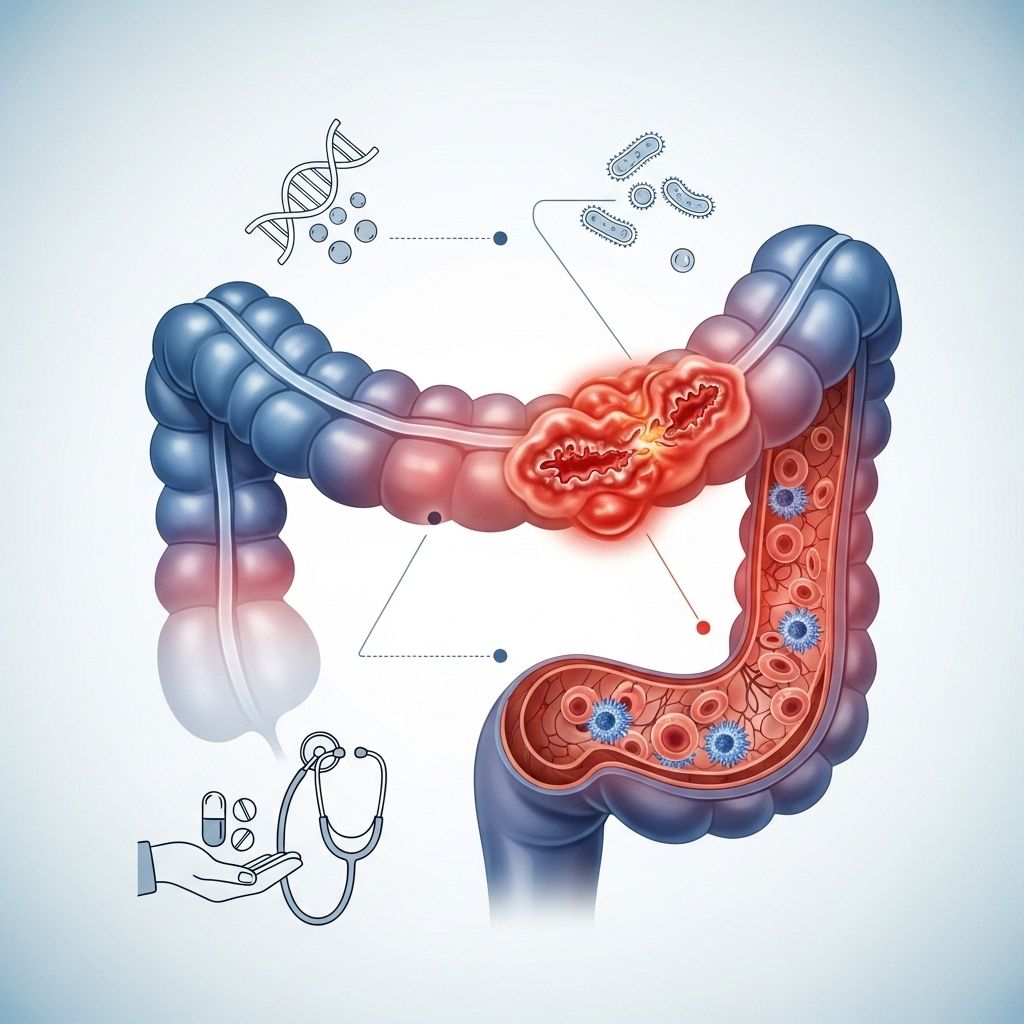
Inflammatory Bowel Disease (IBD) refers to a group of chronic disorders characterized by inflammation of the gastrointestinal (GI) tract. The two main types of IBD are Crohn’s disease and ulcerative colitis, each with distinct clinical features, causes, and treatment approaches. This article provides an in-depth look at IBD, covering causes, symptoms, diagnosis, treatment options, and quality of life considerations.
What is Inflammatory Bowel Disease?
IBD is not a single disease but a term that encompasses chronic inflammatory conditions of the digestive tract, most commonly Crohn’s disease and ulcerative colitis. Both disorders involve persistent inflammation but differ in their specific locations and patterns within the GI tract.
- Crohn’s disease: Can affect any part of the GI tract, from mouth to anus, commonly impacting the terminal ileum and colon. Inflammation can be patchy and may extend through several layers of the bowel wall.
- Ulcerative colitis: Primarily affects the colon and rectum, causing continuous areas of inflammation restricted to the innermost lining of the bowel wall.
Key Differences Between Crohn’s Disease and Ulcerative Colitis
| Feature | Crohn’s Disease | Ulcerative Colitis |
|---|---|---|
| Location | Any part of GI tract | Colon and rectum only |
| Inflammation pattern | Patchy, transmural | Continuous, mucosal |
| Symptoms | Abdominal pain, diarrhea, weight loss | Bloody diarrhea, urgency |
| Complications | Abscesses, fistulas, strictures | Toxic megacolon, colon cancer risk |
Causes and Risk Factors of IBD
The precise cause of IBD is unknown. Current research suggests that several factors contribute to its development:
- Genetic predisposition — Family history of IBD increases risk.
- Immune system dysfunction — Overactive or inappropriate immune responses cause chronic inflammation.
- Intestinal microbiota imbalance — Changes in gut bacteria can trigger inflammation.
- Environmental and lifestyle factors — Diet, smoking, stress, and certain medications may play a role.
The interplay between these factors leads to an abnormal immune reaction against normal components of the gut, driving ongoing inflammation and tissue damage.
Common Symptoms of IBD
Symptoms vary depending on the type and severity of the disease, but the most frequent include:
- Abdominal pain and cramping
- Chronic diarrhea (often bloody in ulcerative colitis)
- Urgency to have a bowel movement
- Rectal bleeding
- Weight loss and fatigue
- Reduced appetite
Extra-intestinal symptoms may also develop, such as skin rashes, joint pain, eye inflammation, and even liver problems, reflecting the systemic nature of IBD.
Complications of IBD
IBD can lead to serious complications over time, including:
- Obstruction or strictures: Narrowing of the bowel from scar tissue
- Perforation: Hole in the intestinal wall leading to infection
- Abscesses: Collections of pus within the abdomen
- Fistulas: Abnormal connections between organs
- Increased risk of colorectal cancer: Particularly in long-standing ulcerative colitis
- Toxic megacolon: Acute, life-threatening colon dilation in ulcerative colitis
Diagnosis of Inflammatory Bowel Disease
The diagnosis combines clinical history, physical examination, and various tests:
- Blood tests: Assess anemia, inflammation, and infection markers.
- Stool tests: Screen for infection and signs of inflammation.
- Endoscopy and Colonoscopy: Direct visualization and biopsy of affected areas.
- Imaging studies: CT or MRI scans to evaluate extent and complications.
Treatment Options for IBD
IBD treatment aims to control inflammation, relieve symptoms, improve quality of life, and minimize complications. Therapy is tailored to disease type, severity, and patient response.
Pharmacological Therapies
- Aminosalicylates (5-ASA): Reduce inflammation, especially in ulcerative colitis.
- Corticosteroids: Powerful anti-inflammatory drugs used for active flares; not suitable for long-term use due to side effects.
- Immunomodulators: Suppress the immune system to prevent flare-ups (azathioprine, 6-mercaptopurine).
- Biologics: Target specific inflammatory molecules (e.g., TNF inhibitors like infliximab, adalimumab).
- Small molecule therapies: Newer drugs targeting unique pathways.
Non-Pharmacological Treatments
- Diet and Nutrition: Individualized dietary changes can help manage symptoms and avoid malnutrition.
- Lifestyle modifications: Stress management, regular exercise, and quitting smoking are beneficial.
- Psychological support: Counseling or support groups can help cope with the chronic nature of IBD.
Surgical Interventions
- Resection of diseased bowel: Surgical removal may be needed for severe cases, complications, or cancer risk.
- Proctocolectomy: Complete removal of colon and rectum in some cases, often followed by creation of an ileal pouch.
- Drainage of abscesses or repair of fistulas: Procedures to address acute complications.
Surgery does not cure Crohn’s disease, as inflammation may recur in other segments, but ulcerative colitis can often be completely cured with removal of the colon.
Emerging Therapies and Research Advances
- Gut-restricted drugs: New compounds targeting intestinal inflammation without widespread immune suppression, such as novel gut enzyme inhibitors.
- Microbiome-targeted therapies: Use of probiotics, prebiotics, synbiotics, and fecal microbiota transplantation (FMT) to restore healthy gut bacteria.
- Cell and exosome therapy: Investigational approaches focused on modulating immune responses.
Research continues to identify new targets and personalized approaches, aiming for better symptom control and long-term mucosal healing.
Improvement of Intestinal Microecology
Understanding and manipulating the gut microbiome has become a major area of IBD research. Data show that patients with IBD have decreased biodiversity of intestinal flora, especially a reduction in beneficial anaerobic bacteria such as Bacteroides, Eubacteria, and Lactobacilli. Loss of these protective bacteria contributes to mucosal injury and chronic inflammation.
- Antibiotics: Target harmful bacteria during acute flares and complications.
- Probiotics and Prebiotics: Support restoration of beneficial bacterial populations.
- Synbiotics: Combine probiotics and prebiotics for synergistic effects.
- Fecal Microbiota Transplantation (FMT): Transfer of healthy donor stool to repopulate gut bacteria, showing promise in certain stubborn IBD cases.
Living with IBD: Quality of Life Considerations
IBD is typically a lifelong disease requiring ongoing medical management. Key issues affecting patients include:
- Unpredictable symptoms (abdominal pain, diarrhea, incontinence)
- Dietary restrictions and nutritional challenges
- Psychosocial stress and anxiety
- Impact on daily activities and social/family life
- Medication side effects
Maintaining remission and minimal symptom activity is central to improving and preserving quality of life. Effective communication with healthcare providers and rapid response to side effects are crucial for long-term well-being. Support networks and mental health resources can provide valuable assistance and hope.
Frequently Asked Questions (FAQs)
Q: Is IBD the same as IBS?
A: No, they are different conditions. IBD involves chronic inflammatory changes to the bowel, while IBS (Irritable Bowel Syndrome) is a functional disorder without inflammation or anatomical changes.
Q: Can diet alone cure IBD?
A: While diet modifications can reduce symptom severity and improve nutritional status, they do not cure IBD. Medical and sometimes surgical interventions are often necessary.
Q: What are the early warning signs of IBD?
A: Common early signs include persistent abdominal pain, diarrhea, blood in the stool, sudden weight loss, and fatigue. If these symptoms occur, medical evaluation is advised.
Q: Does IBD increase cancer risk?
A: Yes. Chronic inflammation, especially in ulcerative colitis involving the whole colon, increases the long-term risk of colorectal cancer. Regular screening is recommended.
Q: Are biologic therapies safe for long-term use?
A: Biologic therapies can provide effective control of IBD but may carry risks such as infection and rarely, malignancy. Regular monitoring by a specialist is essential.
Summary: Navigating Inflammatory Bowel Disease
Inflammatory Bowel Disease is a complex, chronic condition requiring multidisciplinary management. Advances in medications, microbiome research, and personalized care continue to offer hope for improved outcomes and better quality of life. For those living with IBD, regular medical care, healthy lifestyle choices, and supportive resources are key to controlling symptoms and minimizing complications.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8720971/
- https://ventures.jhu.edu/news/johns-hopkins-researchers-develop-gut-restricted-drug-to-treat-ibd/
- https://www.youtube.com/watch?v=Me9H1-EyFQk
- https://www.youtube.com/watch?v=rduQXkqYA_Q
- https://academic.oup.com/ibdjournal/article-abstract/29/Supplement_1/S34/7005563
Read full bio of medha deb












