Immunotherapy for Small Cell Lung Cancer: How It Works, Effectiveness, and What to Expect
A comprehensive guide to the use of immunotherapy for treating small cell lung cancer, its mechanisms, effectiveness, and patient considerations.
Small cell lung cancer (SCLC) constitutes about 13 615% of all lung cancer cases and is characterized by its rapid growth, early spread, and strong association with tobacco use1. Traditional treatments like chemotherapy and radiation have long been mainstays, but immunotherapy has emerged as a promising new avenue 6especially for advanced or extensive-stage disease1.
Understanding Small Cell Lung Cancer
SCLC is aggressive and more likely to spread early compared to non-small cell lung cancer (NSCLC). The aggressive nature of SCLC often makes early intervention vital, but treatment options have historically been limited.
- Incidence: 13 615% of all lung cancers
- Main Risk Factor: Smoking (linked to about 85% of all lung cancers including SCLC)
Common Treatment Approaches for SCLC
Six standard treatment methods are commonly deployed, often in combination, depending on the cancers stage:
- Surgery
- Chemotherapy (most common, often first-line)
- Radiation therapy (often combined with chemotherapy)
- Immunotherapy (an advancing option, especially in extensive-stage SCLC)
- Laser therapy
- Endoscopic stent placement
Chemotherapy and radiation therapy remain the most widely used first-line treatments1. Immunotherapy is commonly considered when other therapies are not effective or for use alongside standard treatments.
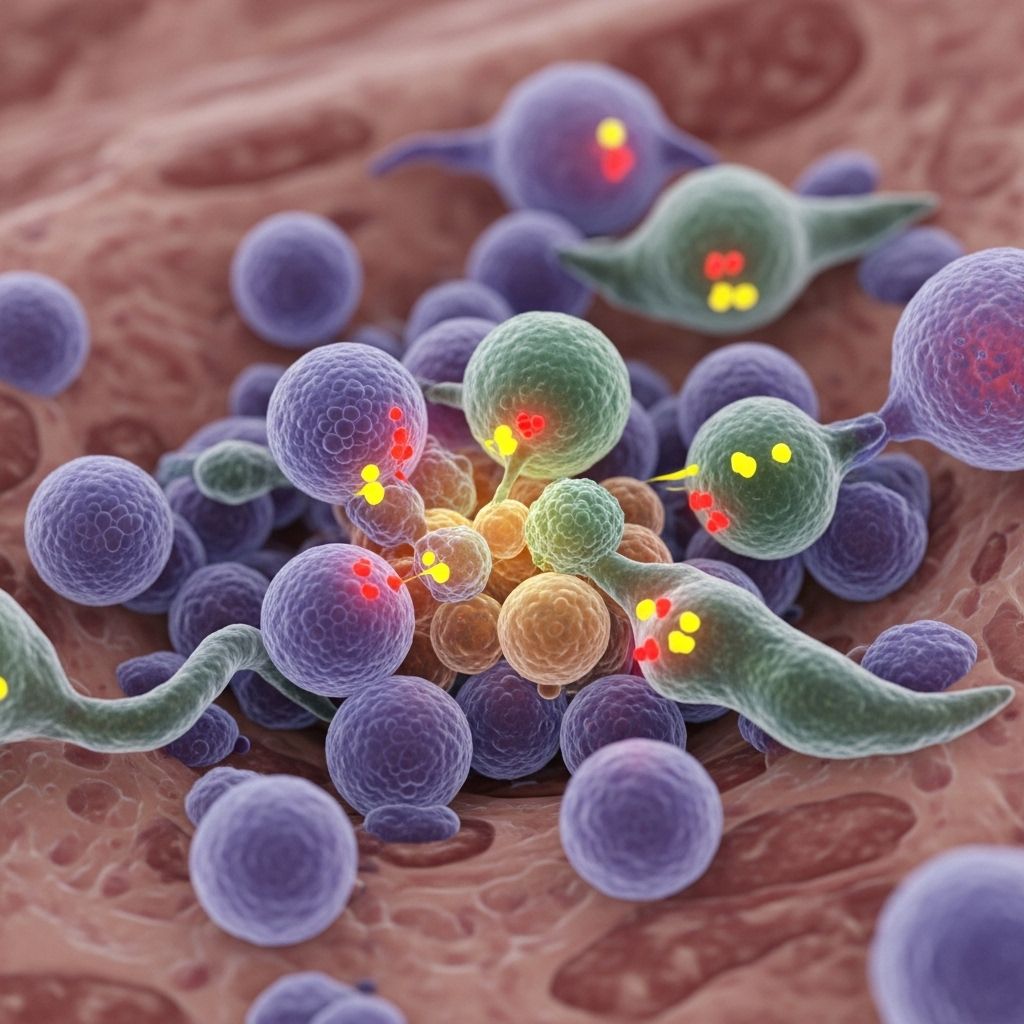
How Does Immunotherapy for SCLC Work?
Immunotherapy involves medications that empower the bodys immune system to identify and destroy cancer cells1. Three principal types are employed in SCLC treatment:
1. Immune Checkpoint Inhibitors
The immune system must balance attacking invaders and sparing healthy cells. It uses molecules called checkpoints to switch immune responses on and off:
- If checkpoints are overactive, they suppress immune responses, letting cancer evade detection.
- Checkpoint inhibitors block these molecules so immune cells (like T cells) can recognize and kill cancer cells more effectively.
2. Tumor Vaccines
Tumor vaccines stimulate the immune system to target antigens (proteins) uniquely produced by tumor cells, guiding the immune system to attack these cells.
3. Monoclonal Antibodies
Monoclonal antibodies are specifically engineered in the laboratory to recognize and bind to antigens on cancer cells, signaling the immune system to target them for destruction.
Types of Immunotherapy Drugs Used for SCLC
Several drugs are currently approved or under investigation for treating SCLC, primarily falling into the immune checkpoint inhibitor and monoclonal antibody categories:
| Drug Name | Type | Target/Mechanism | Status |
|---|---|---|---|
| Atezolizumab | Immune Checkpoint Inhibitor | Anti 6PD-L1 antibody | FDA-approved for extensive-stage SCLC in combination with chemotherapy |
| Durvalumab | Immune Checkpoint Inhibitor | Anti 6PD-L1 antibody | FDA-approved for extensive-stage SCLC in combination therapy |
| Ipilimumab | Immune Checkpoint Inhibitor | Anti 6CTLA-4 antibody | Investigational/limited benefit reported in SCLC trials |
| Nivolumab | Immune Checkpoint Inhibitor | Anti 6PD-1 antibody | Investigational; previously used for relapsed SCLC |
| Monoclonal Antibodies (General) | Monoclonal Antibody | Target tumor-specific antigens | Some in clinical trials |
How Effective Is Immunotherapy for SCLC?
While chemotherapy and radiation remain the primary treatments, the addition of immunotherapy 6specifically in extensive-stage SCLC 6has shown improvement in survival for certain patients2:
- Combined approach: Studies indicate adding immunotherapy to chemotherapy can improve overall survival in extensive-stage SCLC, making this combination the new standard first-line treatment.
- As standalone therapy: Evidence for immunotherapys sole use is limited and generally not recommended as first-line therapy, since SCLC can progress rapidly without immediate chemotherapy intervention1.
- Ongoing research: Dozens of clinical trials continue to evaluate immunotherapy efficacy. Some patients 6especially those whose tumors have specific immune-related features 6benefit more than others3.
Clinical Trial Highlights
- 2013 Phase II: Adding ipilimumab (monoclonal antibody) to chemotherapy for extensive-stage SCLC delivered only minimal extra benefit over placebo1.
- 2016 Phase III: Failed to show an overall survival benefit for ipilimumab plus chemotherapy1.
- 2018 Phase III: Adding atezolizumab to chemotherapy extended survival by about two months compared to placebo1.
- 2019 Phase III: Combining durvalumab and chemotherapy in extensive-stage SCLC resulted in significant improvement in overall survival1.
Who Can Benefit Most from Immunotherapy for SCLC?
Not every patient with SCLC responds equally well to immunotherapy. Research reveals that certain biological factors make some more likely to gain durable benefit, such as:
- High tumor antigen presentation: Tumors with robust expression of antigen presentation machinery are more likely to benefit3.
- Presence of CD8+ T cells: Greater infiltration by these immune cells correlates with better outcomes after immunotherapy3.
Identification of reliable predictive biomarkers remains an ongoing research priority.
Potential Side Effects and Risks of Immunotherapy
As with any treatment, immunotherapy can cause side effects. Most arise due to heightened immune activity, which can also affect healthy tissues. Common potential side effects include:
- Fatigue and weakness
- Skin rashes or itching
- Diarrhea or gastrointestinal upset
- Cough or breathing changes
- Fever
- Hormonal or organ inflammation (rare but serious, can affect thyroid, lungs, liver, etc.)
Promptly reporting side effects to your healthcare provider is crucial, as many can be managed with early intervention.
Combining Immunotherapy with Other Treatments
Clinical experiences show that immunotherapy works best when used together with chemotherapy, especially for extensive-stage SCLC. Trials have explored its combination with:
- Chemotherapy: Most effective in improving survival and now considered standard first-line treatment in this stage2.
- Radiation Therapy: Being investigated in ongoing trials, but standard practice remains limited to chemotherapy plus immunotherapy initially1.
Ongoing Research and Future Directions
SCLC has historically been challenging to treat; however, immunotherapy offers new hope. Current research priorities include:
- Identifying biomarkers for predicting who will respond best
- Combining immunotherapy with targeted agents or radiation
- Developing new drugs that address immune evasion by SCLC cells
- Understanding and overcoming resistance to immunotherapy
Several large-scale clinical trials are underway globally to address these goals.
What to Expect: Starting Immunotherapy for SCLC
If you or a loved one is receiving immunotherapy for SCLC, here are key considerations to discuss with your care provider:
- Expected benefits, risks, and goals of treatment
- How treatment will be delivered (frequency, setting, etc.)
- Possible side effects and when to report new symptoms
- Follow-up schedules, monitoring, and lab tests needed
- Access to supportive care resources
Frequently Asked Questions (FAQs)
What is immunotherapy and how does it differ from chemotherapy?
Immunotherapy uses drugs to enhance or restore the immune systems ability to fight cancer, while chemotherapy uses drugs to directly kill cancer cells. Immunotherapy is often less likely than chemotherapy to cause broad damage to normal cells.
Which immunotherapy drugs are approved for SCLC?
As of 2025, atezolizumab and durvalumab (both immune checkpoint inhibitors targeting PD-L1) are FDA-approved for extensive-stage SCLC in combination with chemotherapy.
Can immunotherapy be used as a first-line treatment for SCLC?
Immunotherapy is not typically used alone as a first-line treatment due to the aggressive nature of SCLC. It is most effective as part of a combination with chemotherapy, especially in extensive-stage disease.
What are the main side effects of immunotherapy for SCLC?
Common side effects include fatigue, rash, diarrhea, fever, and hormonal or organ inflammation. Most are mild, but rare serious reactions can occur and should be reported immediately.
Are there ongoing clinical trials for new immunotherapy drugs in SCLC?
Yes, multiple ongoing trials are assessing new immunotherapy agents, combinations with other therapies, and ways to overcome current drugs’ resistance in SCLC.
Key Takeaways
- Immunotherapy has become a standard addition to chemotherapy for extensive-stage SCLC, improving survival for some patients.
- It works by enabling the immune system to better detect and destroy cancer cells through drugs such as checkpoint inhibitors and monoclonal antibodies.
- Research continues into optimizing its use, selecting the right patients, and improving outcomes.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice. Always consult your healthcare provider about diagnosis, treatment, and follow-up for lung cancer or any health condition.
References
- https://www.healthline.com/health/lung-cancer/immunotherapy-for-small-cell-lung-cancer
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10175664/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10524620/
- https://www.healthline.com/health/lung-cancer/immunotherapy
- https://ascopubs.org/doi/10.1200/EDBK_432520
- https://www.cancer.gov/types/lung/hp/small-cell-lung-treatment-pdq
Read full bio of medha deb












