IBS vs. Celiac Disease: Differences, Similarities, and Diagnosis
Understand how IBS and celiac disease differ, overlap, and what steps to take for accurate diagnosis and treatment.
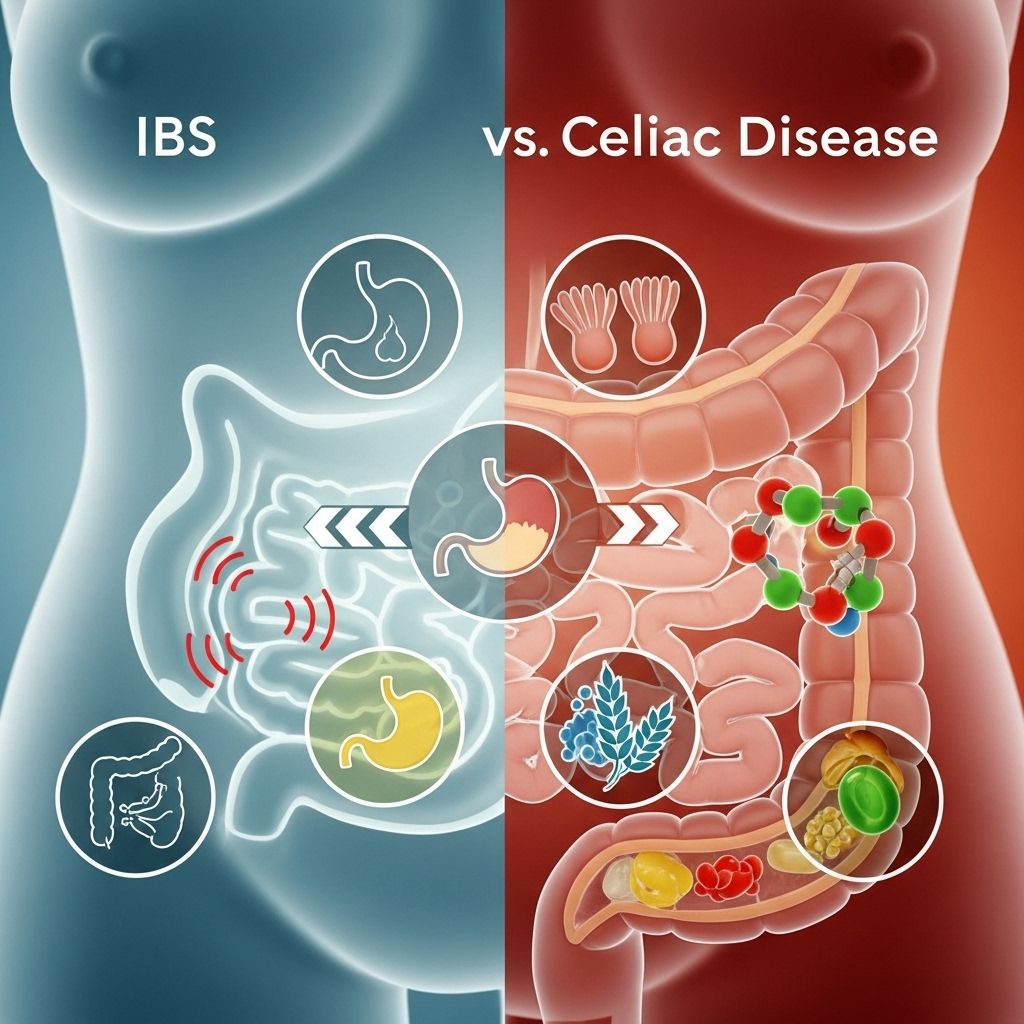
Digestive discomfort can drastically affect quality of life, and understanding the root cause is key to managing symptoms. Two of the most common and often confused digestive conditions are irritable bowel syndrome (IBS) and celiac disease. Although they share certain symptoms, they are distinct in their causes, long-term risks, and treatments. This article explains the key differences, similarities, symptoms, diagnosis, and treatment of IBS and celiac disease to help you navigate potential gastrointestinal health challenges.
IBS and Celiac Disease: An Overview
Irritable bowel syndrome (IBS) is a group of symptoms affecting digestive function. The condition involves abdominal pain, changes in bowel movements, and discomfort, but without identifiable damage to the digestive tract. The exact cause is unknown and may involve multiple factors such as stress, hormonal changes, or food sensitivities.
Celiac disease is a chronic autoimmune disorder where gluten—the protein in wheat, barley, and rye—triggers the immune system to damage the small intestine lining. This can result in nutrient malabsorption, immune complications, and, if untreated, long-term health problems.
Key Differences Between IBS and Celiac Disease
| Feature | IBS | Celiac Disease |
|---|---|---|
| Nature | Functional gastrointestinal disorder (not linked to damage or inflammation of intestines) | Autoimmune disease (immune attack on intestines in response to gluten) |
| Main Triggers | Various foods, stress, hormones (varies by individual) | Gluten proteins in wheat, barley, rye |
| Symptoms | Abdominal pain, cramping, bloating, constipation and/or diarrhea | Diarrhea, abdominal pain, bloating, weight loss, nutrient deficiencies, skin rashes, mouth sores |
| Body Damage? | No physical damage to intestines | Damage to the lining of the small intestine |
| Genetic Links | Very limited or uncertain | Strong—family history and certain genes (such as HLA-DQ2, HLA-DQ8) |
| Long-term Risks | Symptom burden, impaired quality of life | Malnutrition, osteoporosis, infertility, higher risk for other autoimmune disorders |
| Treatment | Dietary changes and symptom management (medication, stress reduction) | Strict lifelong gluten-free diet |
Symptoms: How IBS and Celiac Disease Overlap and Differ
Although IBS and celiac disease both disrupt digestive health, their symptoms are not identical. Their overlap can make self-diagnosis challenging.
Common IBS symptoms
- Cramping or abdominal pain, often relieved by bowel movement
- Bloating and gas
- Changes in stool: diarrhea, constipation, or both (IBS with constipation, IBS with diarrhea, or mixed form)
- Mucus in the stool
- No blood or weight loss typical
Common Celiac Disease symptoms
- Diarrhea (especially chronic, foul-smelling, or fatty)
- Abdominal pain and bloating
- Weight loss or inability to gain weight
- Fatigue, weakness, or anemia
- Itchy skin rashes (dermatitis herpetiformis)
- Mouth ulcers, dental enamel defects, joint pain
- Headaches, nerve tingling or numbness
- Delayed growth in children
It’s important to note:
- IBS does not cause physical damage or increase risks for other diseases.
- Celiac disease may lead to permanent small intestine damage and serious complications if left untreated.
What Causes IBS and Celiac Disease?
IBS Causes
- The exact cause of IBS isn’t fully known.
- Contributing factors include:
- Gut-brain miscommunication
- Abnormal intestinal muscle contractions
- Increased gut sensitivity
- Stress or anxiety
- Hormonal changes
- Certain foods or drinks
- No clear genetic or autoimmune component
Celiac Disease Causes
- Autoimmune reaction to gluten in genetically susceptible individuals
- Requires specific genes (most commonly HLA-DQ2 or HLA-DQ8)
- Triggers may include:
- Infections
- Pregnancy
- Physical trauma or stress
- Other autoimmune disorders
- Both adults and children can develop celiac disease, sometimes after exposure to gluten or a stressful event
Who Gets IBS vs. Who Gets Celiac Disease?
- IBS is very common. Estimates suggest 10–15% of adults in Western countries experience IBS symptoms at some point.
- Celiac disease affects about 1% of the general population.
- Both conditions can occur in adults and children.
- Celiac disease has a higher risk if you have a first-degree relative with the disease or already have an autoimmune disorder.
Complications: Long-Term Effects of Each Condition
IBS
- Does not damage bowel tissue or increase cancer risk
- Can cause severe and persistent symptoms, affecting quality of life
- May lead to missed work, anxiety, or depression due to chronic symptoms
Celiac Disease
- Untreated, leads to chronic inflammation of the small intestine
- Malnutrition (deficiencies in iron, calcium, folate, and vitamins D and B12)
- Osteoporosis, infertility, miscarriage, neurological conditions
- Higher risk for certain cancers, especially intestinal lymphoma
Diagnosing IBS vs. Celiac Disease
Both conditions require a doctor’s evaluation for correct diagnosis.
How is IBS Diagnosed?
- Diagnosis of exclusion (no other identifiable cause)
- Rome IV criteria: Symptoms of abdominal pain/discomfort with altered bowel habits (onset at least 6 months prior and present 1 day/week in the last 3 months)
- Additional tests (blood, stool, colonoscopy) may be used to rule out other diseases
How is Celiac Disease Diagnosed?
- Blood tests for anti-tTG, EMA, and DGP antibodies (while the person is still eating gluten)
- Intestinal biopsy confirms damage to the villi in the small intestine
- Genetic testing (optional) for HLA-DQ2 or HLA-DQ8 may support diagnosis
- Symptoms typically improve on a strict gluten-free diet
Can You Have Both IBS and Celiac Disease?
Yes, some individuals may have both conditions. Studies suggest celiac disease is about 4- to 5-fold more common in people with symptoms of IBS than the general population. Even after starting a gluten-free diet, some people with celiac disease may continue to have IBS-like symptoms due to gut sensitivity or other factors. Diagnosis and treatment should be individualized and monitored by a healthcare provider.
Managing IBS and Celiac Disease
IBS Management
- Individualized dietary changes (e.g., low FODMAP diet, avoiding trigger foods)
- Stress management and mental health support
- Medications for symptom relief (antispasmodics, laxatives, anti-diarrheals, sometimes antidepressants)
- Probiotics and fiber supplements, when appropriate
Celiac Disease Management
- Strict, lifelong gluten-free diet
- Education about cross-contamination and hidden sources of gluten
- Monitoring for nutritional deficiencies; vitamin or mineral supplementation if necessary
- Regular follow-up to check antibody levels and intestinal healing
- Screening for associated autoimmune conditions
Other Possible Overlapping Conditions
- Non-celiac gluten sensitivity (NCGS): Symptoms similar to celiac, but without immune damage or antibodies (diagnosis of exclusion)
- Wheat allergy: Involves allergic (IgE-mediated) response; different from celiac or NCGS
- Inflammatory bowel disease (IBD): Diseases like Crohn’s and ulcerative colitis involve inflammation and physical damage, but are different from both IBS and celiac disease
Frequently Asked Questions (FAQs)
How can I tell if my symptoms are caused by IBS or celiac disease?
Because both conditions share similar symptoms such as abdominal pain and changes in bowel movements, only medical evaluation with blood tests and, if needed, a biopsy can accurately distinguish between IBS and celiac disease.
Can I diagnose myself with celiac disease by cutting out gluten?
No. Removing gluten before testing can affect results, leading to an incorrect or missed diagnosis. Always consult a doctor before making significant dietary changes.
Is it possible to have both IBS and celiac disease at the same time?
Yes, some people with celiac disease continue to have IBS-like symptoms despite following a gluten-free diet. There is also a higher prevalence of celiac disease among those with IBS compared to the general population.
What foods should I avoid for IBS versus celiac disease?
- For IBS: Avoid foods that trigger your individual symptoms (often high in FODMAPs, fatty foods, caffeine, certain artificial sweeteners).
- For celiac disease: Avoid all foods containing gluten (wheat, barley, rye), including processed foods with hidden gluten.
Will symptoms go away if I manage my condition correctly?
With effective management—whether a gluten-free diet for celiac disease or lifestyle and dietary modifications for IBS—most people see a significant improvement in symptoms and quality of life.
When to See a Doctor
If you have persistent digestive symptoms—such as diarrhea, constipation, weight loss, fatigue, or abdominal pain—consult a healthcare professional. Accurate diagnosis is essential for safe and effective treatment. Never self-diagnose or start restrictive diets without expert guidance, as this may mask conditions or cause nutritional harm.
Summary Table: IBS vs. Celiac Disease at a Glance
| Aspect | IBS | Celiac Disease |
|---|---|---|
| What Is It? | Functional bowel disorder | Autoimmune, gluten-triggered |
| Main Symptoms | Abdominal pain, diarrhea/constipation, gas | Diarrhea, abdominal pain, malabsorption, extra-intestinal symptoms |
| Body Damage? | No | Yes, small intestine villi |
| Diagnosis | By symptoms, exclusion of other diseases | Gluten-containing diet, blood tests, biopsy |
| Treatment | Diet, stress reduction, medications as needed | Lifelong strict gluten-free diet |
Key Takeaways
- IBS and celiac disease are common, chronic digestive conditions with some overlapping symptoms but different causes, risks, and treatments.
- IBS involves functional symptoms without physical bowel damage, while celiac disease involves an immune response to gluten, leading to intestinal injury and systemic complications.
- Professional evaluation is essential to distinguish between them and develop an individualized treatment plan.
References
- https://www.medicalnewstoday.com/articles/ibs-vs-celiac
- https://windsordigestivehealth.com/ibs-vs-celiac-disease-the-difference-explained/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3480312/
- https://www.webmd.com/ibs/celiac-disease-ibs
- https://www.cdc.gov/inflammatory-bowel-disease/about/myths.html
- https://celiac.org/fodmaps-and-celiac-disease/
- https://www.thermofisher.com/celiac/wo/en/clinical/case-studies/celiac-disease-versus-IBS.html
Read full bio of Sneha Tete












