Understanding IgA Nephropathy and its Progression to End-Stage Renal Disease
Explore the risks, symptoms, and management of IgA nephropathy and how it leads to end-stage renal disease.
What to Know About IgA Nephropathy and End-Stage Renal Disease
IgA nephropathy is a rare chronic autoimmune disorder that targets the kidneys, often resulting in progressive kidney damage and sometimes kidney failure. This article details how IgA nephropathy develops, its relationship with end-stage renal disease (ESRD), associated complications, risk factors, and available treatments.
What is IgA Nephropathy?
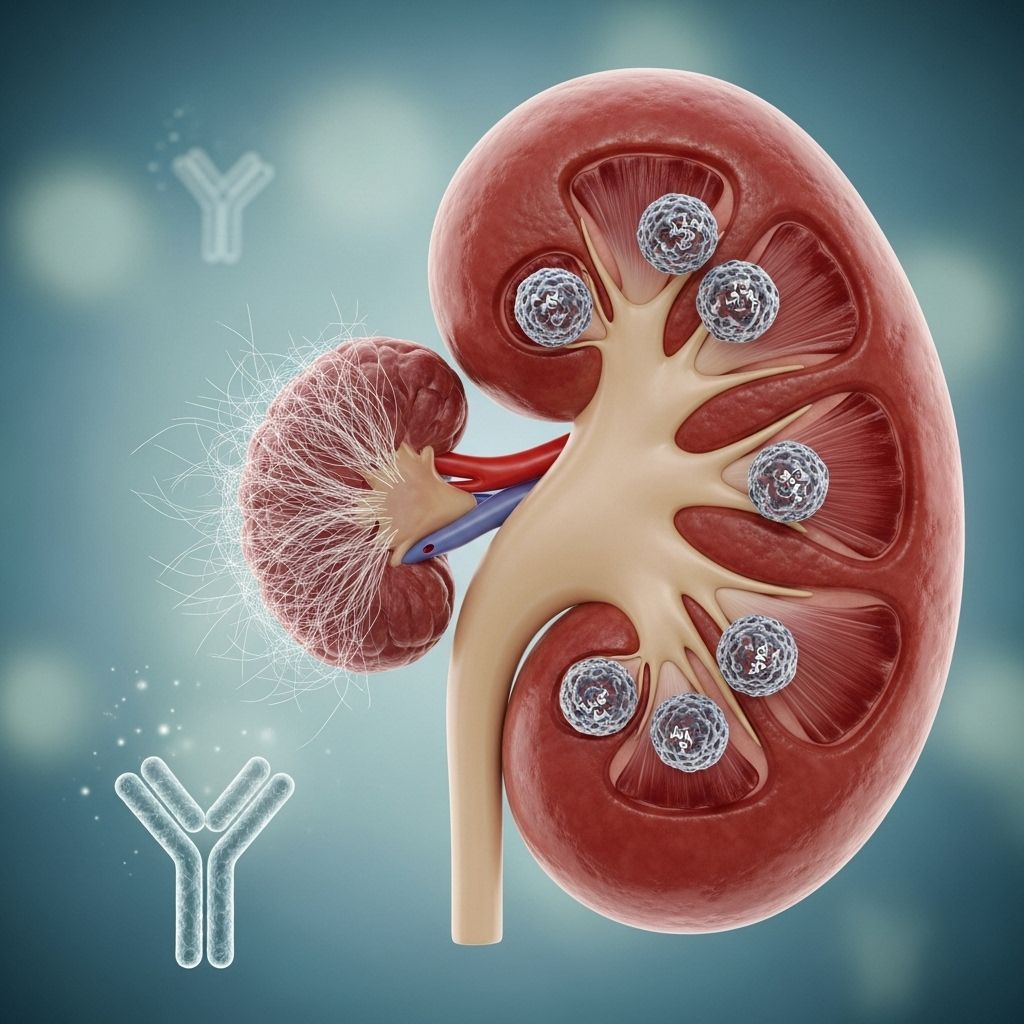
IgA nephropathy, also known as Berger’s disease, is an autoimmune condition in which the body’s immune system mistakenly targets healthy kidney tissue. In this disorder, large amounts of immunoglobulin A (IgA) antibodies accumulate within the glomeruli—tiny filters in the kidneys responsible for cleaning the blood. This buildup leads to inflammation, ultimately damaging the kidney’s filtering capacity over time.
- Glomeruli damage causes blood and protein to leak into the urine.
- The disease often presents as visible blood (hematuria) or excess protein (proteinuria) in the urine.
- It is the third most common cause of kidney disease after high blood pressure and diabetes.
- IgA nephropathy can develop slowly or, in some cases, progress more rapidly.
Symptoms and Early Signs
IgA nephropathy can be clinically silent for years, or its progression can be rapid. Common signs and symptoms include:
- Blood in the urine (urine may appear cola- or tea-colored, especially after respiratory infections)
- Foamy urine, indicating proteinuria
- Swelling in the hands, feet, or around the eyes
- High blood pressure (hypertension)
- Fatigue and general weakness
- Pain in the lower back or sides
- Invisible blood or protein in the urine, sometimes detected only during a routine urine test
How is IgA Nephropathy Detected?
A diagnosis often arises from a routine urine test after observing blood or protein. A definitive diagnosis may require a kidney biopsy to examine glomerular changes and the extent of damage.
Progression: IgA Nephropathy and End-Stage Renal Disease (ESRD)
Over time, progressive damage from IgA accumulation can compromise the kidneys’ ability to filter blood. When untreated or poorly managed, this process may lead to end-stage renal disease (ESRD), where the kidneys can no longer support essential functions without medical intervention.
- ESRD requires lifelong dialysis or a kidney transplant for survival.
- Approximately 1 in 5 people with IgA nephropathy develop kidney failure within 10 years of diagnosis.
- Early and effective treatment can slow progression and delay or prevent ESRD.
How IgA Nephropathy Causes Kidney Failure
IgA deposits inflame and scar the glomeruli and surrounding kidney tissue. As scarring worsens, filtering efficiency drops. Eventually, waste builds up in the bloodstream, leading to severe complications.
Who is at Risk?
While anyone can develop IgA nephropathy, several demographic and medical factors increase susceptibility:
- Biological male
- Family history of IgA nephropathy or IgA vasculitis
- Ages 10–40 (most diagnoses occur in younger adults)
- Pacific Islander, White European, or Asian descent
- Associated conditions:
- Inflammatory bowel disease (IBD)
- Chronic infections (e.g., hepatitis, HIV)
- Celiac disease
- Cirrhosis (liver failure)
Complications of IgA Nephropathy
Complications result from both kidney dysfunction and the underlying autoimmune activity. Major complications include:
- High blood pressure: Damaged kidneys increase blood pressure, worsening kidney damage and raising cardiovascular risks.
- High cholesterol: Linked to kidney dysfunction, increases risk of heart attack and stroke.
- Acute kidney failure: Sudden, severe loss of kidney function—may require urgent dialysis.
- Nephrotic syndrome: Cluster of symptoms including extreme proteinuria, low blood protein, elevated cholesterol, and swelling (edema) around the eyes, abdomen, feet.
Symptoms and Complications of End-Stage Renal Disease
Progression to ESRD brings a host of severe and systemic symptoms due to accumulation of waste in the blood. Common issues include:
- Changes in urination (frequency, color, or cessation)
- Nausea and vomiting
- Loss of appetite
- Persistent fatigue
- Generalized swelling (edema)
- Anemia (lack of red blood cells)
- Increased bleeding and easy bruising
- Bone, joint, and muscle pain
- Blood sugar changes
- Nerve damage (especially in hands and feet)
- Fluid around the lungs (pleural effusion)
- Heart complications (heart attack, heart failure)
- High potassium (hyperkalemia) – can be life-threatening
- Infection risk rises sharply
- Malnutrition and weakened bones (osteoporosis, fracture risk)
- Reproductive issues (fertility problems, miscarriage)
- Restless legs syndrome
- Stroke, seizures, and cognitive changes or dementia
Treatment Approaches for IgA Nephropathy
There is no cure for IgA nephropathy, but proper management can slow its progression and reduce complications. Treatments are tailored according to disease severity:
- Blood pressure control: ACE inhibitors or ARBs to reduce proteinuria and slow kidney damage.
- Immunosuppressive drugs: Corticosteroids and other immunosuppressants may be prescribed in selected cases to reduce immune activity.
- Cholesterol management: Statins may be recommended to manage high cholesterol and reduce cardiovascular risk.
- Dietary modifications: Reducing sodium, protein, and cholesterol intake as directed by a nephrologist.
- Treatment of swelling: Diuretics may reduce fluid retention and edema.
- Close monitoring: Regular lab tests and follow-up to track kidney function, protein, and blood pressure.
Delaying Progression to ESRD
Modern therapies and better understanding of early markers have improved outcomes for many patients with IgA nephropathy. Key strategies include:
- Adherence to prescribed blood pressure and cholesterol therapies
- Avoiding non-steroidal anti-inflammatory drugs (NSAIDs) and other nephrotoxic medications
- Maintaining a healthy weight and balanced nutrition
- Promptly treating infections, as upper respiratory illnesses can trigger flares
Kidney Transplant and Dialysis: When the Kidneys Fail
For individuals whose IgA nephropathy advances to ESRD, treatment options become more limited but essential for survival:
- Dialysis: Mechanical filtration of blood, necessary when the kidneys no longer function.
- Kidney transplantation: May offer better quality of life and function, but not a cure—IgA nephropathy can return in the new kidney.
Challenges After Transplantation
Kidney transplantation offers hope but comes with distinct challenges:
- Up to 19% of transplant recipients may experience a recurrence of IgA nephropathy within 10 years.
- Among those who receive a transplant for IgA nephropathy, up to 40% of transplanted kidneys may ultimately fail due to disease recurrence or other complications.
- Donor kidney shortages remain a major hurdle, with far more candidates than available organs each year.
Frequently Asked Questions (FAQs)
What causes IgA nephropathy?
The exact cause is unknown. It is believed to be an autoimmune condition where abnormal immune responses trigger the accumulation of IgA antibodies in the kidneys, leading to inflammation and damage.
Is IgA nephropathy hereditary?
Genetics play a role, as it is more common in people with a family history of IgA nephropathy or IgA vasculitis. However, environmental and other factors are also involved.
Can IgA nephropathy be cured?
Currently, there is no cure, but treatment can manage symptoms and slow the progression of kidney damage.
What is the life expectancy for someone with IgA nephropathy?
Prognosis varies: Some have mild disease with little progression, while others experience rapid decline. Early intervention improves outcomes, and many live many years with proper management. However, up to 20% develop kidney failure within a decade of diagnosis.
Can IgA nephropathy return after kidney transplant?
Yes, IgA nephropathy often recurs after kidney transplantation. In about 19% of transplant recipients, the condition redevelops in the new kidney within 10 years, potentially leading to transplant failure.
Patient Tips for Living with IgA Nephropathy
- Maintain regular follow-up with a nephrologist and keep all appointments.
- Monitor blood pressure and report significant changes to your care team.
- Follow dietary guidance from your healthcare team.
- Report new symptoms, especially swelling or changes in urine color, immediately.
- Stay informed about new research and treatment options.
Summary Table: IgA Nephropathy vs End-Stage Renal Disease
| Aspect | IgA Nephropathy | End-Stage Renal Disease (ESRD) |
|---|---|---|
| Disease Nature | Autoimmune, gradual kidney damage | Complete kidney failure, need for replacement therapy |
| Symptoms | Blood/protein in urine, swelling, hypertension | Uremia, severe fatigue, persistent swelling, multi-system effects |
| Diagnosis | Urine tests, kidney biopsy | Blood and urine tests, clinical evaluation |
| Treatment | Blood pressure control, immunosuppression, monitoring | Dialysis, kidney transplant, supportive therapies |
| Long-Term Outlook | Variable; some reach remission, others progress to ESRD | Lifelong therapy needed; transplant may be possible |
Conclusion
IgA nephropathy is a significant cause of chronic kidney disease and failure worldwide. Early identification, continuous monitoring, and comprehensive management are crucial in preventing progression to end-stage renal disease. While challenges remain—especially regarding organ transplant and recurrent disease—ongoing advancements in research and treatment are helping to change outcomes for the better.
References
- https://www.webmd.com/a-to-z-guides/iga-nephropathy-challenges-renal-disease
- https://www.healthline.com/health/kidney-disease/iga-nephropathy-and-end-stage-renal-disease
- https://www.kidneyfund.org/all-about-kidneys/other-kidney-diseases/iga-nephropathy
- https://www.ncbi.nlm.nih.gov/books/NBK538214/
- https://www.mayoclinic.org/diseases-conditions/iga-nephropathy/symptoms-causes/syc-20352268
- https://my.clevelandclinic.org/health/diseases/5990-iga-nephropathy
- https://rarediseases.org/rare-diseases/iga-nephropathy/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11648327/
Read full bio of Sneha Tete












