IgA Nephropathy: Risk Factors and Causes Explained
Gain a detailed understanding of IgA nephropathy, including the causes, risk factors, and complications that influence this autoimmune kidney disease.
IgA Nephropathy: Risk Factors and Causes
Immunoglobulin A nephropathy, also known as IgA nephropathy or Berger’s disease, is a chronic autoimmune kidney disease characterized by the deposition of the IgA antibody in the kidneys. This accumulation sets off a cascade of events that can damage the kidneys and hamper their essential functions. Understanding the risk factors and potential causes of IgA nephropathy is crucial for early detection, disease management, and minimizing long-term complications.
What is IgA Nephropathy?
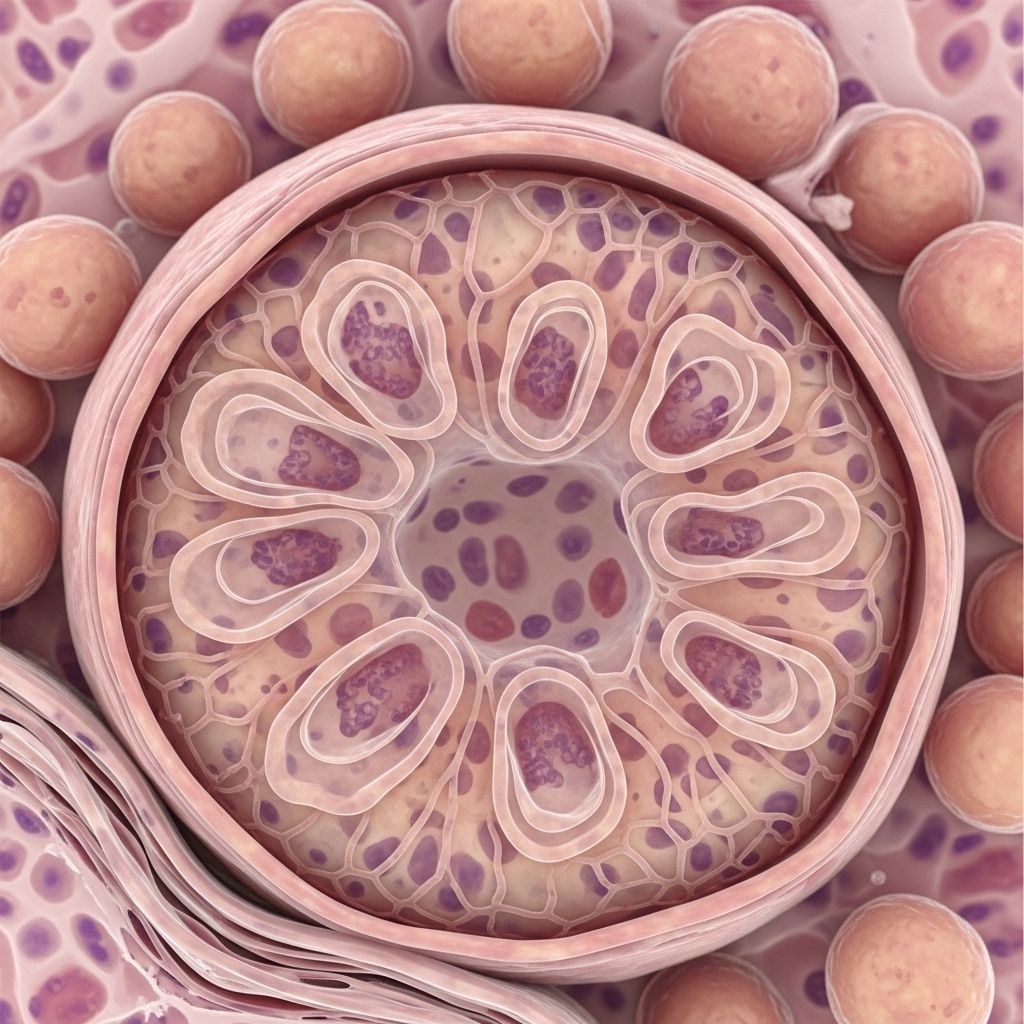
IgA nephropathy is a type of autoimmune kidney disorder in which the antibody immunoglobulin A (IgA) forms clumps and becomes lodged in the glomeruli – the small filtering units of the kidneys. This triggers local inflammation and, over time, may impair the kidneys’ ability to filter waste and excess fluids from the blood. The condition can range from mild forms with little impact to severe disease progressing to chronic kidney disease or even kidney failure.
How Does IgA Nephropathy Develop?
The pathophysiology of IgA nephropathy centers on immune system dysfunction. Immunoglobulin A, a major antibody in the immune response, should help defend against infections. In IgA nephropathy, however, the body produces abnormal IgA molecules that tend to bind together and form complexes. These clusters become trapped in the glomeruli, causing inflammation and possible scarring (fibrosis) of kidney tissue over time. The exact mechanisms by which this abnormal immune activity begins remain unclear, but both genetic susceptibility and environmental triggers are believed to play key roles.
Who is at Risk for IgA Nephropathy?
While IgA nephropathy can develop in anyone, certain groups and conditions are associated with a significantly higher risk. The following table summarizes the known risk factors:
| Risk Factor | Details/Description |
|---|---|
| Age | Most common between ages 10 and 40. |
| Sex | More frequent in males than females. |
| Ethnicity | Higher incidence in people of East Asian, White European, or Pacific Island descent. |
| Family History | Having a family member with IgA nephropathy or IgA vasculitis increases risk. |
| Certain Health Conditions | Includes celiac disease, inflammatory bowel disease, cirrhosis, hepatitis, HIV, and dermatitis herpetiformis. |
| Infections | Respiratory or gastrointestinal infections can trigger symptom onset in some individuals. |
Demographic Risk Factors
- Age: Most common between ages 10 and 40, but possible at any age.
- Sex: Occurs more frequently in people assigned male at birth, though reasons remain unclear.
- Ethnicity: Increased frequency in people of East Asian, White European, or Pacific Island ancestry.
Genetic Factors
- Family history: Having close relatives with IgA nephropathy or IgA vasculitis raises your risk, suggesting a genetic component.
Associated Health Conditions
- Liver diseases, such as cirrhosis and hepatitis B or C, are linked to higher risk of IgA nephropathy.
- Celiac disease and inflammatory bowel diseases (such as Crohn’s disease and ulcerative colitis) can be associated with the onset of IgA nephropathy.
- HIV infection and certain skin disorders like dermatitis herpetiformis are also associated with increased risk.
Triggering Infections
- Respiratory infections (colds, sore throats)
- Gastrointestinal infections
- Viral infections such as hepatitis and HIV
In many cases, flares or the initial onset of IgA nephropathy symptoms occur soon after an upper respiratory or gastrointestinal infection, indicating that infection may act as a trigger in genetically susceptible individuals.
Environmental and Lifestyle Factors
- Infections: Certain infections, especially of the upper respiratory and digestive tracts, may trigger flares or lead to the disease’s initial presentation.
- Unlike some chronic illnesses, no strong connection exists between diet, smoking, or environmental toxins and the risk of IgA nephropathy. However, maintaining overall kidney health through a balanced diet and healthy lifestyle is always recommended.
What Causes IgA Nephropathy?
Despite decades of research, the precise cause of abnormal IgA production and accumulation in the kidneys remains obscure. The most widely accepted explanations involve a combination of genetic predisposition and environmental influences.
The main steps in disease development typically include:
- Production of abnormal IgA: For unclear reasons, the immune system produces faulty IgA antibodies.
- Formation of IgA complexes: These abnormal antibodies cluster together, forming immune complexes that are not cleared from the bloodstream.
- Deposition in kidney glomeruli: These immune complexes accumulate in the filtering units of the kidneys.
- Inflammation and damage: The deposits provoke local inflammation, leading to glomerular injury and impaired kidney function.
Currently Proposed Contributing Factors
- Genetic mutations or susceptibility: Certain genes may predispose individuals to produce abnormal IgA.
- Immune regulation defects: Improper immune signaling or regulation could cause excessive or aberrant IgA responses.
- External triggers: Infections (bacterial or viral) are frequent triggers, potentially provoking abnormal immune activity in susceptible individuals.
- Other autoimmune conditions: Those with diseases such as celiac disease are at increased risk, making a systemic immune dysfunction more likely.
Early Signs and Complications of IgA Nephropathy
IgA nephropathy often progresses silently, with no symptoms in its early stages. When symptoms do occur, they may include blood in the urine (hematuria), foamy urine due to protein loss (proteinuria), and swelling (edema). If left unmanaged, the ongoing kidney damage can lead to more serious health consequences.
Common Signs and Symptoms
- Blood in urine (hematuria): Can be visible (pink, cola-colored urine) or detected via microscopic examination.
- Proteinuria: Foamy urine indicates presence of protein, reflecting kidney filter damage.
- Edema: Swelling in the legs, ankles, or around the eyes.
- High blood pressure: Damaged kidneys may no longer regulate blood pressure properly.
- Fatigue and weakness from chronic kidney dysfunction.
Major Complications
- High blood pressure (hypertension): Both a cause and consequence of kidney disease, hypertension can accelerate damage.
- Chronic kidney disease (CKD): IgA nephropathy is a leading cause; CKD involves gradual, progressive loss of kidney function and may result in kidney failure.
- Nephrotic syndrome: A cluster of symptoms including high protein in urine, low blood protein, and elevated cholesterol – all pointing to severe kidney damage.
- Cardiovascular disease: Increased risk due to protein loss and high blood pressure.
- Kidney failure (end-stage renal disease): Roughly 1 in 5 people diagnosed with IgA nephropathy progress to kidney failure within 10 years.
Can IgA Nephropathy Be Prevented?
There is currently no known method to prevent IgA nephropathy outright, as the underlying mechanisms largely involve uncontrollable genetic and immune system factors. However, strategies that may help reduce risk or delay disease progression include:
- Managing associated health conditions: Good control of liver disease, celiac disease, and inflammatory bowel conditions may help reduce risk in susceptible individuals.
- Prompt treatment of infections: Address respiratory or gastrointestinal infections quickly to avoid triggering disease flares.
- Regular health checkups: Monitoring urine for blood or protein can help detect the disease early, even before symptoms develop.
- Adhering to a healthy lifestyle: Healthy diet, exercise, and blood pressure control support kidney health in general.
Treatment Approaches for Those at Risk
Treating IgA nephropathy centers around slowing disease progression and preventing complications. While no cure exists, effective management can often maintain kidney function and improve quality of life. Treatment commonly includes:
- Medications
- ACE inhibitors or ARBs: First-line therapies for lowering proteinuria and blood pressure.
- Endothelin receptor antagonists (ERAs): Newer drugs to help limit kidney inflammation and protein loss.
- SGLT2 inhibitors: Used for reducing proteinuria, managing blood sugar, especially helpful for patients with diabetes.
- Corticosteroids: Used to suppress the immune system when indicated, typically in short courses.
- Lifestyle modifications: Including sodium restriction, healthy weight, smoking cessation, and regular physical activity.
- Monitoring: Routine assessments for kidney function, blood pressure, and protein in the urine help guide therapy and detect changes early.
For individuals with advanced disease or kidney failure, further interventions such as dialysis or kidney transplantation may be necessary.
Key Takeaways
- IgA nephropathy is an autoimmune disorder primarily affecting the kidneys through the build-up of IgA antibodies.
- Genetic, demographic, and certain health conditions significantly increase risk.
- Early signs are subtle or absent; complications can be severe if unrecognized.
- Treatment focuses on managing symptoms and slowing progression rather than cure.
Frequently Asked Questions (FAQs)
What is the prognosis for people diagnosed with IgA nephropathy?
Prognosis varies widely. While some people experience mild disease with few complications, about 20% may develop kidney failure within a decade of diagnosis. Close monitoring and management can help improve outcomes.
Is IgA nephropathy contagious?
No, IgA nephropathy is not a contagious condition. It results from immune and genetic factors rather than infection transmission.
Can lifestyle changes help prevent IgA nephropathy?
No lifestyle changes can directly prevent the development of IgA nephropathy, but a healthy lifestyle, prompt infection treatment, and managing related conditions may help lower risk or slow disease progression.
Are there specific foods to avoid or follow with IgA nephropathy?
There is no specific ‘IgA nephropathy diet,’ but general kidney-friendly diets emphasizing low sodium, balanced protein, and healthy fats are recommended. People with associated celiac disease should strictly avoid gluten.
How common is IgA nephropathy?
It is one of the most common causes of chronic kidney disease worldwide, affecting about 1 in 10 people who undergo a kidney biopsy in the United States. It is more common in men, people aged 10–40, and those with East Asian or White European ancestry.
References
- https://www.medicalnewstoday.com/articles/what-is-iga-nephropathy
- https://www.niddk.nih.gov/health-information/kidney-disease/iga-nephropathy
- https://www.healthline.com/health/iga-nephropathy-bergers
- https://www.healthline.com/health/kidney-health/igan-awareness-day
- https://www.medicalnewstoday.com/program/a-deeper-understanding-of-igan
- https://igan.org/nutrition/
- https://www.healthline.com/health/video/foods-to-avoid-with-kidney-disease
- https://igan.org/diet-nutrition/managing-iga-nephropathy-with-an-anti-inflammatory-diet/
Read full bio of Sneha Tete












