IBS vs Diverticulitis: Understanding Key Differences, Causes & Treatments
Learn about the distinct causes, symptoms, diagnosis, and treatment options for IBS and diverticulitis to better manage your digestive health.
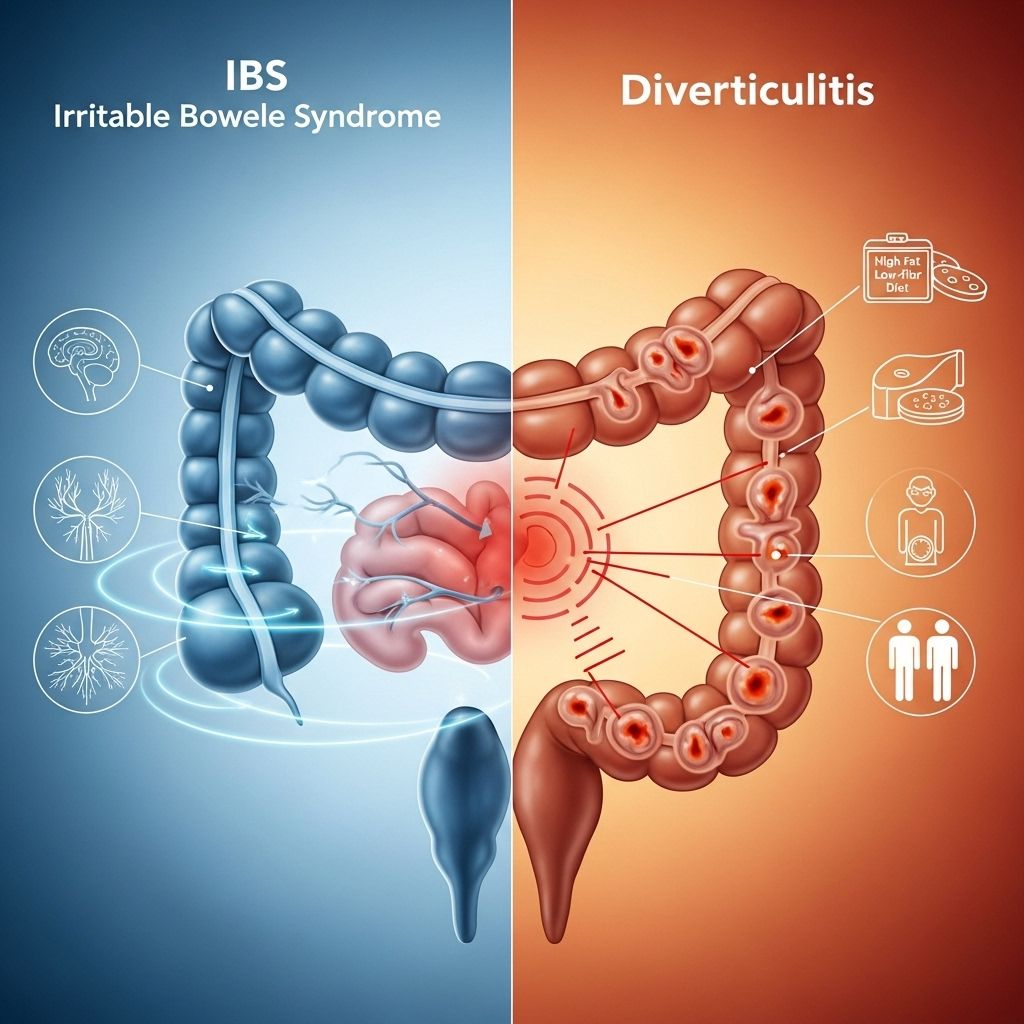
IBS vs Diverticulitis: What Sets Them Apart?
Irritable Bowel Syndrome (IBS) and diverticulitis are two common digestive conditions that are often confused, yet each has unique causes, symptoms, and treatment paths. Understanding their differences is essential for correctly managing your health and seeking adequate care.
Quick Overview Table
| IBS | Diverticulitis | |
|---|---|---|
| Common Symptoms | Constipation, abdominal pain, cramps, bloating, diarrhea | Constipation, abdominal pain, nausea, vomiting, fever, diarrhea (less frequent) |
| Main Cause | Not completely known; functional gut disorder | Inflammation and infection of pockets (diverticula) in intestines |
| Prevalence | 10-15% of people | 15% of people over 60 with diverticulosis; ~200,000 annual US hospitalizations |
| Sex Differences | More common in women (1.5-2x) | More common in men under 50, women over 50 |
| Typical Age | Under 50 | Older adults (average hospital age 63) |
What is IBS?
Irritable Bowel Syndrome (IBS) is a chronic gastrointestinal disorder marked by unpredictable abdominal pain, bloating, and changes in bowel habits. Unlike diverticulitis, IBS doesn’t cause inflammation or visible changes to digestive organs and is classified as a functional disorder, meaning symptoms arise without any detectable structural abnormalities in the gut.
IBS affects an estimated 10-15% of people worldwide, especially those under age 50, and is up to twice as common in women.
What are the Symptoms of IBS?
- Persistent abdominal pain (often relieved by bowel movement)
- Bloating
- Gas
- Constipation alternating with diarrhea
- Mucus in stool
- Abdominal distension or swelling
- Sense of incomplete bowel evacuation
IBS symptoms often flare periodically and can be triggered by stress, diet changes, hormonal fluctuations, or infections.
What Causes IBS?
- Unknown precise cause; likely a combination of factors
- Disrupted gut-brain axis
- Altered nervous system signals affecting gut motility
- Genetics (family history)
- Diet sensitivities, stress, infections, hormones
Common theories suggest that IBS results from food moving too fast or too slow through the digestive tract, oversensitive gut nerves, and poor communication between the brain and gut.
What is Diverticulitis?
Diverticulitis develops when small pouches (diverticula) form in weak areas of the colon wall—the effect of diverticulosis—and one or more become inflamed or infected, usually from stool trapped inside these pouches.
Diverticulosis can be present with no symptoms and is highly prevalent in people over 50. Around 15% of those with diverticulosis will develop diverticulitis, most commonly after age 60.
Symptoms of Diverticulitis
- Intense, constant pain (usually lower left abdomen)
- Constipation or diarrhea
- Fever and chills
- Nausea and vomiting
- Abdominal swelling and bloating
- Rectal bleeding (sometimes)
- Painful or frequent urination
Pain with diverticulitis is often severe, constant, and may increase with movement or touch. In many Western countries, diverticula more commonly affect the left side of the colon, while in people of Asian descent, the right side may be affected.
What Causes Diverticulitis?
- Inflammation and infection of diverticula (colon wall pouches)
- Usually due to bacteria in stool becoming trapped
- Diverticulosis primarily results from increased pressure in the colon, often caused by a low-fiber diet
Diverticulitis can occur as a single episode or recur, and its risk increases with age.
How Are IBS and Diverticulitis Diagnosed?
Because IBS does not cause structural abnormalities, diagnosis relies on reported symptoms, physical exam, and medical history. There are no lab tests or imaging to definitively diagnose IBS, though doctors may perform tests to exclude other illnesses.
Diverticulitis, on the other hand, is diagnosed through medical imaging (such as CT scans), blood tests, and stool cultures, which look for signs of infection, inflammation, or bleeding. A colonoscopy may be used once acute symptoms resolve.
- IBS is diagnosed by exclusion—confirming typical symptoms and ruling out other causes
- Diverticulitis requires visible evidence of infection or inflammation in tissue
Can IBS Cause Diverticulitis?
Current research does not support that IBS directly causes diverticulitis. However, people who have experienced diverticulitis may develop IBS-like symptoms afterward—sometimes called Post-Diverticulitis Syndrome. Additionally, both conditions can coexist or present similar digestive complaints, making thorough evaluation essential for accurate diagnosis and appropriate management.
Key Differences Between IBS and Diverticulitis
- IBS pain is usually relieved with a bowel movement; diverticulitis pain is persistent and severe.
- IBS does not produce fever; diverticulitis may cause high fever and infection signs.
- IBS alternates between constipation and diarrhea; diverticulitis tends toward constipation and may also cause diarrhea.
- Diverticulitis can lead to complications requiring surgery; IBS rarely needs surgical intervention.
- Diverticulitis is visible as inflammation on imaging; IBS is a functional diagnosis.
Treatment Strategies for IBS and Diverticulitis
IBS Treatment Options
- Increase dietary fiber (gradually and as tolerated)
- Reduce triggers such as caffeine, fatty foods, and artificial sweeteners
- Manage stress and anxiety through relaxation techniques
- Regular balanced meals
- Exercise regularly
- Avoid smoking
- Consider prescription medications for severe cases (spasmolytics, antidepressants, or medications targeting gut motility)
IBS is typically managed with lifestyle changes and symptom-based treatments rather than curative interventions.
Diverticulitis Treatment Options
- Mild cases: Rest, clear liquid diet, antibiotics
- Severe cases: Hospitalization, intravenous antibiotics
- Surgery for complications (abscesses, perforations, recurrent episodes)
- Long-term management includes a high-fiber diet to prevent new diverticula formation
- Consulting with a healthcare professional on the best dietary guidelines for prevention and recovery
Unlike IBS, diverticulitis can lead to life-threatening complications if left untreated, making prompt medical attention critical during acute episodes.
Prognosis and Long-term Outlook
- IBS is a chronic but non-life-threatening condition. Its symptoms can be managed effectively with lifestyle modifications, although relapses are common.
- Diverticulitis is potentially serious. Recovery depends on early diagnosis and adequate treatment. Recurrence can be minimized with dietary adjustments and regular medical surveillance.
- With proper management, most people can maintain a high quality of life.
Preventive Measures
- Adopt a high-fiber diet with vegetables, fruits, whole grains
- Stay hydrated
- Exercise regularly
- Manage stress
- Limit processed foods
- Consult your healthcare provider when experiencing unusual digestive symptoms
Long-term prevention for diverticulitis focuses on dietary fiber and general gut wellness, while IBS prevention is more individualized and based on avoiding triggers.
Frequently Asked Questions (FAQs)
Q: How can I tell if my abdominal pain is IBS or diverticulitis?
IBS pain is often cyclical, comes and goes, and is relieved after bowel movements. Diverticulitis pain is severe, persistent, and usually localized to the lower left abdomen. Fever, nausea, and rectal bleeding point more toward diverticulitis.
Q: Is IBS dangerous compared to diverticulitis?
IBS is not considered dangerous, though symptoms can affect your quality of life significantly. Diverticulitis, particularly untreated cases, can lead to serious complications and may require urgent medical or surgical treatment.
Q: Can lifestyle changes prevent both conditions?
A high-fiber diet, physical activity, and stress reduction benefit both conditions, but diverticulitis also requires attention to infection risk, and IBS management may involve additional dietary adjustments and psychological strategies.
Q: Are IBS and diverticulitis related?
While both affect the digestive tract and can have overlapping symptoms, their causes are distinct. Studies suggest having diverticulitis may lead to IBS-like symptoms in some cases, called Post-Diverticulitis Syndrome.
Q: Who is at risk for IBS and diverticulitis?
IBS often affects younger people and women, while diverticulosis/diverticulitis mainly impacts older adults. A low-fiber diet and inactivity increase risk for diverticulitis, while IBS may be linked to genetics, stress, and gut sensitivity.
Takeaway Message
Recognizing the distinct features, symptoms, causes, and treatments for IBS and diverticulitis empowers you to seek proper medical help, make lifestyle adjustments, and prevent serious complications. When persistent abdominal symptoms occur, timely diagnosis and intervention are crucial for health and quality of life.
References
- https://www.emedicinehealth.com/diverticular_diverticulitis_ibs_irritable_bowel/article_em.htm
- https://www.healthline.com/health/irritable-bowel-syndrome/clinical-growth-whats-the-difference-between-ibs-and-diverticulitis
- https://evinature.com/blog/gut-health/diverticulitis-vs-ibs/
- https://www.healthpartners.com/blog/diverticulosis-vs-diverticulitis/
- https://pubmed.ncbi.nlm.nih.gov/22572688/
- https://karger.com/ddi/article/30/1/64/95907/Is-It-Diverticular-Disease-or-Is-It-Irritable
- https://www.uclahealth.org/news/release/ucla-researchers-discover-new-form-of-irritable-bowel-syndrome
Read full bio of medha deb












