IBS-D: Diagnosis and Treatment Options for Irritable Bowel Syndrome with Diarrhea
Comprehensive guide to diagnosing and managing IBS-D, with evidence-based therapies, lifestyle tips, and expert insight on living with irritable bowel syndrome–diarrhea.
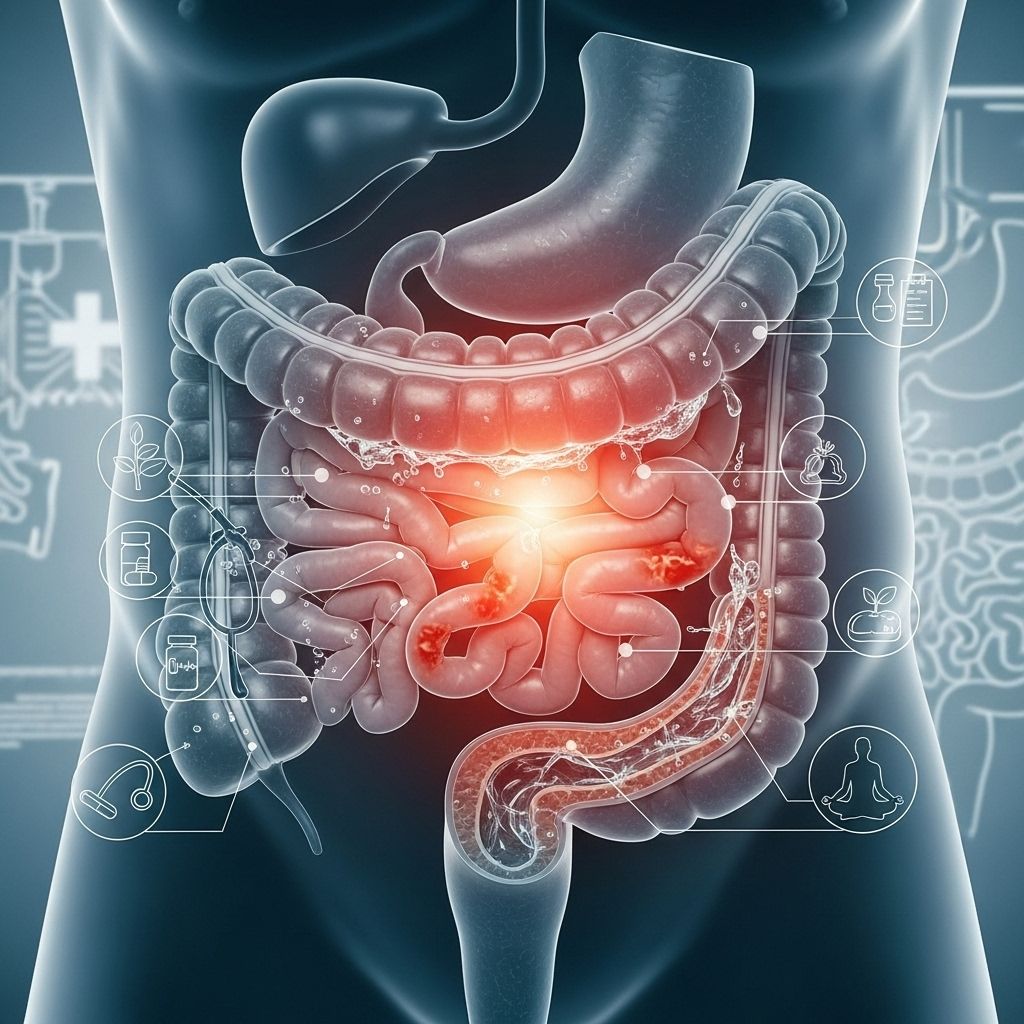
Irritable bowel syndrome with diarrhea (IBS-D) is a common digestive disorder that profoundly affects day-to-day life. Proper diagnosis and an individualized, multi-pronged treatment approach are key to managing symptoms and improving long-term quality of life for those living with this chronic condition.
Overview: What is IBS-D?
IBS-D stands for irritable bowel syndrome with diarrhea as the predominant symptom. IBS is a chronic disorder affecting the gut-brain axis, characterized by recurring abdominal pain and changes in bowel habits. Individuals with IBS-D experience frequent loose stools and urgency, often accompanied by bloating, cramping, and discomfort.
IBS is not caused by structural or biochemical abnormalities and does not show up on standard medical testing. The symptoms are persistent but can fluctuate in intensity. Many people report their symptoms become worse during periods of stress or after eating certain foods.
- IBS-D is one of several IBS subtypes; others include IBS-C (constipation-predominant), IBS-M (mixed), and IBS-U (unclassified).
- The overall prevalence of IBS is around 11% globally, and IBS-D is one of the most common subtypes among adults.
- IBS greatly impacts quality of life, work productivity, and psychological well-being.
Symptoms of IBS-D
IBS-D symptoms mainly involve frequent, urgent, loose, or watery stools, but the condition has many other possible features:
- Recurring abdominal pain or cramping (often relieved by bowel movements)
- Frequent episodes of diarrhea (3 or more loose stools per day)
- Sudden or urgent need to have a bowel movement
- Bloating and excess gas
- A feeling of incomplete evacuation after bowel movements
- Mucus in stool
- Symptoms may vary in severity and can be intermittent
Most people with IBS-D report that symptoms fluctuate in response to factors such as stress, emotional upheaval, certain foods, or illness. Non-digestive symptoms like fatigue, sleep disturbances, and anxiety frequently coexist.
Possible Causes and Risk Factors
The exact cause of IBS-D remains unclear, but several factors are believed to contribute to symptom development:
- Gut-brain axis dysfunction: Abnormal communication between the digestive tract and the central nervous system impacts gut motility and pain perception.
- Visceral hypersensitivity: Increased sensitivity to intestinal stretching or gas, leading to pain and cramping.
- Altered gut microbiota: Imbalances in the intestinal bacteria may play a role.
- Gastrointestinal infections: IBS-D can develop after viral or bacterial gastroenteritis (post-infectious IBS).
- Intestinal inflammation: Low-grade inflammation is observed in some patients.
- Genetics and family history: A family history of IBS or functional GI disorders increases risk.
- Dietary triggers: Certain foods can aggravate symptoms (high FODMAP foods, fatty meals, caffeine).
- Psychological factors: Stress, anxiety, or depression are commonly reported and may worsen symptoms.
Diagnosis of IBS-D
IBS-D is generally diagnosed based on symptoms, thorough medical history, and physical examination. Lab tests and procedures may be ordered to rule out other conditions with similar symptoms, but IBS is a clinical diagnosis—there is no single test to confirm it.
Diagnostic Criteria
- Rome IV Criteria: Recurrent abdominal pain, at least one day per week in the last three months, associated with two or more of the following:
- Related to defecation
- Associated with a change in stool frequency
- Associated with a change in the form/appearance of stool
- Symptom onset at least six months before diagnosis
People with IBS-D have predominant diarrhea, meaning the majority of bowel movements are loose or watery.
Excluding Other Conditions
- Celiac disease (by blood tests)
- Inflammatory bowel disease (IBD), such as Crohn’s disease or ulcerative colitis
- Microscopic colitis
- Bile acid malabsorption
- Colon cancer or polyps (especially in people aged 50+ or with family history)
- Lactose intolerance or food allergies
Red flag or “alarm” symptoms requiring further investigation include:
- Unintentional weight loss
- Rectal bleeding or blood in stool
- New symptoms after age 50
- Family history of IBD or colon cancer
- Severe nocturnal symptoms
Typical investigations that may be used to rule out other causes:
- Blood tests (complete blood count, celiac serology)
- Stool tests (to rule out infection, inflammation)
- Colonoscopy (in older patients or if symptoms are atypical)
Treatment Options for IBS-D
While there is no cure for IBS-D, symptoms can often be controlled through a combination of lifestyle changes, dietary interventions, medications, and psychological support. Treatment is individualized based on the severity, predominant symptoms, and associated conditions.
Lifestyle and Diet Modifications
- Dietary changes: Adjusting what and how you eat can have a profound effect. Approaches may include:
- Adopting a low FODMAP diet (reduces certain fermentable carbohydrates that can trigger symptoms)
- Limiting caffeine, alcohol, spicy or fatty foods
- Eating smaller, more frequent meals
- Identifying and avoiding specific trigger foods through a food diary
- Stress management: Practices such as mindfulness, yoga, meditation, and proper sleep hygiene may alleviate symptom severity.
- Regular exercise: Physical activity may help regulate bowel function and reduce stress.
- Probiotics: Can be beneficial for some individuals, especially specific strains designed for IBS.
Medications for IBS-D
Medications may be recommended if lifestyle and dietary changes are insufficient or symptoms are severe. Treatment is tailored to predominant symptoms.
| Medication Type | Examples | How They Help |
|---|---|---|
| Antidiarrheals | Loperamide (Imodium) | Reduces bowel urgency and frequency by slowing intestinal movement |
| Bile acid binders | Cholestyramine, Colesevelam | Bind bile acids if diarrhea is due to bile acid malabsorption |
| Antispasmodics | Hyoscyamine, Dicyclomine | Reduce abdominal pain by relaxing intestinal muscles |
| 5-HT3 antagonists | Alosetron, Ondansetron | Reduce diarrhea and cramping (Alosetron approved with restrictions for women with severe IBS-D) |
| Eluxadoline | Viberzi | Reduces diarrhea and abdominal pain (avoid if you do not have a gallbladder) |
| Rifaximin | Gut-targeted antibiotic | Short-course used for IBS-D with suspected bacterial overgrowth |
| Tricyclic antidepressants | Amitriptyline, Nortriptyline | Low doses reduce pain, normalize gut motility, and help mood |
All medications should be chosen based on healthcare provider judgment and monitoring for side effects is essential.
Psychological Therapies
- Cognitive behavioral therapy (CBT): Shown to reduce IBS symptoms and improve coping skills by addressing the gut-brain axis.
- Gut-directed hypnotherapy: An evidence-based therapy that involves relaxation and visualization techniques to modulate gut symptoms.
- Other approaches: Stress management training, psychotherapy, and support groups may be helpful.
Complementary and Alternative Approaches
- Acupuncture, peppermint oil capsules, and herbal supplements have shown some promise for select symptoms, but evidence varies and these should only be used with professional advice.
Living with IBS-D
Managing IBS-D is an ongoing process involving more than just medicine. Self-care strategies empower people to control their symptoms and preserve quality of life. Important tips include:
- Keep a symptom and food journal to identify triggers, track progress, and guide treatment adjustments.
- Educate family, friends, and employers about IBS-D for understanding and support.
- Consider working with a registered dietitian experienced in GI disorders for personalized dietary advice.
- Prioritize open communication with your healthcare team to address evolving symptoms and treatment preferences.
It is also normal to feel frustrated or anxious about chronic symptoms. Joining an IBS support group or online community can reduce isolation and help with coping strategies.
Potential Complications and Outlook
IBS-D does not cause permanent damage to the intestines or increase the risk of colon cancer, but the impact on daily functioning and emotional well-being can be profound if left unaddressed. While the disorder is chronic and may fluctuate over a lifetime, many people experience substantial relief with a guided treatment plan and attentive self-care practices. There is no single “cure,” but remission is possible for some, and new therapies are continually emerging.
When to See a Doctor
- If you experience sudden or severe symptoms, unexplained weight loss, blood in stool, persistent pain, or a family history of serious GI diseases, seek medical evaluation promptly.
- Periodic follow-ups are important for optimizing your care and updating your management plan as research evolves.
Frequently Asked Questions (FAQs) about IBS-D
What is the difference between IBS-D and other types of IBS?
IBS-D is characterized predominantly by frequent loose or watery stools, while IBS-C mainly involves constipation and IBS-M swings between diarrhea and constipation. The underlying mechanisms and treatment responses may differ somewhat between types.
Will IBS-D go away permanently?
IBS-D is usually a chronic condition. While long periods of remission are possible, symptoms may recur. Managing triggers and following a comprehensive treatment approach is key to long-term symptom control.
Can diet alone cure IBS-D?
No diet universally cures IBS-D, but dietary management—such as a low FODMAP diet—can significantly reduce symptoms for many.
Is IBS-D dangerous?
IBS-D does not cause cancer or structural intestinal damage, though it can severely affect quality of life. Worrisome signs like blood in stool or unexplained weight loss require investigation for other causes.
Are antidepressants prescribed only for depression in IBS-D?
No. Low-dose tricyclic antidepressants are sometimes used in IBS-D for their effects on pain and gut motility, even in people without depression.
Key Takeaway
IBS-D is a complex and chronic condition that can be managed with a combination of precise diagnosis, individualized treatment, lifestyle modifications, and supportive therapies. With advancements in understanding the gut-brain axis and new treatment options on the horizon, the outlook for people with IBS-D continues to improve.
References
- https://www.ncbi.nlm.nih.gov/books/NBK534810/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5001845/
- https://en.wikipedia.org/wiki/Irritable_bowel_syndrome
- https://www.medicalnewstoday.com/articles/37063
- https://www.healthline.com/nutrition/9-signs-and-symptoms-of-ibs
- https://www.mayoclinic.org/diseases-conditions/irritable-bowel-syndrome/symptoms-causes/syc-20360016
- https://my.clevelandclinic.org/health/diseases/4342-irritable-bowel-syndrome-ibs
- https://www.webmd.com/ibs/digestive-diseases-irritable-bowel-syndrome
- https://www.nhs.uk/conditions/irritable-bowel-syndrome-ibs/
Read full bio of Sneha Tete












