Comprehensive Guide to Hypertrophic Cardiomyopathy Testing
Learn how hypertrophic cardiomyopathy is diagnosed, from medical history and imaging to cutting-edge genetic tests and what you can expect at each step.
Hypertrophic Cardiomyopathy Testing: Procedures, Preparation, and What to Expect
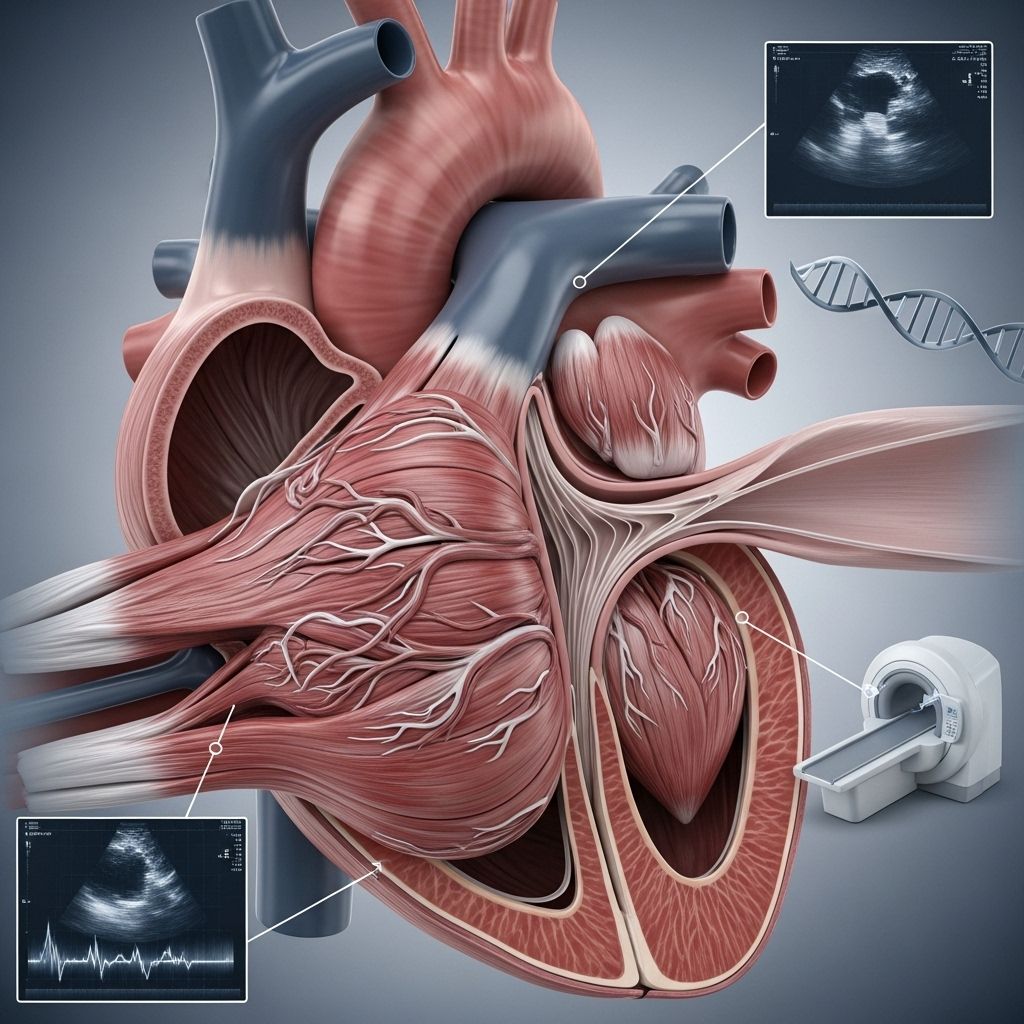
Hypertrophic cardiomyopathy (HCM) is a complex and often hereditary heart condition that affects the heart’s muscle structure, making early and accurate diagnosis essential for effective management and treatment. Testing for HCM involves a combination of medical history reviews, physical exams, imaging studies, genetic testing, and possibly additional specialized assessments. This comprehensive article will guide you through the common tests used to diagnose hypertrophic cardiomyopathy, how to prepare for them, and what to expect throughout the process.
Overview of Hypertrophic Cardiomyopathy
Hypertrophic cardiomyopathy is a disease characterized by the thickening of the heart muscle, particularly the left ventricle. This thickening can impede blood flow, cause abnormal heart rhythms, and increase the risk of complications such as heart failure or sudden cardiac arrest. Because symptoms may be subtle or absent, proactive testing is critical, especially for individuals with a family history of HCM.
Why Testing Is Important
Diagnosing HCM allows individuals to:
- Receive timely treatments to manage symptoms and reduce complications.
- Identify at-risk family members for early intervention.
- Make informed choices about physical activities and lifestyle changes.
- Plan for long-term management and surveillance of the condition.
Who Should Be Tested?
- People who exhibit HCM symptoms, such as chest pain, shortness of breath, fainting, or palpitations.
- Individuals with a family history of HCM or sudden cardiac death.
- Children, adolescents, and athletes with unexplained heart murmurs or abnormal results on a routine electrocardiogram (ECG).
Doctors may recommend genetic testing and routine cardiac screening for first-degree relatives of someone diagnosed with HCM, even in the absence of symptoms.
Preparing for HCM Testing
Preparation depends on the specific tests your healthcare provider suggests. In most cases, you should:
- Share your personal and family medical history, especially any history of HCM, heart disease, or unexplained deaths before age 50.
- Provide a medication list, including supplements and over-the-counter drugs.
- Ask about fasting requirements (some tests like certain blood draws may require fasting).
- Wear comfortable clothing and plan ahead for possible physical activity during some tests, such as exercise stress tests.
- Arrange transportation if your test involves sedation (for example, a transesophageal echocardiogram).
Common Tests Used to Diagnose Hypertrophic Cardiomyopathy
The path to a definitive HCM diagnosis often involves a series of tests. Below, we detail each significant test, its purpose, procedure, and what you can expect before, during, and after the appointment.
Physical Exam and Medical History
- Physical exam includes listening for heart murmurs, which might suggest obstruction of blood flow due to thickened muscle or faulty valves.
- Gathering a detailed three-generation family history helps to assess hereditary risk factors.
Electrocardiogram (ECG or EKG)
An electrocardiogram records the heart’s electrical signals, which trigger muscle contractions. Small electrodes are attached to the chest, arms, and legs.
- Takes about 5–10 minutes and is painless.
- Up to 95% of people with HCM have abnormal ECG findings, such as irregular rhythms or evidence of cardiac thickening.
- Helps determine if additional testing is needed.
Echocardiogram
Transthoracic echocardiogram (TTE) is the primary imaging test for HCM. It uses ultrasound waves to produce images of the heart, showing:
- Thickening of the heart walls, especially the left ventricle.
- Obstruction in blood flow or abnormal movement of valves (notably the mitral valve).
- Pumping ability and chamber sizes.
The test is noninvasive and involves a handheld transducer pressed gently against the chest, typically performed in about 30–60 minutes. It provides real-time, moving images to the interpreting cardiologist.
Exercise Stress Echocardiogram
An exercise (or stress) echocardiogram combines ultrasound imaging with physical activity:
- Images are taken before and immediately after exercise (walking or running on a treadmill).
- Examines how heart muscles and valves respond to exertion.
- Can unmask obstructions or symptoms not present at rest.
- May require fasting or avoiding certain medications before the test, as advised by the doctor.
Transesophageal Echocardiogram (TEE)
A transesophageal echocardiogram involves inserting an ultrasound probe down your esophagus after sedation:
- Provides sharper, more detailed images than a standard transthoracic echocardiogram.
- Especially useful for detecting obstructions or abnormal valve motion.
- May require mild sedation. Arrange to have someone drive you home after the test.
- Takes about 20–30 minutes.
Cardiac Magnetic Resonance Imaging (MRI)
Cardiac MRI uses strong magnets and radio waves to create detailed images of the heart. This noninvasive scan can:
- Show the extent and distribution of heart wall thickening.
- Identify scarring (fibrosis), which is linked to increased risk of arrhythmias or heart failure.
- Use a contrast agent (injected dye) to improve image clarity.
An MRI may last from 30 to 90 minutes. You’ll be asked to remain very still and hold your breath during certain phases. Cardiac MRI is especially valuable when echocardiogram images are unclear or incomplete.
Cardiac Catheterization and Coronary Angiogram
When more information about blood flow or valve function is needed, a cardiac catheterization may be performed:
- A thin, flexible tube (catheter) is inserted into a vein in your arm or groin and guided to the heart using X-ray imaging (fluoroscopy).
- Contrast dye highlights the heart chambers and coronary arteries on live X-ray.
- Measures blood pressure changes, detects blockages, and assesses valve performance.
- Helps differentiate HCM from other causes of chest pain, such as coronary artery disease.
- Procedure typically performed under local anesthesia and sedation. Recovery is quick, but activity may be restricted for a short period afterward.
Genetic Testing for HCM
Since HCM can be inherited, genetic testing plays a vital role in diagnosis and family screening. Key facts:
- Tests for suspected mutations in genes known to cause HCM (most commonly sarcomere protein genes).
- Helps clarify risk for family members, as 30–60% of HCM cases have an identified genetic component.
- Counseling is recommended before and after testing to interpret results.
- Available techniques include next-generation sequencing (NGS), Sanger sequencing, high-resolution melting, and other advanced molecular methods.
- Results may take days to weeks depending on the method used.
| Method | Key Features |
|---|---|
| Sanger Sequencing | Highly accurate, optimal for confirming specific mutations; slow and costly for large-scale testing |
| Next-Generation Sequencing (NGS) | Tests multiple genes rapidly and cost-effectively; ideal for first-line screening |
| High-Resolution Melting | Efficient closed-tube detection of known and unknown variants; usually requires confirmation by another method |
| iPLEX-MassARRAY | Quick, high-throughput analysis but limited to already known mutations |
What Happens After Testing?
Once test results are available:
- Your cardiologist will explain the findings and whether you meet criteria for HCM diagnosis.
- Results may help determine:
- The severity and type of HCM you have.
- Your risk for complications such as arrhythmias or heart failure.
- Which lifestyle changes or treatments are most appropriate (medications, procedures, lifestyle modifications).
- Recommendations for screening or testing close relatives.
Frequently Asked Questions About HCM Testing
What symptoms prompt HCM testing?
Common triggers include unexplained chest pain, fainting, family history of heart conditions, palpitations, shortness of breath, or abnormal heart sounds detected during a physical exam. Sometimes, HCM is discovered incidentally during routine screening or sports physicals.
How long do these tests take?
- ECG, echocardiogram, and most physical exams are completed in under an hour.
- MRI and stress tests may take longer (up to 2 hours for some imaging studies).
- Genetic testing results may take from several days to a few weeks.
Is HCM testing safe?
Most tests (ECG, echocardiogram, MRI) are noninvasive and carry minimal risk. Cardiac catheterization and TEE involve some increased risk related to sedation or blood vessel entry, but serious complications are rare.
Does a normal test rule out HCM?
No. Some people may not show definite changes early in the disease, or imaging may be inconclusive. Ongoing surveillance and repeated testing may be necessary, especially for those with a strong family history or persistent symptoms.
How often should family members be screened?
Screening intervals can vary by age, symptoms, and family history. Often, first-degree relatives are advised to have an echocardiogram and ECG every 1–3 years, but your cardiologist will tailor the schedule to your risk profile.
Key Takeaways and Next Steps
- Timely, accurate testing is crucial for diagnosing HCM and guiding effective management.
- Genetic counseling can help interpret complex test results and assist family members in understanding their own risks.
- If you or a loved one is scheduled for HCM testing, don’t hesitate to ask your care team for more details on preparation and what the results may mean for your health.
Resources for More Information
- American Heart Association: Information on HCM testing and living with heart disease.
- Hypertrophic Cardiomyopathy Association: Support and educational resources for patients and families.
- National Society of Genetic Counselors: Find a certified cardiac genetics expert in your area.
Frequently Asked Questions (FAQs)
Q: What is the gold-standard test for HCM?
A: Transthoracic echocardiogram (TTE) is widely regarded as the primary diagnostic imaging test for HCM, often combined with ECG and, when appropriate, genetic testing.
Q: Will health insurance cover HCM testing?
A: Most diagnostic procedures for HCM are covered if deemed medically necessary, but coverage for genetic testing may vary. Check with your provider and insurer for detailed information.
Q: Can HCM be diagnosed without symptoms?
A: Yes, particularly when family screening prompts testing in people without symptoms or when HCM is detected incidentally during unrelated medical evaluations.
Q: What happens if I test positive for an HCM gene mutation?
A: A positive result helps clarify your risk and typically leads to further cardiac screening and regular follow-up for you and potentially affected family members. Not all mutations cause disease; your medical team will interpret your results in context of your overall health profile.
Q: Are children at risk for HCM?
A: If a parent or sibling has HCM, children may be at increased risk. Pediatricians and pediatric cardiologists can advise on the right time for genetic or cardiac screening of kids and adolescents at risk.
References
- https://nyulangone.org/conditions/hypertrophic-cardiomyopathy/diagnosis
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4199654/
- https://www.aafp.org/pubs/afp/issues/2022/0200/p207.html
- https://my.clevelandclinic.org/health/diseases/17116-hypertrophic-cardiomyopathy
- https://www.heart.org/en/health-topics/cardiomyopathy/understand-your-risk-for-cardiomyopathy/genetic-testing-for-hcm
- https://www.acc.org/Latest-in-Cardiology/ten-points-to-remember/2022/01/24/20/39/Diagnosis-and-Evaluation-of-HCM
- https://www.columbiacardiology.org/patient-care/hypertrophic-cardiomyopathy-center/about-hypertrophic-cardiomyopathy/genetic-testing
- https://www.froedtert.com/hypertrophic-cardiomyopathy/diagnosing-treating
Read full bio of medha deb












