Immunotherapy for Lung Cancer: How It Works, Success Rates, and What to Expect
Explore immunotherapy options for lung cancer, including how treatments work, possible outcomes, side effects, and the outlook for patients.
Immunotherapy for Lung Cancer: Does It Work?
Immunotherapy has become an increasingly vital approach in treating lung cancer, particularly for those diagnosed with non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC). As new drugs and methods undergo clinical trials, immunotherapy is helping many patients improve survival rates and quality of life.
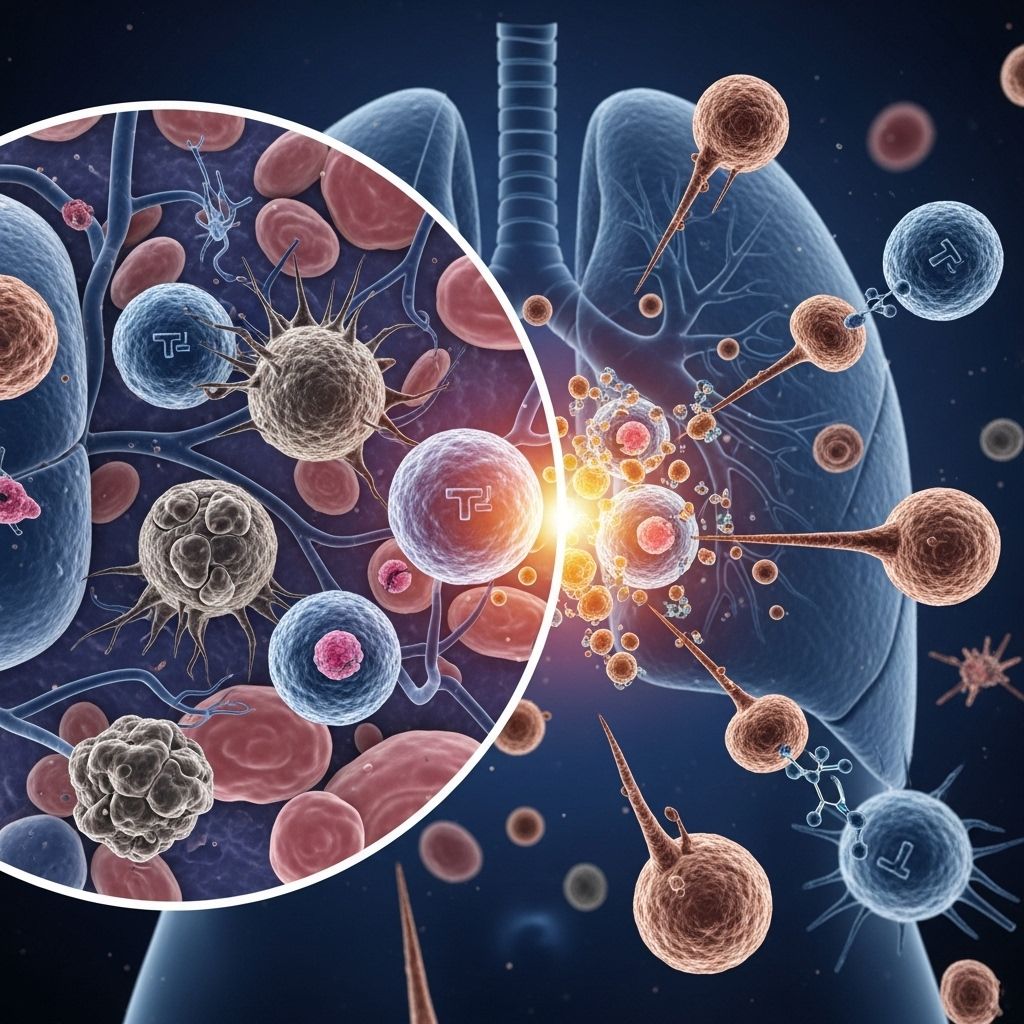
How Immunotherapy Works in Lung Cancer
Immunotherapy uses medications to stimulate or restore the body’s natural defenses against cancer. By engaging the immune system to identify and attack cancer cells, these therapies represent a promising alternative or adjunct to traditional cancer treatments like chemotherapy and radiation.
- The immune system is normally vigilant against abnormal cells, but certain cancers evade detection.
- Immunotherapy drugs help unmask cancer cells or boost immune activity, enabling the body to target and destroy malignant cells.
Types of Immunotherapy for Lung Cancer
There are several types of immunotherapy employed in lung cancer management, with different mechanisms and applications:
- Immune checkpoint inhibitors: These drugs block proteins (checkpoints) that restrain immune responses. Key targets include PD-1, PD-L1, and CTLA-4. By inhibiting these pathways, checkpoint inhibitors allow immune cells to detect and attack cancer cells more effectively.
- Tumor vaccines: Different from traditional vaccines, tumor vaccines are designed to bind to specific antigens present on cancer cells and trigger an immune response against them.
- Monoclonal antibodies: Laboratory-engineered antibodies that mimic natural immune responses and bind to cancer antigens, flagging abnormal cells for destruction by the immune system.
Immune Checkpoint Inhibitors Explained
Cancer immune surveillance involves the immune system searching for antigens on cancer cells. But tumors may go undetected if immune checkpoints are too active, suppressing the response. Checkpoint inhibitors remove these restraints — letting T cells and natural killer cells fight more aggressively against tumors.
Side Effects and Risks of Immunotherapy
Although immunotherapy is generally less toxic than chemotherapy, it can present unique side effects due to immune system activation:
- Fatigue
- Skin rashes or itching
- Diarrhea
- Lung inflammation (pneumonitis)
- Endocrine changes (thyroid dysfunction, etc.)
- Joint pain
Most side effects are manageable, but severe immune reactions can occur, affecting organs such as the liver, lungs, or heart. For this reason, patients on immunotherapy require regular monitoring and prompt attention to new symptoms.
Success Rates of Immunotherapy for Lung Cancer
Immunotherapy has been transformative for several forms of lung cancer, but results vary:
- NSCLC: Immune checkpoint inhibitors are now first-line treatments for many patients. Survival outcomes have improved, especially in metastatic disease and after chemoradiation in locally advanced cancer.
- SCLC: Chemotherapy and radiation remain mainstays, but adding certain immunotherapy agents to chemo has extended survival for some — often by only a few months.
Ongoing clinical trials continue to uncover new uses for immunotherapy, with some drugs already showing increased survival times. However, predicting who will respond remains challenging, and resistance to therapy can develop.
Notable Clinical Trial Outcomes
| Year | Drug & Combination | Population | Result |
|---|---|---|---|
| 2013 | Ipilimumab + Chemo vs Placebo + Chemo | Extensive-stage SCLC | Minimal benefit with ipilimumab |
| 2016 | Ipilimumab + Chemo vs Placebo + Chemo | Extensive-stage SCLC | No improved survival |
| 2018 | Atezolizumab + Chemo vs Placebo + Chemo | Extensive-stage SCLC | Improved survival by 2 months |
| 2019 | Durvalumab + Chemo | Extensive-stage SCLC | Significant improvement in overall survival |
Who is a Candidate for Immunotherapy?
The suitability of immunotherapy depends on cancer type, stage, previous treatments, and specific biomarkers:
- Some forms of NSCLC respond especially well to immunotherapy, particularly when high levels of PD-L1 are present on tumor cells.
- Stage and spread of the cancer are considered — metastatic disease is most likely to be treated with immunotherapy.
- Patients with autoimmune diseases or organ transplants may not be candidates due to risk of complications.
- Additional tests can help determine if immunotherapy is likely to benefit an individual patient.
Clinical Trials and Research
As researchers refine these therapies, dozens of clinical trials continue investigating possible benefits:
- Trials compare immunotherapy drugs alone, in combination with chemotherapy, or in sequence with radiation.
- New agents and targets — including engineered T cells or vaccines — are being developed for both NSCLC and SCLC.
- Biomarker discovery is essential to identify responders and avoid unnecessary treatment.
Outlook and Future Directions
Immunotherapy is not curative for most, but it does offer prolonged survival and improved quality of life for certain types of lung cancer. Ongoing research aims to make these gains available to more patients through:
- Refined patient selection via genetic or biomarker testing
- Novel drug targets and combination therapies
- Cell-based immunotherapies, such as CAR-T cell engineering
- Strategies to overcome resistance
Despite tremendous advances, scientists emphasize the need for personalized approaches, further clinical testing, and vigilant symptom management during immunotherapy treatment.
Frequently Asked Questions (FAQs)
Q: Is immunotherapy a cure for lung cancer?
A: Immunotherapy is not a cure for most lung cancers but can extend life and improve symptoms for many patients. For some, it leads to long-term remission.
Q: How long does immunotherapy treatment last?
A: Treatment duration varies depending on response, side effects, and cancer type. Some may receive periodic infusions for many months to years.
Q: What are the risks of immunotherapy?
A: Common risks include fatigue, rash, diarrhea, and organ inflammation. Severe immune reactions require medical attention, but most side effects are manageable with therapy adjustments.
Q: Who should avoid immunotherapy?
A: Patients with serious autoimmune diseases or prior organ transplants may not be candidates due to risk of immune-related complications. Always consult with your oncology team.
Q: What is the difference between immunotherapy and chemotherapy?
A: Chemotherapy targets rapidly dividing cells non-specifically, causing widespread side effects. Immunotherapy harnesses the body’s immune system to target cancer cells more selectively, often with fewer systemic side effects.
Key Takeaways
- Immunotherapy is a rapidly evolving treatment that holds promise for lung cancer patients, especially those with advanced disease.
- Drug types include checkpoint inhibitors, monoclonal antibodies, and cancer vaccines; each works differently to activate or support immune defense against tumors.
- While not curative for most, immunotherapy can extend survival and improve quality of life compared to traditional options.
- Success rates depend on cancer subtype, stage, individual biomarkers, and treatment combination.
- Clinical trials are crucial for expanding immune-based therapies and refining patient selection criteria.
References
- https://www.healthline.com/health/lung-cancer/immunotherapy-for-small-cell-lung-cancer
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8864096/
- https://www.healthline.com/health/lung-cancer/immunotherapy
- https://www.medicalnewstoday.com/articles/323701
- https://www.lung.org/lung-health-diseases/lung-disease-lookup/lung-cancer/treatment/types-of-treatment/immunotherapy
- https://www.cancer.gov/types/lung/hp/non-small-cell-lung-treatment-pdq
- https://www.chp.gov.hk/en/static/80049.html
- https://ascopubs.org/doi/10.1200/JCO.21.01497
- https://www.lungcancercenter.com/lung-cancer/stages/stage-1/
Read full bio of medha deb












