IgA Nephropathy: Risk Factors, Causes, and Complications Explained
Learn what puts you at risk for IgA nephropathy, how it develops, and the critical reasons early detection is essential.
IgA Nephropathy: Understanding Risk Factors, Causes, and Complications
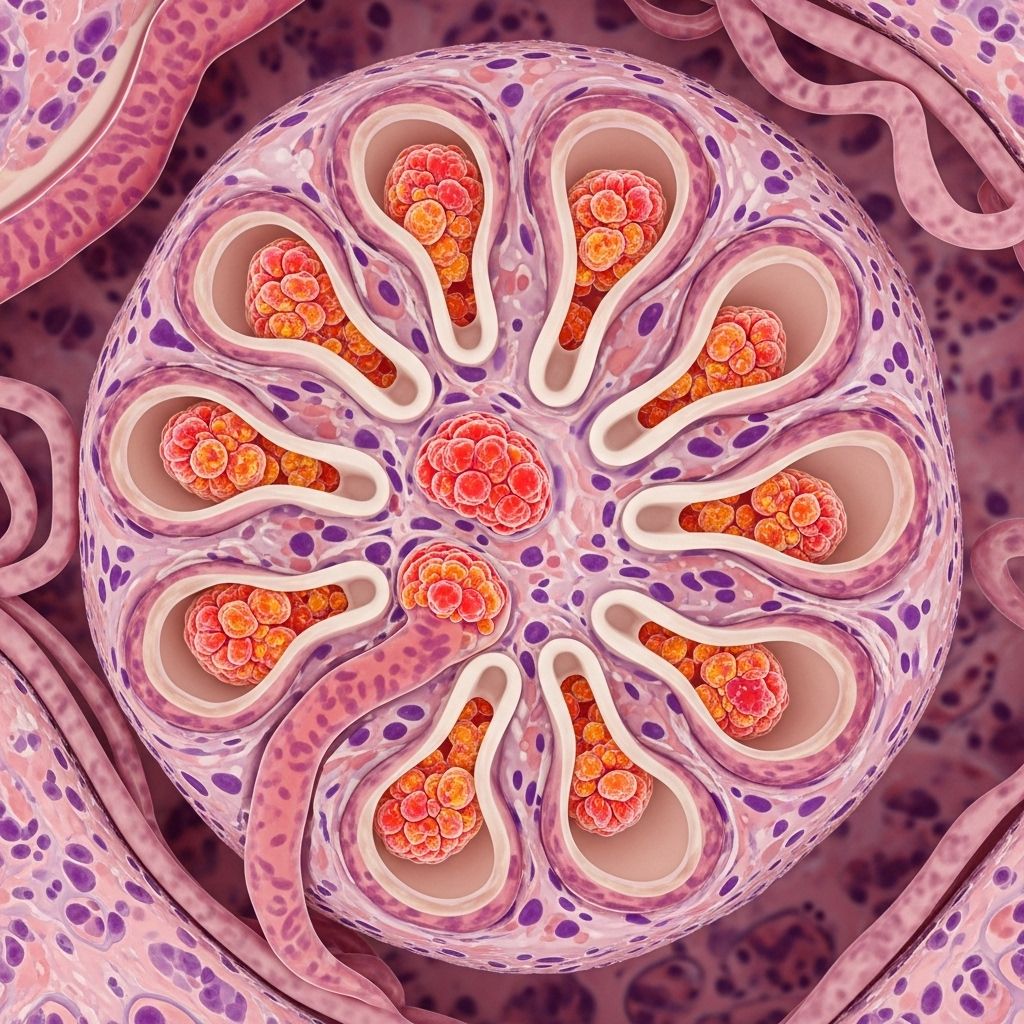
IgA nephropathy, also known as Berger’s disease, is a chronic autoimmune condition affecting the kidneys. It develops when immunoglobulin A (IgA), a type of antibody, abnormally builds up in the small blood vessels within the kidneys, causing inflammation and damage. Over time, this can lead to chronic kidney disease, kidney failure, and additional complications impacting overall health.
This article explores the key risk factors, suspected causes, and critical complications associated with IgA nephropathy, while offering guidance on who is most vulnerable and what actions can be taken to manage the condition.
What is IgA Nephropathy?
IgA nephropathy is a type of autoimmune kidney disease where IgA antibodies form clusters in the kidneys, triggering inflammation and disruption of their filtration capacity. The disease often progresses slowly, sometimes over decades, and is a major contributor to both chronic kidney disease and kidney failure.
- Autoimmune origin: The body’s immune system targets its own tissues, causing renal inflammation.
- Alternate name: Also commonly referred to as Berger’s disease.
- Presentation: IgA deposits can remain asymptomatic initially; symptoms may take years to manifest.
How Common Is IgA Nephropathy?
IgA nephropathy is one of the most common causes of kidney disease worldwide. In the United States, it accounts for about 1 in 10 kidney biopsies.
- Common in East Asian, White European, and Pacific Islander ancestry.
- More prevalent in individuals assigned male at birth.
- Most cases diagnosed between the ages of 10 and 40.
Key Facts Table
| Aspect | Details |
|---|---|
| Alternate Name | Berger’s Disease |
| Occurrence | About 1 in 10 kidney biopsies in U.S. show IgA nephropathy |
| Common Age Range | 10 to 40 years |
| Most Affected Groups | East Asian & White European ancestry; Males |
Risk Factors for IgA Nephropathy
While anyone can develop IgA nephropathy, certain factors markedly increase susceptibility. Recognizing these risk factors aids in early detection and proactive management:
- Genetic Factors: Family history of IgA nephropathy or IgA vasculitis.
- Age: Primarily affects people aged 10–40.
- Sex: More frequently diagnosed in males.
- Ethnicity: Increased prevalence in Asians, White Europeans, and Pacific Islanders.
- Underlying Health Conditions:
- Celiac disease
- Inflammatory bowel disease
- Liver diseases (hepatitis, cirrhosis)
- HIV infection
- Dermatitis herpetiformis
- Henoch-Schönlein purpura
- Recent Infections: Particularly respiratory infections such as pharyngitis, tonsillitis, or colds
Causes of IgA Nephropathy
The exact cause is not fully understood, and ongoing research continues to uncover contributing factors. Current evidence suggests that both genetic and environmental influences play significant roles.
- IgA molecules abnormally bind to each other, forming long chains in the bloodstream.
- These chains are deposited in the kidney’s glomeruli (filtration units).
- The deposits trigger chronic inflammation, leading to impaired kidney function.
- Some people experience first symptoms after a viral or bacterial infection.
Genetic Contributions
- Familial clustering and genes linked to immune system function suggest a strong genetic component.
- Research is ongoing into specific gene variants affecting IgA structure and immune regulation.
Environmental and Health Triggers
- Infections, especially viral illnesses of the upper respiratory tract, can precede disease onset.
- Chronic liver conditions and autoimmune disorders can increase risk.
- Diet and gut health may play indirect roles in immune activation and response.
Symptoms of IgA Nephropathy
IgA nephropathy is sometimes called a “silent” disease because initial symptoms can be subtle or absent, making early detection challenging.
- Microscopic hematuria (blood in urine not visible to the naked eye)
- Gross hematuria (tea-colored or cola-colored urine)
- Proteinuria (foamy urine due to protein)
- Swelling (edema) in ankles, feet, legs, or other areas
- High blood pressure
- Pain below the ribs or lower back
- Fatigue and general weakness
Routine urine tests sometimes reveal kidney involvement before any outward symptoms arise. If untreated, symptoms can worsen and lead to serious complications.
Complications of IgA Nephropathy
If IgA nephropathy is not managed effectively, progressive kidney damage can cause a range of health complications:
High Blood Pressure (Hypertension)
Damaged kidneys struggle to regulate sodium, water, and hormones involved in blood pressure control. This results in increased blood pressure, which further accelerates kidney injury.
Chronic Kidney Disease (CKD)
Long-term inflammation and scarring can lead to gradual loss of kidney function. People with CKD face a higher risk of heart disease, metabolic complications, and stroke.
Nephrotic Syndrome
This cluster of symptoms results from severe kidney damage and includes:
- High protein levels in urine
- Low protein levels in blood
- High cholesterol and lipid levels
- Generalized swelling
Kidney Failure
When kidney function drops too low to support the body’s needs, kidney failure (end-stage renal disease) occurs. Dialysis or transplantation may become necessary. Approximately 1 in 5 people with IgA nephropathy will experience kidney failure within 10 years of diagnosis.
Cardiovascular Disease
The kidney can no longer filter excess proteins, sodium, and toxins, raising the risk for heart attack, stroke, and heart failure.
Diagnosis of IgA Nephropathy
Diagnosing IgA nephropathy often begins with urinalysis (protein and blood detection), blood tests (to gauge kidney function), and confirmation through a kidney biopsy, where tissue samples are examined for IgA deposits and inflammation.
Managing IgA Nephropathy and Its Complications
Although there is currently no cure for IgA nephropathy, treatments are available that can control symptoms, slow disease progression, and help prevent complications.
Medications
- ACE inhibitors or ARBs: Reduce protein in urine and control blood pressure, slowing kidney deterioration.
- Endothelin receptor antagonists (ERAs): Relax kidney blood vessels and reduce proteinuria.
- SGLT2 inhibitors: Lower urine protein levels, also help stabilize blood sugar in diabetics.
- Corticosteroids: Calm immune system activity, decreasing harmful IgA production (typically used short-term to avoid side effects).
Lifestyle and Self-Care
- Maintain a blood pressure-friendly diet (low salt, balanced nutrition).
- Achieve and sustain a healthy body weight.
- Exercise regularly as tolerated.
- Manage or prevent diabetes and cardiovascular risk factors.
- Work closely with a nephrologist for ongoing care and monitoring.
Monitoring and Specialist Care
A kidney specialist (nephrologist) will typically oversee management, monitor kidney function, and suggest treatment adjustments as needed.
Frequently Asked Questions (FAQs)
Q: Is IgA nephropathy hereditary?
A: Genetics play a role in susceptibility. People with a family history of IgA nephropathy or IgA vasculitis are at higher risk, but environmental factors are also involved. Several genes related to immune regulation have been implicated.
Q: Can people with IgA nephropathy live a normal life?
A: Many people with IgA nephropathy live full lives, especially with early diagnosis and good symptom management. However, it’s important to monitor kidney function regularly and follow a customized treatment plan.
Q: Are certain populations more affected than others?
A: Yes, IgA nephropathy is more common in males, individuals aged 10 to 40, and those of East Asian and White European ancestry.
Q: What symptoms require urgent medical attention?
A: Sudden swelling, tea-colored or foamy urine, high blood pressure that does not respond to medications, and severe fatigue should be promptly evaluated by a doctor.
Q: How is IgA nephropathy diagnosed?
A: Diagnosis typically involves urinalysis (looking for blood or protein), blood tests for kidney function, and confirmation through a kidney biopsy to detect IgA deposits.
Conclusion
IgA nephropathy is a leading cause of chronic kidney disease and kidney failure, often arising from a complex interplay of genetics, underlying conditions, and environmental factors. Understanding risk factors and disease mechanisms is crucial for early diagnosis, proactive management, and reducing the burden of complications. Regular monitoring, tailored medication, and lifestyle measures are vital to slowing progression and maintaining overall health. If you suspect any symptoms or have relevant risk factors, consult your healthcare provider to discuss appropriate screening and preventive strategies.
References
- https://www.medicalnewstoday.com/articles/what-is-iga-nephropathy
- https://www.niddk.nih.gov/health-information/kidney-disease/iga-nephropathy
- https://www.healthline.com/health/iga-nephropathy-bergers
- https://www.healthline.com/health/kidney-health/igan-awareness-day
- https://www.medicalnewstoday.com/program/a-deeper-understanding-of-igan
- https://igan.org/nutrition/
- https://www.healthline.com/health/video/foods-to-avoid-with-kidney-disease
- https://www.youtube.com/watch?v=YNmJiiPBTss
Read full bio of Sneha Tete












