A Comprehensive Guide to Immunotherapy Options for Kidney Cancer
Explore modern immunotherapy strategies, breakthroughs, and considerations for treating kidney cancer, including recent approvals and best practices.
Immunotherapy Options for Kidney Cancer: An In-Depth Guide
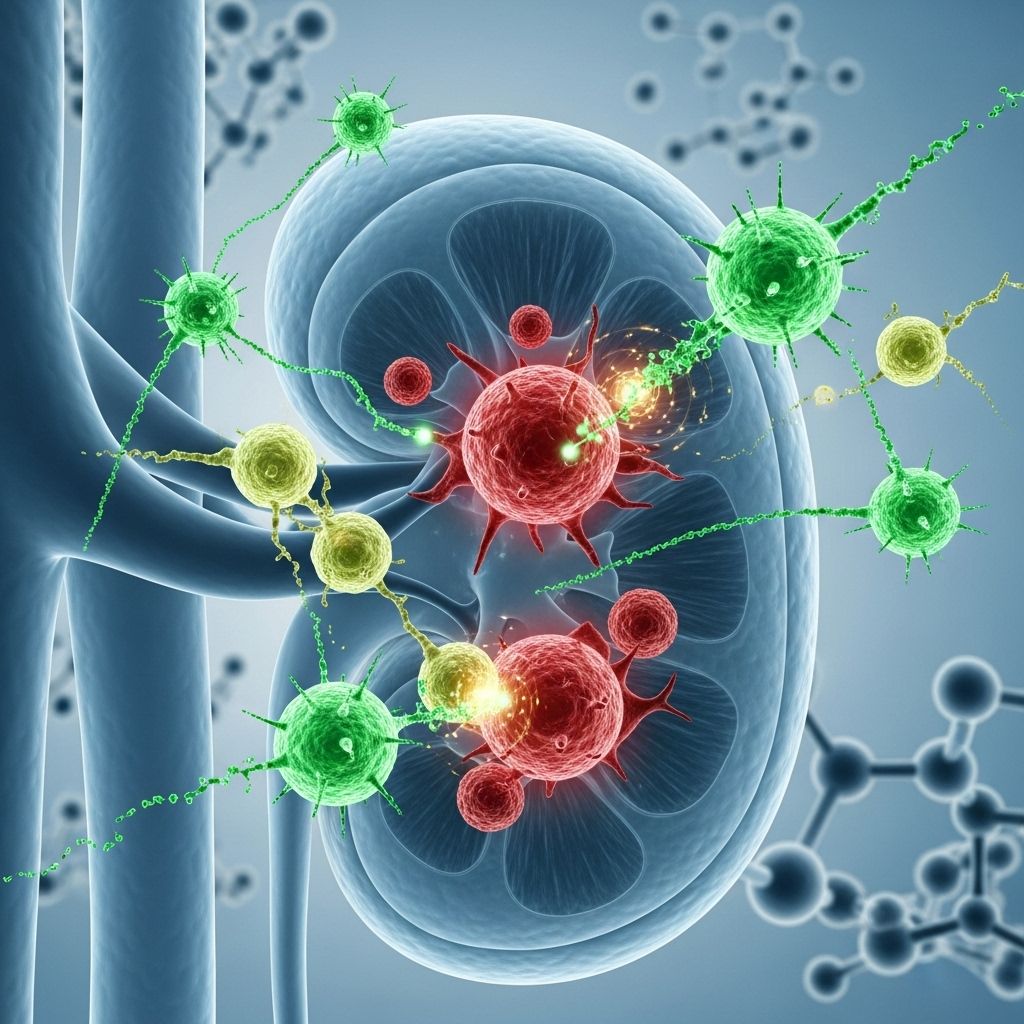
Kidney cancer, especially renal cell carcinoma (RCC), poses unique challenges due to its resistance to traditional therapies like chemotherapy and radiotherapy. In recent years, the landscape of treatment has dramatically evolved with the advent of immunotherapy, a class of treatments designed to harness the power of the body’s own immune system to target and destroy cancer cells.
Understanding Kidney Cancer
Before delving into immunotherapy, it is important to grasp basic facts about kidney cancer:
- The kidneys are vital organs responsible for filtering blood, removing waste, and producing urine.
- Renal cell carcinoma is the most common type of kidney cancer, accounting for around 90% of cases. The most frequent subtype is clear cell carcinoma, but there are other variants including papillary, chromophobe, mucinous tubular and spindle cell (MTSC), Xp11.2 translocation, medullary, and unclassified types.
- Risk factors include smoking, obesity, high blood pressure, chronic renal failure, exposure to certain chemicals (e.g., trichloroethylene), and previous radiation therapy.
- Early-stage kidney cancer often causes no symptoms. Most cases are detected incidentally on scans done for unrelated reasons.
- Symptoms, when present, may include blood in the urine, persistent pain or a mass in the back or abdomen, fatigue, unexplained weight loss, and leg swelling.
Kidney Cancer Statistics
- Approximately 400,000 new renal cancer cases are diagnosed worldwide annually.
- In the United States, more than 80,000 new cases and 15,000 deaths are projected in 2023.
- If diagnosed before it has spread, the 5-year survival can be as high as 93%. When metastatic, this rate drops to around 12%.
Treatment Options for Kidney Cancer
The choice of treatment for kidney cancer is highly individualized, considering the tumor’s location, stage, and the patient’s overall health.
- For early-stage (stages 1–3) cancer, the standard is surgical removal—either a partial or total nephrectomy.
- High-risk features post-surgery may qualify a patient for adjuvant systemic therapy such as immunotherapy.
- For advanced or metastatic disease, treatment typically involves targeted therapies and/or immunotherapy.
- Chemotherapy and traditional radiotherapy are generally less effective due to the intrinsic resistance of kidney tumors.
What Is Immunotherapy?
Immunotherapy is an approach to cancer treatment that stimulates the body’s immune system to recognize and destroy cancer cells more effectively. The rationale comes from observations that kidney cancer can—on rare occasions—regress spontaneously after surgical removal of the primary tumor, suggesting a potential for immune-mediated control.
How Does Immunotherapy Work?
- Cancer can disrupt or suppress immune checkpoints, allowing abnormal cells to evade immune detection and grow unchecked.
- Checkpoint inhibitors are drugs that block proteins (e.g., PD-1, PD-L1, CTLA-4) used by cancer cells to shield themselves from the immune response, thereby reactivating immune cells against the tumor.
- PD-1 inhibitors such as pembrolizumab prevent the interaction of the PD-1 protein with its ligand, restoring immune cell attack capability.
Current FDA-Approved Immunotherapy Options
There are currently seven FDA-approved immunotherapy agents for kidney cancer. These may be administered as single agents or in combination with other immunotherapies or targeted therapies.
- Pembrolizumab (Keytruda):
The first immunotherapy approved for use after surgery (adjuvant therapy) in patients with intermediate-high or high risk of recurrence, shown to reduce the risk of cancer recurrence or death by 32% compared to placebo in the KEYNOTE-564 trial. - Nivolumab (Opdivo):
Approved for treating previously treated advanced RCC, both alone and in combination with ipilimumab. - Ipilimumab (Yervoy):
CTLA-4 inhibitor, often used in combination with nivolumab for increased efficacy. - Avelumab (Bavencio) and Axitinib (Inlyta):
Used in combination for advanced cases. - Atezolizumab (Tecentriq) and Bevacizumab (Avastin):
Also approved for use together in certain metastatic scenarios. - Other checkpoint and targeted therapy combinations may be part of evolving treatment standards.
Older Forms of Immunotherapy: Cytokines
Historically, treatment involved immune-stimulating substances known as cytokines (e.g., interleukin-2, interferon-alpha). These agents are now used in only select cases due to their severe toxicity profiles and moderate efficacy—leading to response rates of 10–20% in advanced cases.
How Immunotherapy Is Given
- Treatments are administered intravenously (IV), typically as infusions every 2–6 weeks, depending on the specific drug protocol.
- The entire course of treatment may last for months or even years, with infusion sessions lasting about 30–60 minutes.
- For adjuvant therapy (after surgery), pembrolizumab is commonly given every 3 weeks for a year.
- The number of treatments is individualized according to the patient’s cancer response and tolerance to side effects.
Who Should Consider Immunotherapy?
- Post-surgery patients at intermediate-high or high risk of recurrence may be offered adjuvant immunotherapy.
- Patients with advanced or metastatic RCC are candidates, potentially as first-line or second-line therapy, or as maintenance to limit progression.
- Cytokine immunotherapies (like IL-2) are reserved for select patients whose cancer is unresponsive to newer agents.
Effectiveness of Immunotherapy
Immunotherapy has revolutionized outcomes for patients with advanced kidney cancer, offering improved survival rates and the possibility of prolonged remission:
- In the pivotal KEYNOTE-564 trial, pembrolizumab reduced the risk of recurrence or death by 32% vs. placebo, with 78.3% of patients disease-free at two years, compared to 67.3% in the placebo group.
- Checkpoint inhibitors may help control cancer growth for many months or even years, especially when used in combination.
- Effectiveness can vary between individuals. Not all patients experience benefit; some may have stable disease, others remission, and a minority rapid response.
Potential Side Effects of Immunotherapy
Immunotherapy is generally well-tolerated, especially compared to older systemic cancer treatments, but it can cause a range of side effects due to activation of the immune system.
- Common side effects may include:
- Fatigue
- Musculoskeletal pain
- Rash
- Itchy skin (pruritus)
- Diarrhea
- Hypothyroidism (decreased thyroid function)
- Around 8% of patients needed steroids for side effect management, and 20% discontinued treatment early because of adverse effects in clinical trials.
- Rare but serious side effects can be life-threatening or irreversible, such as:
- Autoimmune inflammation affecting the liver, lungs, or colon
- Type 1 diabetes mellitus (new onset)
- Adrenal insufficiency
Prompt recognition and treatment of emerging side effects are crucial. Many adverse effects require medical intervention and will not resolve without specific therapy (such as corticosteroids).
Making the Decision: Is Immunotherapy Right for You?
The decision to pursue immunotherapy is highly personal and should be made in close consultation with your oncology team. Key points to consider:
- Potential benefits: Reduced recurrence risk, potential for longer survival, and possibility of remission in advanced cases.
- Risks: Possibility of side effects, including rare but severe immune reactions that can affect quality of life or require treatment cessation.
- Personal factors: Age, overall health, immune status, coexisting conditions, and personal values/goals.
- Convenience and logistics: Treatment requires frequent visits, IV access, and potential hospital monitoring for serious reactions.
Many cancer centers, particularly those with multidisciplinary teams, offer specialized management of immunotherapy and its side effects. Choose a center with expertise in treating kidney cancer whenever possible.
Frequently Asked Questions (FAQs)
What is the main advantage of immunotherapy for kidney cancer?
Immunotherapy can improve survival and reduce recurrence or progression, especially in metastatic or high-risk cases, by harnessing the immune system to fight cancer cells.
Who should not receive immunotherapy?
Patients with a history of severe autoimmune disease, certain organ transplants, or uncontrolled infections may not be good candidates. Consultation with your doctor is necessary to assess individual risks.
What should I expect during treatment?
Treatment typically involves regular IV infusions every 2–6 weeks. You may be monitored for side effects, which can arise weeks or months after treatment initiation. Routine bloodwork and imaging may be required to assess your response and detect complications.
Can immunotherapy be combined with other treatments?
Yes. Combinations of immunotherapy with other immunotherapies (e.g., nivolumab plus ipilimumab) or targeted therapies (e.g., axitinib) are now standard for certain advanced kidney cancer cases.
How long does immunotherapy last?
Duration varies. Adjuvant pembrolizumab is given for one year; advanced/metastatic cases may receive therapy as long as there is disease control and minimal toxicity—sometimes for years.
What should I do if I experience side effects?
Report new or worsening symptoms to your care team immediately. Early management of side effects reduces the risk of irreversible damage or serious complications.
Summary Table: Common Immunotherapies for Kidney Cancer
| Drug | Type | Used For | Key Points |
|---|---|---|---|
| Pembrolizumab (Keytruda) | PD-1 inhibitor | Adjuvant (post-surgery), advanced/metastatic RCC | Reduces recurrence, disease-free survival benefit |
| Nivolumab (Opdivo) | PD-1 inhibitor | Advanced/metastatic RCC, can combine with ipilimumab | First-line and second-line therapy |
| Ipilimumab (Yervoy) | CTLA-4 inhibitor | Combined with nivolumab for advanced/metastatic RCC | Enhanced efficacy with increased side effect risk |
| Avelumab (Bavencio), Atezolizumab (Tecentriq) | Checkpoint inhibitors | Advanced/metastatic (select combinations) | Used with tyrosine kinase inhibitors (e.g., axitinib) |
| Interleukin-2, Interferon-alpha | Cytokine | Selected cases of advanced/unresponsive RCC | High toxicity, less common |
Key Takeaways
- Immunotherapy has transformed the kidney cancer treatment paradigm, especially for advanced or high-risk patients.
- Seven FDA-approved immunotherapies are currently available, often used in combination for the best results.
- Patients must be monitored closely for rare but severe immune side effects.
- Treatment decisions should be made collaboratively with specialist teams, considering individual goals and health status.
Related Reading
- Kidney Cancer Basics: Risk Factors and Early Detection
- Navigating Targeted Therapy Options for Renal Cell Carcinoma
- Understanding the Role of Surgery in Kidney Cancer Treatment
References
- https://utswmed.org/medblog/kidney-cancer-immunotherapy/
- https://www.cancerresearch.org/immunotherapy-by-cancer-type/kidney-cancer
- https://www.cancercouncil.com.au/kidney-cancer/advanced-cancer/immunotherapy/
- https://www.cancer.org/cancer/types/kidney-cancer/treating/immunotherapy.html
- https://www.keytruda.com/kidney-cancer/
- https://www.kidneycancer.org/diagnosis-treatment/treatment-options/
- https://www.aacr.org/patients-caregivers/progress-against-cancer/combining-immunotherapy-and-targeted-therapy-for-kidney-cancer/
- https://www.mayoclinic.org/diseases-conditions/kidney-cancer/diagnosis-treatment/drc-20352669
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9835201/
Read full bio of medha deb












