Hypertrophic Cardiomyopathy Life Expectancy: What You Should Know
Understand life expectancy, risks, management, and prognosis for people living with hypertrophic cardiomyopathy.
Hypertrophic Cardiomyopathy Life Expectancy
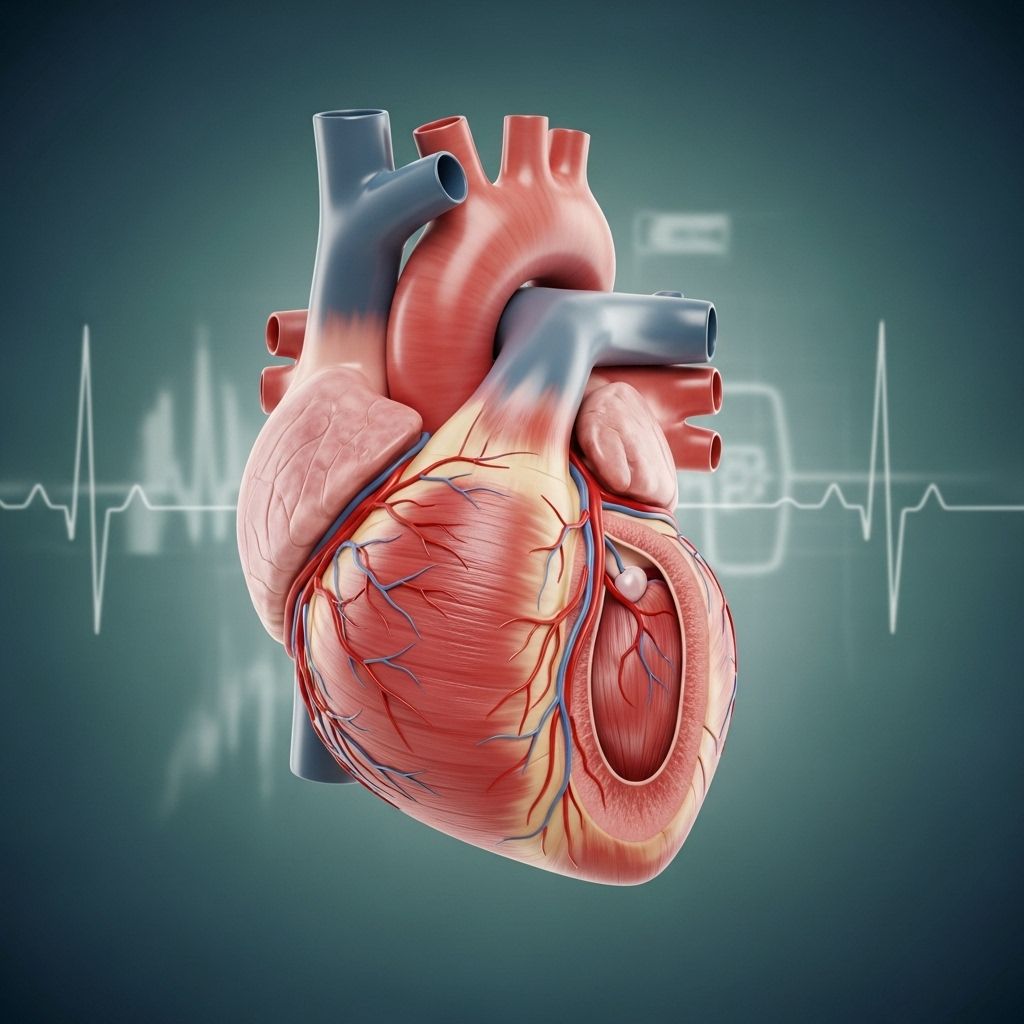
Hypertrophic cardiomyopathy (HCM) is a genetic heart condition that affects the heart muscle, making it abnormally thick. This thickening can make it harder for the heart to pump blood efficiently, and it increases the risk for certain heart-related complications. Advances in understanding, diagnosis, and treatment of HCM have significantly changed what it means to live with this condition. This article reviews life expectancy, risk factors, complications, treatments, long-term outlook, and frequently asked questions regarding HCM.
What Is Hypertrophic Cardiomyopathy?
Hypertrophic cardiomyopathy is characterized by the abnormal thickening (hypertrophy) of the heart muscle, often affecting the septum separating the heart’s left and right chambers. This thickening can obstruct blood flow, disrupt electrical signaling, and put individuals at risk for a range of symptoms or even sudden cardiac events. HCM tends to run in families and is most often caused by inherited genetic mutations.
- Most commonly detected in adolescence or early adulthood, but can develop at any age.
- Symptoms range from none at all to chest pain, shortness of breath, dizziness, or palpitations.
- Some people only discover they have HCM during routine screenings or after a family member is diagnosed or experiences complications.
Life Expectancy for People with Hypertrophic Cardiomyopathy
Many people wonder how long they can expect to live after an HCM diagnosis. While HCM increases the risk of heart-related complications, the vast majority of individuals reach a normal or near-normal life expectancy with appropriate care.
- Studies suggest most people with HCM die from non-HCM-related causes, such as cancer or age-related conditions.
- Regular follow-up and treatment reduce the risk of heart failure, sudden cardiac arrest, and other dangerous complications.
- Having a family history of sudden cardiac death due to HCM underscores the importance of close medical supervision.
HCM Prognosis Over Time
Current research provides a positive outlook, especially for adults diagnosed with HCM:
| Time Since Diagnosis | Cumulative Survival Rate |
|---|---|
| 5 Years | 93.5% |
| 10 Years | 89.5% |
| 15 Years | 83.2% |
| 20 Years | 81% |
The annual HCM-related mortality rate is around 1–1.3%.
Factors Affecting Life Expectancy
- Age of Diagnosis: Diagnoses in adulthood are associated with outcomes comparable to the general population, while childhood diagnoses carry greater risk.
- Presence of Complications: Sudden cardiac death, heart failure, and arrhythmias increase risk.
- Symptoms at Diagnosis: People with more advanced symptoms or evidence of heart dysfunction are at higher risk.
- Genetics and Family History: Family members who experienced HCM-related cardiac events may signal a higher inherited risk.
Understanding Your Risk: Complications of HCM
Living with HCM does increase the risk of certain heart problems. The most notable include:
- Arrhythmias: Abnormal heart rhythms such as atrial fibrillation (AF) or ventricular tachycardia. AF can increase the risk of stroke.
- Heart Failure: Thickened heart muscle can weaken the heart’s pumping ability over time.
- Outflow Tract Obstruction: The thickened septum may block blood leaving the heart, leading to symptoms like fainting or chest pain.
- Sudden Cardiac Arrest: HCM is a leading cause of sudden death in young athletes but remains rare overall.
- Embolic Stroke: Clots that travel to the brain, especially in those with atrial fibrillation.
The good news is that careful management dramatically reduces the impact of these risks for most individuals.
How Hypertrophic Cardiomyopathy Is Treated
Treatment for HCM is highly individualized, focusing on reducing symptoms, preventing complications, and minimizing the risk of sudden cardiac events. Most treatments involve a combination of medication, lifestyle changes, and sometimes invasive procedures.
Medications
- Beta-blockers: Lower blood pressure and slow the heart rate, making the heart more efficient and reducing abnormal rhythms.
- Calcium channel blockers: Help relax the heart muscle and improve blood flow.
- Cardiac myosin inhibitors: Newer medications that target contraction in the heart muscle, improving symptoms and function.
- Diuretics: Used to help manage fluid retention and decrease swelling.
- Antiarrhythmics: For those with irregular heartbeats, these medicines help restore and maintain a normal rhythm.
Procedures and Devices
- Septal Ablation: Injection of alcohol into the arteries supplying the thickened heart muscle to reduce obstruction.
- Septal Myectomy: Surgical removal of part of the thickened muscle obstructing blood flow.
- Implantable Cardioverter-Defibrillator (ICD): Device implanted in the chest to correct life-threatening abnormal heart rhythms and prevent sudden cardiac death.
- Pacemakers: Used in select cases to help coordinate heartbeats and relieve symptoms.
Lifestyle Changes & Monitoring
- Consistent follow-up with a heart specialist (cardiologist)
- Limiting high-intensity competitive sports (on your doctor’s advice)
- Managing other conditions such as high blood pressure, diabetes, or obesity
- Family screening and genetic counseling for relatives, as HCM is often inherited
- Prompt reporting of new or worsening symptoms
Treatment plans are highly personalized. Not all individuals with HCM will need invasive interventions—the majority benefit from lifestyle modification and medications alone.
Long-Term Outlook: Living with Hypertrophic Cardiomyopathy
With regular care and careful observation, most people with HCM live long, fulfilling lives. Many never develop severe symptoms, and only a minority experience major complications if they closely follow their treatment plan.
- Most deaths related to HCM occur at advanced ages: The mean age at an HCM-related death is about 70 years.
- Improved detection, family screening, and ICDs have dramatically reduced sudden cardiac death rates, especially in young people.
- The majority of people with HCM have mild or no symptoms at regular follow-up.
- Prognosis may be less favorable for those diagnosed in childhood or who present with advanced symptoms or severe obstruction.
How Genetics and Family History Play a Role
HCM is usually inherited in an autosomal dominant pattern. This means if a parent has HCM, each child has a 50% chance of inheriting the mutation, though not everyone with the gene develops symptoms.
- Regular screening of first-degree relatives (parents, siblings, children) can detect early changes or disease.
- Genetic counseling helps families understand and manage risk.
When Should You See a Doctor?
If you have a family history of hypertrophic cardiomyopathy, unexplained fainting, chest pain, shortness of breath, or a heart murmur detected at a physical exam, seek evaluation by a cardiologist. Early diagnosis and ongoing monitoring help prevent complications.
- Screen any first-degree relatives of someone diagnosed with HCM, especially before participating in high-intensity sports.
- Report symptoms like fainting, palpitations, or chest pain as soon as they occur.
Frequently Asked Questions (FAQs)
How long can you live with hypertrophic cardiomyopathy?
Most people can expect to live a normal or near-normal lifespan with HCM, especially if they are closely monitored and follow their treatment plan.
What increases the risk of sudden cardiac death in HCM?
Risk factors include a family history of sudden death, prior fainting episodes, very thick heart muscle (greater wall thickness), and certain abnormal rhythms on heart monitoring. An implantable cardioverter-defibrillator may be recommended in higher-risk situations.
Can children with HCM have a normal life expectancy?
Children diagnosed with HCM are at somewhat higher risk for complications and sudden cardiac death compared to adults, but careful management can still provide an excellent outlook.
Is exercise safe for people with HCM?
Exercise is important for overall health, but people with HCM should discuss individualized guidelines with their physician. High-intensity and competitive sports may be discouraged, especially in those with risk factors or a family history of sudden death.
Will I need surgery if I have HCM?
Only a minority of people with HCM require surgical treatment. Many manage well with medications and lifestyle adjustments alone.
Can HCM be cured?
There is no cure for HCM, but treatment can control symptoms and reduce risk of complications. Many people live normal lives with ongoing care.
Is genetic testing recommended?
Genetic counseling and testing are recommended for people with HCM and their close relatives. Results can guide screening and family planning, but not all people with the gene will become symptomatic.
Key Takeaways
- HCM is a lifelong condition, but most affected individuals achieve a normal life expectancy.
- Annual monitoring, early detection, and updated treatments significantly improve outcomes.
- Family members of individuals with HCM should undergo regular screening.
- Notify your doctor immediately about symptoms like chest pain, fainting, or palpitations.
- Advances in HCM research continue to improve the outlook and quality of life for people with this condition.
References
- https://jamanetwork.com/journals/jama/fullarticle/188775
- https://pace-cme.org/news/20-year-prognosis-of-hypertrophic-cardiomyopathy-low-mortality-but-high-morbidity/2456235/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9288772/
- https://www.healthline.com/health/heart/life-expectancy-hypertrophic-cardiomyopathy
- https://www.medicalnewstoday.com/articles/hypertrophic-cardiomyopathy-life-expectancy
- https://www.healthcentral.com/condition/hypertrophic-cardiomyopathy/hypertrophic-cardiomyopathy-life-expectancy
- https://www.heart.org/en/health-topics/cardiomyopathy/what-is-cardiomyopathy-in-adults/hypertrophic-cardiomyopathy
Read full bio of medha deb












