IBS-M: Understanding Mixed-Type Irritable Bowel Syndrome – Causes, Symptoms, and Treatment
Explore IBS-M, its distinct symptoms, causes, and learn about diagnostic methods and management strategies for improved digestive health.
IBS-M: Understanding Mixed-Type Irritable Bowel Syndrome
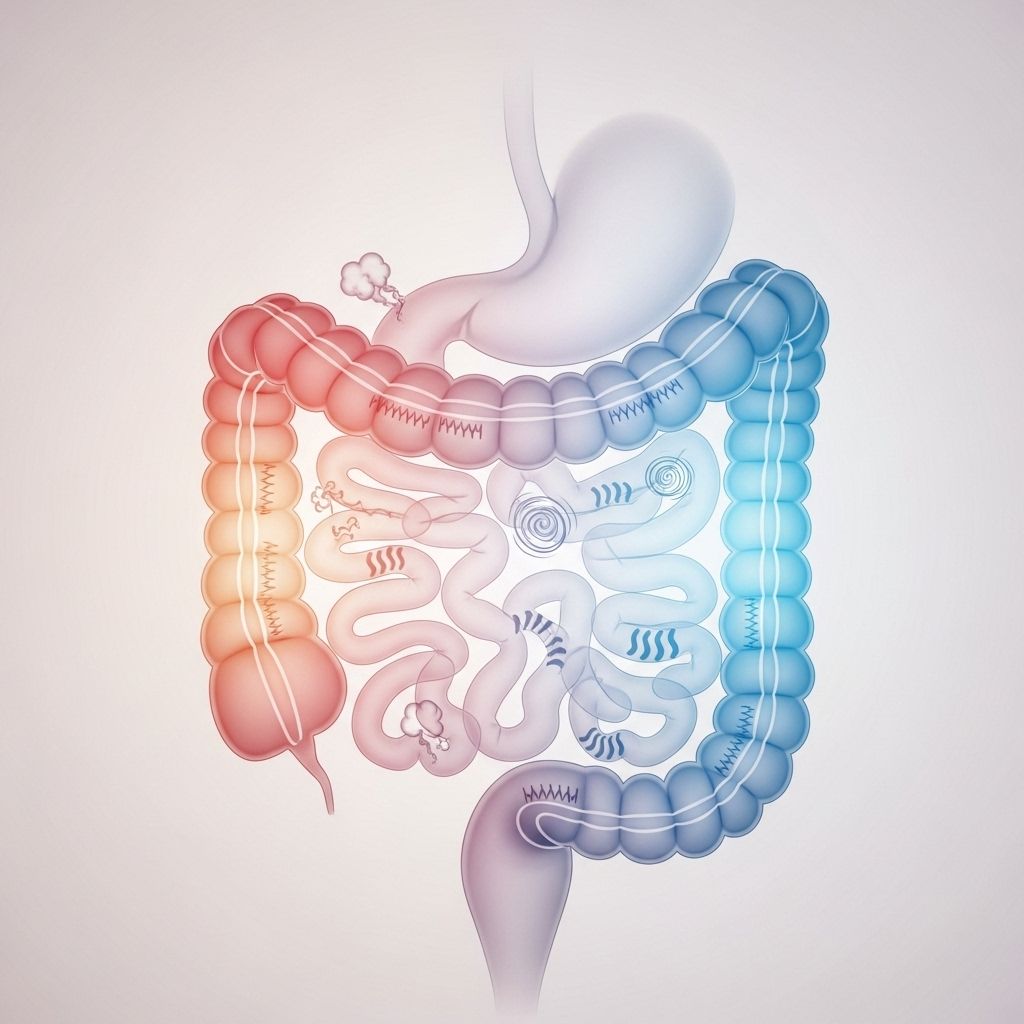
IBS-M (mixed-type irritable bowel syndrome) is a chronic digestive disorder marked by alternating symptoms of diarrhea and constipation, accompanied by abdominal pain and discomfort. It is a subgroup of irritable bowel syndrome (IBS), a functional gastrointestinal disorder that significantly impacts daily life and well-being.
What is IBS-M?
IBS-M stands for irritable bowel syndrome with mixed bowel habits. This subtype of IBS is characterized by recurrent abdominal symptoms plus alternating periods of diarrhea and constipation. People with IBS-M experience:
- Abdominal pain and cramping tied to bowel movements
- Frequent changes between loose and hard stools
- Bloating, gas, and stomach discomfort
While IBS-M shares features with other IBS subtypes (IBS-D for diarrhea-predominant and IBS-C for constipation-predominant), its chief distinction is the regular alternation between these extremes.
Symptoms of IBS-M
- Abdominal pain and discomfort: Often relieved or worsened by bowel movements
- Constipation: Hard, dry, or infrequent stools
- Diarrhea: Loose, watery, or urgent bowel movements
- Bloating and excess gas
- Change in stool appearance: Alternating between loose and hard
- A feeling of incomplete evacuation after a bowel movement
- Mucus in stool
Other non-digestive symptoms such as fatigue, insomnia, anxiety, and depression are also common among IBS patients.
IBS-M vs. Other IBS Types: At a Glance
| IBS Subtype | Main Symptoms | Stool Pattern |
|---|---|---|
| IBS-M (Mixed) | Abdominal pain, alternating diarrhea & constipation | Switches between hard & loose stools |
| IBS-D (Diarrhea-predominant) | Abdominal pain, frequent loose stools | Mostly loose/watery |
| IBS-C (Constipation-predominant) | Abdominal pain, hard, infrequent stools | Mostly hard/dry |
Possible Causes of IBS-M
The exact cause of IBS-M remains unclear, but research suggests a complex interplay of multiple factors:
- Gut-brain axis dysfunction: Altered communication between the digestive tract and brain can lead to abnormal gut movement and heightened pain sensitivity.
- Changes in gut motility: Muscle contractions in the intestines may speed up or slow down unpredictably, resulting in diarrhea or constipation.
- Visceral hypersensitivity: Increased sensitivity of the nerves in the intestine, causing more pronounced pain and discomfort.
- Altered gut microbiota: Imbalances in the types and quantities of bacteria present in the gut may contribute to IBS symptoms.
- Intestinal infection: Some patients develop IBS after a gastrointestinal infection, known as post-infectious IBS.
- Food sensitivities: Certain foods may trigger or worsen symptoms due to poor digestion or intolerance.
- Genetic factors: Family history may increase susceptibility.
- Psychological stress: Anxiety, depression, and past trauma can be strongly linked to symptom flare-ups.
It is important to note that IBS-M does not cause physical damage to the intestines and is not associated with inflammation or an increased risk of colorectal cancer.
Diagnosing IBS-M
No single test can confirm IBS-M. Diagnosis involves:
- Reviewing your symptoms and medical history
- A physical examination
- Application of the Rome IV criteria: recurrent abdominal pain related to defecation and changes in stool frequency/form, present for at least six months
- Exclusion of ‘alarm’ symptoms such as blood in stool, unexplained weight loss, or family history of inflammatory bowel disease
Doctors may order tests (blood, stool, imaging) to rule out other conditions (celiac disease, inflammatory bowel disease, colon cancer) before confirming a diagnosis of IBS-M.
Key Diagnostic Criteria for IBS-M
- At least 25% of bowel movements are loose/watery
- At least 25% are hard/lumpy, on the same or different days
- Symptoms persist for at least three months, with onset at least six months earlier
How IBS-M Affects Daily Life
IBS-M can substantially disrupt daily activities and social life due to unpredictable bowel habits and abdominal discomfort. Many sufferers report:
- Reduced quality of life, missed work or school
- Social avoidance due to bowel unpredictability
- Impaired concentration and productivity
- Emotional distress (anxiety, depression)
Coping strategies and effective management can help restore quality of life for most people.
Treatment Options for IBS-M
Treatment for IBS-M focuses on alleviating symptoms and improving overall well-being. Because every patient’s triggers and symptom patterns vary, management should be tailored individually.
Dietary and Lifestyle Modifications
- Increase fiber intake – Soluble fiber (from oats, bananas, apples) can help balance bowel habits in some patients
- Try the Low-FODMAP Diet – Limits foods rich in fermentable carbohydrates that may trigger symptoms (such as onions, garlic, beans, wheat products)
- Avoid trigger foods – Common triggers include fatty foods, caffeine, alcohol, and carbonated drinks
- Eat regular, balanced meals
- Stay hydrated
- Exercise regularly – Physical activity can promote healthy bowel function and reduce stress
- Manage stress – Mindfulness, yoga, or counseling may reduce flare-ups
Medications for IBS-M
- Antispasmodics – Reduce abdominal cramping
- Laxatives – For constipation episodes (use cautiously and under medical advice)
- Antidiarrheals – For diarrhea episodes (such as loperamide)
- Probiotics – May help balance gut bacteria
- Antidepressants – Low-dose tricyclic antidepressants or SSRIs can improve pain and relieve coexisting anxiety/depression
Psychological and Behavioral Therapies
- Cognitive behavioral therapy (CBT): Effective for managing stress and reducing bowel symptoms
- Gut-directed hypnotherapy
- Relaxation and coping skills
Prognosis and Outlook
IBS-M is a long-term condition with periods of symptom improvement and recurrence. Most people can successfully control their symptoms with a combination of dietary, medical, and lifestyle interventions. IBS does not shorten life expectancy or lead to serious diseases but can impact well-being and day-to-day comfort.
Frequently Asked Questions (FAQs)
What is the difference between IBS-M and regular IBS?
IBS-M is a subtype of IBS defined by a regular alternation between constipation and diarrhea, while other subtypes are predominated by only one bowel habit.
Is IBS-M dangerous?
No, IBS-M does not cause structural damage to the intestines or increase cancer risk. However, it can significantly impact quality of life if left unmanaged.
Can IBS-M be cured?
There is no cure, but symptoms can often be controlled or minimized. Treatment is focused on symptom management.
Will changing my diet help IBS-M?
Many people notice significant improvement with dietary modifications, especially the low-FODMAP diet and increased fiber. Triggers vary individually, so careful tracking is advised for best results.
Should I see a doctor for IBS-M?
Yes, especially if you experience symptoms for more than three months, or notice blood in stool, weight loss, or other concerning features. Professional diagnosis rules out more serious conditions.
Are medications always necessary for IBS-M?
Not always; many people control their symptoms through lifestyle and diet alone. However, medications are available for those with more severe symptoms or when initial measures are inadequate.
Tips for Living Well with IBS-M
- Keep a detailed food and symptom diary to identify your personal triggers
- Eat smaller, more frequent meals
- Stay active, aiming for regular exercise
- Prioritize sleep and relaxation
- Join a support group or connect online to share coping strategies
- Work with your healthcare team to tailor your management plan
When to Seek Help
Consult your physician promptly if you experience:
- Blood in your stool
- Unintentional weight loss
- Persistent or severe abdominal pain
- Symptoms starting after age 50
- Family history of colon cancer or inflammatory bowel disease
Resources and Support
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)
- International Foundation for Gastrointestinal Disorders
- Local support groups and online forums for IBS
If you suspect you may have IBS-M or are struggling with symptoms, speak with your healthcare provider for personalized advice and support.
References
- https://www.ncbi.nlm.nih.gov/books/NBK534810/
- https://www.niddk.nih.gov/health-information/digestive-diseases/irritable-bowel-syndrome
- https://en.wikipedia.org/wiki/Irritable_bowel_syndrome
- https://www.medicalnewstoday.com/articles/37063
- https://www.healthline.com/nutrition/9-signs-and-symptoms-of-ibs
- https://www.mayoclinic.org/diseases-conditions/irritable-bowel-syndrome/symptoms-causes/syc-20360016
- https://my.clevelandclinic.org/health/diseases/4342-irritable-bowel-syndrome-ibs
- https://www.webmd.com/ibs/digestive-diseases-irritable-bowel-syndrome
- https://www.nhs.uk/conditions/irritable-bowel-syndrome-ibs/
Read full bio of medha deb












