IBS-D: Understanding, Diagnosis, and Effective Treatments
Comprehensive guide to IBS-D, its symptoms, diagnostic process, and the latest evidence-based treatment strategies for improved quality of life.
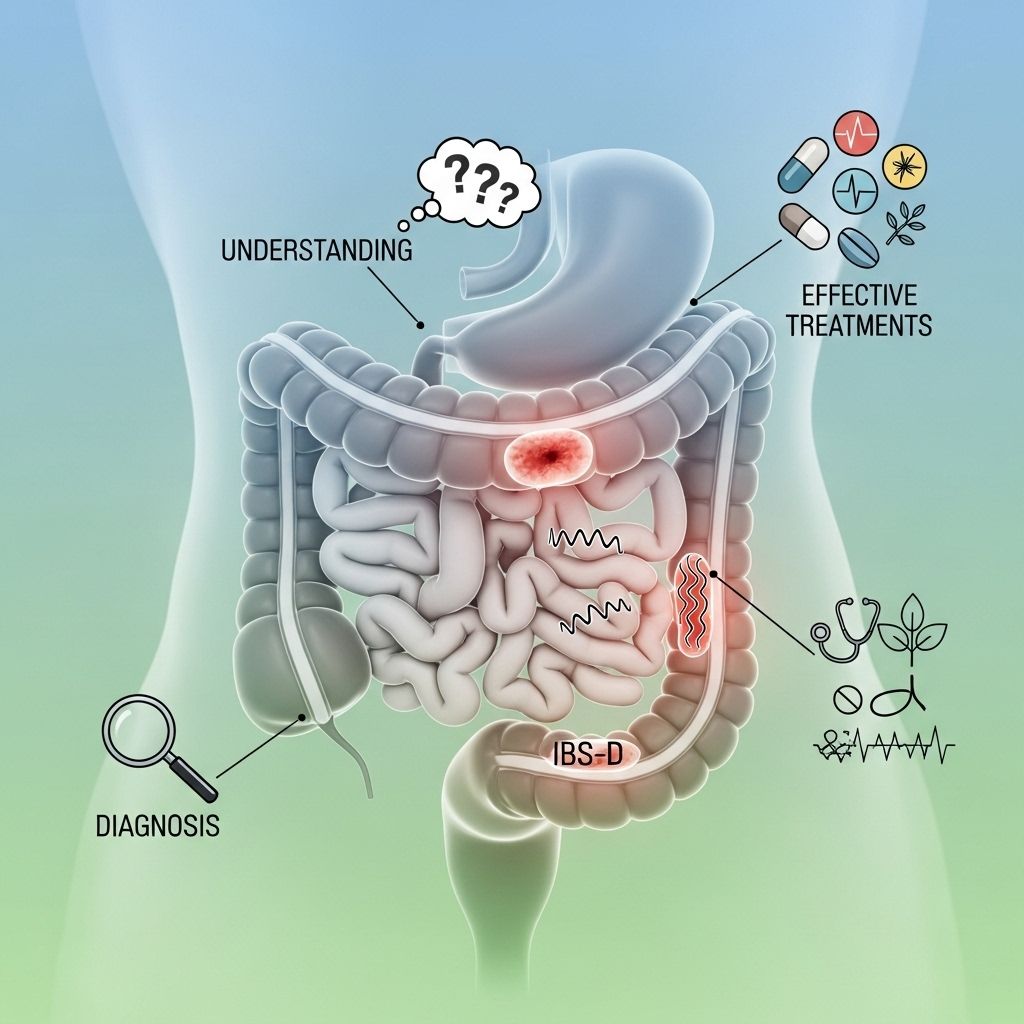
Irritable bowel syndrome with diarrhea (IBS-D) is a common type of IBS marked by frequent, urgent, and loose stools alongside abdominal discomfort. This comprehensive guide explores what IBS-D is, how it’s diagnosed, and the variety of treatment options available to help manage its symptoms effectively.
What Is IBS-D?
Irritable bowel syndrome (IBS) is a chronic gut disorder involving recurrent abdominal pain or discomfort, coupled with changes in bowel habits. There are several subtypes of IBS based on predominant symptoms, including:
- IBS-D: IBS with diarrhea as the primary symptom
- IBS-C: IBS with constipation
- IBS-M: Mixed diarrhea and constipation
- IBS-U: Unclassified
IBS-D can impact daily activities, work, and overall quality of life, making timely recognition and patient-centered management essential.
Symptoms of IBS-D
Symptoms may vary over time and in intensity, but typical features of IBS-D include:
- Frequent, loose, or watery stools
- Sudden, urgent need to have a bowel movement
- Recurrent abdominal pain or cramping, often easing after a bowel movement
- Bloating and excessive gas
- Mucus visible in the stool
- Sensation of incomplete evacuation
Physical harm such as intestinal tissue damage or increased cancer risk is not associated with IBS-D, although the symptoms can be distressing and disruptive.
What Causes IBS-D?
The precise cause of IBS-D remains unclear, but several factors are thought to play a role. These include:
- Gut-brain axis dysregulation: Communication between the gut and nervous system may become abnormal
- Altered gut motility leading to faster transit and loose stools
- Visceral hypersensitivity (increased sensitivity to pain signals from the gut)
- Post-infectious changes (following a bout of gastroenteritis)
- Changes in gut microbiota (the collection of bacteria in the intestines)
- Food intolerances or sensitivities
- Psychosocial stress
- Genetic and environmental influences
Triggers can vary widely among individuals and may include particular foods, stress, hormonal changes, or infections.
How Is IBS-D Diagnosed?
Diagnosing IBS-D largely relies on symptom patterns and the exclusion of other conditions. There isn’t a specific test for IBS-D; rather, the process involves:
- Detailed medical history: Analysis of symptoms, their frequency, duration, relation to bowel movements, and any family history of gastrointestinal diseases.
- Physical examination: Evaluation for abdominal tenderness and other signs.
- Rome IV criteria: Diagnostic criteria requiring recurrent abdominal pain, on average, at least one day per week in the last three months, associated with two or more of the following:
- Relief by defecation
- Change in stool frequency
- Change in stool appearance
To ensure you receive the correct diagnosis and avoid mismanagement, understanding your testing options is key. Read our guide on How Doctors Test and Diagnose Irritable Bowel Syndrome (IBS) to discover essential tests that can lead to an accurate diagnosis. - Exclusion of other causes: Laboratory tests or stool studies to rule out infections, inflammatory bowel disease, celiac disease, and other digestive disorders, especially if there are warning features such as blood in stools, unintentional weight loss, fever, or family history of colon cancer.
In some cases, additional tests like colonoscopies or imaging studies may be warranted if there are red flag symptoms or an atypical disease course.
Alarm Symptoms: When to Seek Immediate Evaluation
It’s important to differentiate IBS from more serious conditions. Certain “alarm” or “red flag” symptoms indicate the need for further evaluation beyond typical IBS workup, including:
- Onset after age 50
- Rectal bleeding or blood in stool
- Unexplained weight loss
- Persistent vomiting
- Anemia (low blood count)
- Nocturnal symptoms waking you from sleep
- Family history of gastrointestinal diseases (such as colon cancer, inflammatory bowel disease)
Such findings may suggest an underlying organic disease, not classic IBS-D.
IBS-D and Quality of Life
Although IBS-D does not cause lasting physical harm, it can have a significant impact on daily life, including social, work, and emotional domains. Many people struggle with unpredictability of symptoms, embarrassment, and stress, which may create a cycle that worsens gut problems.
Comprehensive Treatment Options for IBS-D
Managing IBS-D is highly individualized. Most people benefit from a combination of approaches, tailored to their unique symptoms and triggers. The goals are to alleviate symptoms, restore normal bowel habits, and improve quality of life.
1. Lifestyle and Diet Modifications
- Regular exercise: Physical activity helps regulate bowel function and reduce stress.
- Stress management: Mindfulness, yoga, meditation, and cognitive behavioral therapy (CBT) can be helpful.
- Identifying triggers: Keeping a symptom and food diary may reveal links between symptoms and specific foods or situations.
Dietary Interventions
Several dietary changes may alleviate IBS-D symptoms. Common strategies include:
- Low FODMAP diet: This eliminates certain fermentable carbohydrates found to trigger IBS-D in many people. Gradual reintroduction under a dietitian’s guidance helps identify specific problem foods.
- Limiting caffeine, alcohol, and fatty foods: These can exacerbate diarrhea and abdominal discomfort.
- Avoiding artificial sweeteners (such as sorbitol and mannitol): These can cause diarrhea in sensitive individuals.
- Ensuring adequate hydration: Compensates for fluid lost through diarrhea.
- Considering lactose or gluten avoidance: Only if intolerance or celiac disease is suspected or diagnosed.
2. Pharmacological Treatments
For persistent or severe symptoms, medications may be required. Prescription and over-the-counter options include:
- Antidiarrheal agents (e.g., loperamide): Reduce stool frequency and improve consistency in acute diarrhea, but are less effective for pain and bloating.
- Bile acid binders (e.g., cholestyramine): Useful if excessive bile acids contribute to diarrhea (diagnosed via specific tests or history).
- Antispasmodics (e.g., dicyclomine, hyoscyamine): Help relieve abdominal cramping and discomfort by relaxing gut muscles.
- Antidepressants (low-dose tricyclics, SSRIs): Can help manage pain and gut motility via effects on the gut-brain axis, especially if pain or mood disturbances predominate.
- Prescription drugs for IBS-D:
- Rifaximin: A non-absorbed antibiotic shown to reduce symptoms in some people by altering gut bacteria.
- Eluxadoline: Decreases bowel activity and relieves diarrhea via acting on opioid receptors in the gut (not suitable for those without a gallbladder).
- Alosetron: Approved for severe IBS-D in women unresponsive to standard therapies; use with caution due to rare but serious side effects.
3. Probiotics and Supplements
- Probiotics: Certain strains may help regulate bowel movements and ease IBS-D symptoms, but evidence is mixed and strain-specific.
- Peppermint oil: Available as enteric-coated capsules, peppermint oil may relax gut muscles and reduce pain and bloating for some individuals.
- Soluble fiber supplements: (such as psyllium) can sometimes help those with mixed symptoms or mild diarrhea, but results are variable.
4. Psychological and Behavioral Therapies
Chronic gut disorders are influenced by the gut-brain connection. Behavioral therapies can reduce symptom severity and recurrence, especially for stress-sensitive individuals. Options include:
- Cognitive behavioral therapy (CBT): Addresses negative thought patterns and empowers self-management.
- Gut-directed hypnotherapy: Uses relaxation and imagery techniques to modulate perception of gut symptoms.
- Mindfulness-based stress reduction (MBSR): Enhances awareness and reduces anxiety linked to gut symptoms.
5. Other Interventions and Self-care Tips
- Eat regular, small meals to prevent overloading the gut
- Allow time for relaxed meals; avoid rushing eating
- Review all prescription and over-the-counter medications with your healthcare provider in case any may worsen diarrhea
- Stay as physically active as possible to encourage regular gut motility
Treatment Approaches Table
| Treatment Type | Main Purpose | Notes / Examples |
|---|---|---|
| Lifestyle & Diet | Reduce symptom triggers | Low-FODMAP diet, stress reduction, hydration |
| Medications | Symptom relief | Loperamide, eluxadoline, rifaximin, bile acid binders |
| Probiotics & Supplements | Gut flora balance, pain/cramp reduction | Specific strains, peppermint oil, soluble fiber |
| Behavioral Therapy | Reduce stress, pain sensitivity | CBT, gut-directed hypnotherapy |
Living With IBS-D: Tips for Daily Management
- Maintain a consistent meal schedule
- Carry supplies for symptom flare-ups (e.g., spare clothing, access to restrooms)
- Communicate openly with friends and employers about your condition, as needed
- Seek support through IBS communities, mental health professionals, or peer groups
Frequently Asked Questions (FAQs)
Q: Can I prevent IBS-D?
A: There is no known way to prevent IBS-D entirely, but proactive management of stress, healthy dietary choices, and regular exercise may help reduce flare-ups and symptom severity.
Q: Is IBS-D a lifelong condition?
A: IBS-D is a chronic disorder for most people, with symptoms tending to come and go. With individualized treatment, many people achieve substantial relief.
Q: Does IBS-D cause lasting damage or cancer?
A: IBS-D does not cause visible damage to the digestive tract or increase cancer risk. It is a functional disorder, meaning the gut appears normal on examination, despite distressing symptoms.
Q: Will dietary fiber help with IBS-D?
A: Soluble fiber (like psyllium) may help some individuals, but insoluble fiber can sometimes worsen diarrhea. Working with a dietitian can help tailor fiber intake to your needs.
Q: Should I avoid gluten or dairy with IBS-D?
A: Unless you have diagnosed celiac disease or lactose intolerance, there is no need to strictly avoid these foods. However, some people report fewer symptoms by minimizing them.
Q: When should I see a doctor about IBS-D?
A: Any time you have alarm symptoms (blood in stools, weight loss, persistent pain, or symptoms after age 50), or if your usual IBS-D symptoms change suddenly, seek prompt medical evaluation.
Key Takeaways
- IBS-D is a common, functional gut disorder featuring abdominal pain and frequent diarrhea, negatively impacting quality of life but not associated with severe physical complications.
- Diagnosis relies on symptoms and ruling out other conditions, especially when red flag symptoms are present.
- Treatment is individualized and often includes diet and lifestyle changes, medications, probiotics, and psychological therapies.
- Successful management is possible for most with a patient-centered approach and regular follow-up with healthcare providers.
References
- https://www.niddk.nih.gov/health-information/digestive-diseases/irritable-bowel-syndrome
- https://en.wikipedia.org/wiki/Irritable_bowel_syndrome
- https://www.healthline.com/nutrition/9-signs-and-symptoms-of-ibs
- https://www.mayoclinic.org/diseases-conditions/irritable-bowel-syndrome/symptoms-causes/syc-20360016
- https://my.clevelandclinic.org/health/diseases/4342-irritable-bowel-syndrome-ibs
- https://www.webmd.com/ibs/digestive-diseases-irritable-bowel-syndrome
- https://www.health.harvard.edu/diseases-and-conditions/a-new-diet-to-manage-irritable-bowel-syndrome
- https://medlineplus.gov/ency/article/000246.htm
- https://www.nhs.uk/conditions/irritable-bowel-syndrome-ibs/
Read full bio of medha deb












