IBS vs. Diverticulitis: Understanding Differences, Causes, and Treatments
A comprehensive comparison of IBS and diverticulitis, including symptoms, causes, risk, diagnosis, and management strategies.
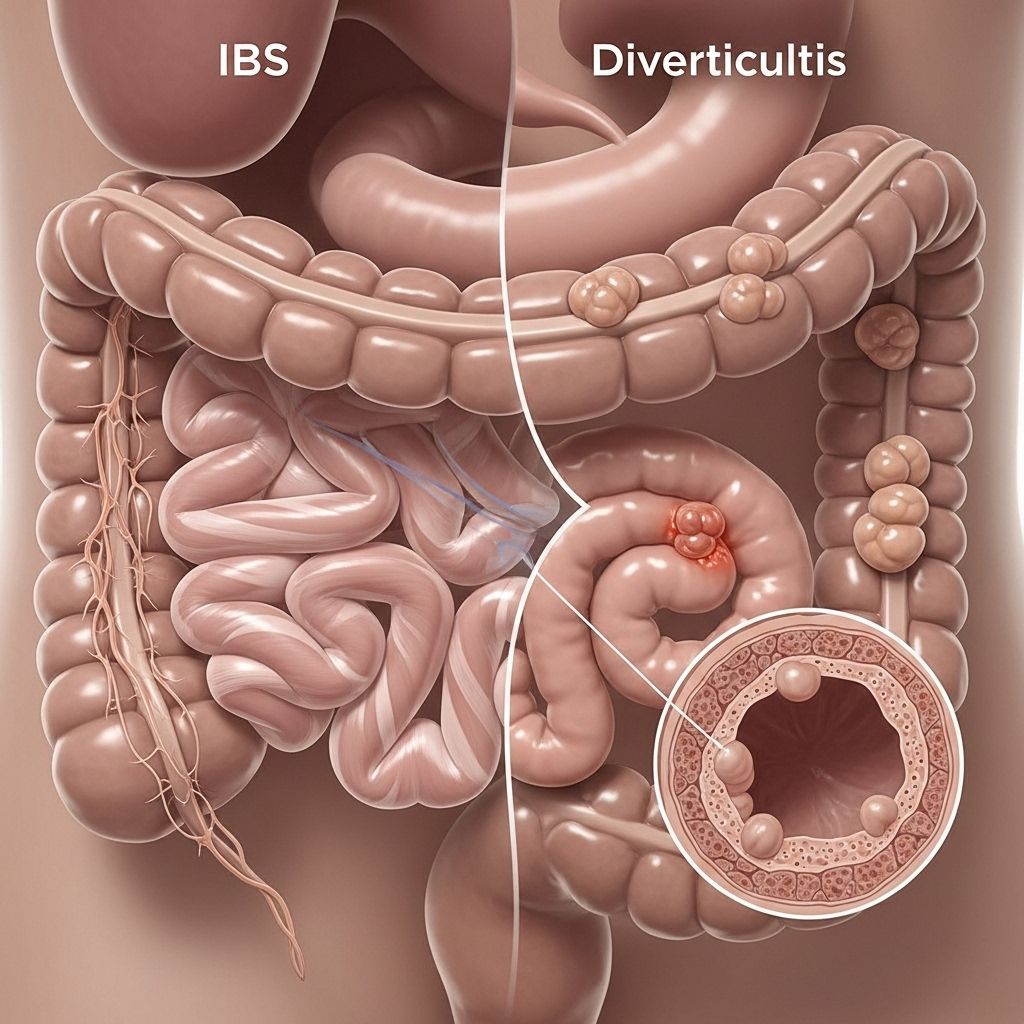
Irritable bowel syndrome (IBS) and diverticulitis are both common gastrointestinal conditions, but they differ in causes, symptoms, risk factors, and management. Recognizing the distinctions between them is crucial for receiving appropriate care and managing symptoms effectively.
Overview: What Are IBS and Diverticulitis?
Irritable bowel syndrome (IBS) is a chronic functional disorder of the digestive system. It primarily affects the large intestine (colon) and causes a cluster of symptoms including abdominal pain, bloating, changes in bowel movements, and general discomfort. IBS is considered a “functional” disorder, meaning no structural abnormalities are visible during routine tests.
Diverticulitis, by contrast, is an acute complication that arises when small pouches known as diverticula in the wall of the colon become inflamed or infected. These pouches often form due to pressure on weakened spots in the intestinal wall— a condition called diverticulosis. Diverticulosis may be symptomless, but once inflammation or infection sets in, diverticulitis can cause severe abdominal pain and potential complications impacting health.
How Do IBS and Diverticulitis Differ?
| IBS | Diverticulitis | |
|---|---|---|
| Common Symptoms |
|
|
| Causes | Not completely known; may involve gut nerve sensitivity, motility disturbances, stress, genetics | Inflammation of colon pouches (diverticula) due to infection |
| Prevalence | Affects about 10–15% of the population |
Understanding how IBS presents can vary between genders is crucial for effective management. For a detailed comparison of how IBS symptoms differ between men and women, check out our guide on IBS Symptoms in Men and Women: Key Differences. |
| Sex Differences | 1.5 to 2 times more common in women than men |
|
| Typical Age | Most commonly affects people younger than 50 | More common in older adults; average age of hospitalization is 63 years |
Key Symptoms: Comparison
IBS Symptoms
- Abdominal pain or cramping, often relieved by passing stool
- Bloating and excessive gas
- Changes in bowel movement patterns, typically alternating between diarrhea and constipation
- Urgency following eating (sometimes)
- Mucus in stool
- A persistent sensation of incomplete evacuation
Diverticulitis Symptoms
- Persistent abdominal pain, usually on the lower left side
- Fever and chills
- Nausea and vomiting
- Constipation or, less often, diarrhea
- Bloating or swelling in the abdomen
- Rectal bleeding (sometimes)
- Increased urinary urgency or frequency (occasional)
Causes and Risk Factors
Causes of IBS
- Exact cause unknown. IBS is believed to involve:
- Abnormalities in gut-brain signaling
- Changes in gut motility (how quickly food moves through the bowel)
- Heightened sensitivity of intestinal nerves
- Influence of stress or hormonal changes
- History of gastrointestinal infection
- Genetics/family history
- Symptom triggers can include specific foods, emotional stress, medication changes, and infections.
Causes of Diverticulitis
- Diverticulosis (formation of pouches) typically arises due to years of pressure on weak spots in the colon wall.
- Low-fiber diets common in industrialized countries contribute to increased risk by promoting constipation and increased bowel pressure.
- Diverticulitis develops when a pouch becomes blocked by stool, allowing bacteria to multiply and cause infection or inflammation.
Who Is Most at Risk?
- IBS is most common in individuals under 50 years old and is more prevalent among women.
- Diverticulitis risk increases with age; it becomes common in adults over 60 and is more frequent in men under 50, but in women over 50.
- Dietary and lifestyle factors—especially low fiber intake, obesity, smoking, and sedentary lifestyle—raise the risk for diverticulosis and thus diverticulitis.
- Family history and genetics may play a role in both conditions.
How Are IBS and Diverticulitis Diagnosed?
IBS Diagnosis
- IBS is diagnosed based on:
- Typical symptom pattern (abdominal discomfort with bowel habit changes)
- Detailed medical and family history
- Physical examination
- Exclusion of other conditions (such as celiac disease or inflammatory bowel disease)
- IBS is a functional disorder; routine tests and colonoscopy typically appear normal.
Diverticulitis Diagnosis
- Diverticulitis is detectable in tissue and often diagnosed through:
- Blood tests to look for infection or inflammation
- Imaging tests, such as CT scan, to visualize inflamed pouches
- Physical examination for abdominal tenderness
- Review of medical history and symptoms
- Colonoscopy (usually after acute infection has resolved)
Complications and Associations: Can IBS Cause Diverticulitis?
- There is little evidence that IBS directly causes diverticulitis.
- However, individuals with diverticulitis can later develop IBS-like symptoms. This is known as Post-Diverticulitis Syndrome, or Post-Diverticulitis Irritable Bowel Syndrome (PDV–IBS).
- Persistent gastrointestinal and mood symptoms may occur after recovery from acute diverticulitis.
How Are These Conditions Managed and Treated?
Treatment for IBS
- Dietary management, particularly increasing fiber intake for those with constipation-predominant IBS (not always appropriate for all types)
- Identifying and avoiding food triggers, such as high-FODMAP foods, lactose, or gluten
- Medications to address specific symptoms (anti-spasmodics for pain, laxatives for constipation, anti-diarrheal medication as needed)
- Managing stress through behavioral therapies, mindfulness, regular exercise, and sleep hygiene
- Counseling or psychological support for those whose symptoms worsen with stress or mood changes
Treatment for Diverticulitis
- Mild cases may be managed at home with rest, a liquid or low-fiber diet, and oral antibiotics if infection is suspected
- Severe cases (including those with uncontrolled pain, high fever, or complications) often require hospitalization, intravenous antibiotics, and, in rare cases, surgical removal of the affected portion of the colon
- Avoiding foods high in seeds or nuts is no longer routinely recommended, as evidence shows these are not significant risks for flare-ups
- Recovery includes gradually increasing fiber intake after infection resolves, to prevent future diverticular disease
Prevention Strategies
Preventing IBS Flare-Ups
- Maintain regular, balanced meals
- Include soluble fiber in the diet (oats, fruits, vegetables)
- Avoid known trigger foods and drinks (spicy foods, caffeine, alcohol)
- Practice stress-reduction techniques
- Stay active with regular exercise
Preventing Diverticulitis
- Follow a high-fiber diet for healthy colon function and regular bowel movements
- Drink plenty of fluids daily
- Engage in regular physical activity
- Treat constipation proactively to help prevent pouch formation
- Avoid smoking, as it increases risk for complications
Frequently Asked Questions (FAQs)
Q: How can I tell if my abdominal symptoms are IBS or diverticulitis?
A: IBS pain often fluctuates and is relieved by bowel movements, while diverticulitis pain is typically constant, focused on the lower left abdomen, and may be accompanied by fever or nausea.
Q: Is there a risk that IBS will become diverticulitis?
A: There is no current scientific evidence to suggest IBS turns into diverticulitis. They are distinct conditions with separate causes.
Q: Are there foods I should avoid to prevent either IBS or diverticulitis flare-ups?
A: IBS management is highly individual—quickly identifying and excluding trigger foods is important. For diverticulitis, focus on eating a higher-fiber diet once the inflammation has resolved; previously avoided foods like seeds and nuts are generally safe for most people.
Q: Can both IBS and diverticulitis be managed without medication?
A: Mild cases of either condition may be managed with dietary adjustments and lifestyle changes, but severe diverticulitis should always be addressed by a healthcare professional and may require antibiotics or other interventions.
Q: Should I request a colonoscopy?
A: A colonoscopy is often recommended for those at risk of colorectal cancer, for those over the age of 50, or if other serious illnesses are suspected. IBS diagnosis typically does not require colonoscopy unless “red flag” symptoms like unexplained weight loss or bleeding are present. Diverticulitis is diagnosed by imaging, especially during an acute episode.
Takeaway
Both IBS and diverticulitis affect the colon and may cause overlapping symptoms, but they differ markedly in their causes, complications, age distribution, and treatments. Clear diagnosis is essential for tailored management. Sustained dietary and lifestyle changes, in consultation with your healthcare provider, can help minimize the impact of both conditions and maintain digestive health over time.
References
- https://www.emedicinehealth.com/diverticular_diverticulitis_ibs_irritable_bowel/article_em.htm
- https://www.healthline.com/health/irritable-bowel-syndrome/clinical-growth-whats-the-difference-between-ibs-and-diverticulitis
- https://evinature.com/blog/gut-health/diverticulitis-vs-ibs/
- https://www.uclahealth.org/news/release/ucla-researchers-discover-new-form-of-irritable-bowel-syndrome
- https://pubmed.ncbi.nlm.nih.gov/22572688/
- https://karger.com/ddi/article/30/1/64/95907/Is-It-Diverticular-Disease-or-Is-It-Irritable
- https://iffgd.org/gi-disorders/other-disorders/diverticulosis-and-diverticulitis/diverticula-diverticulosis-diverticulitis-what-s-the-difference/
Read full bio of medha deb












