Hyperglycemia vs. Hypoglycemia: Understanding Blood Sugar Extremes
Explore the essential differences, causes, symptoms, and treatments for hyperglycemia and hypoglycemia—including how to recognize and manage both blood sugar emergencies.
Blood sugar, or glucose, is the body’s main source of fuel. For many people, blood glucose remains within a normal range, but for people with diabetes or certain medical conditions, there can be dangerous swings—low blood sugar (hypoglycemia) or high blood sugar (hyperglycemia). Understanding the differences, symptoms, causes, and treatments for each is essential for effective management and long-term health.
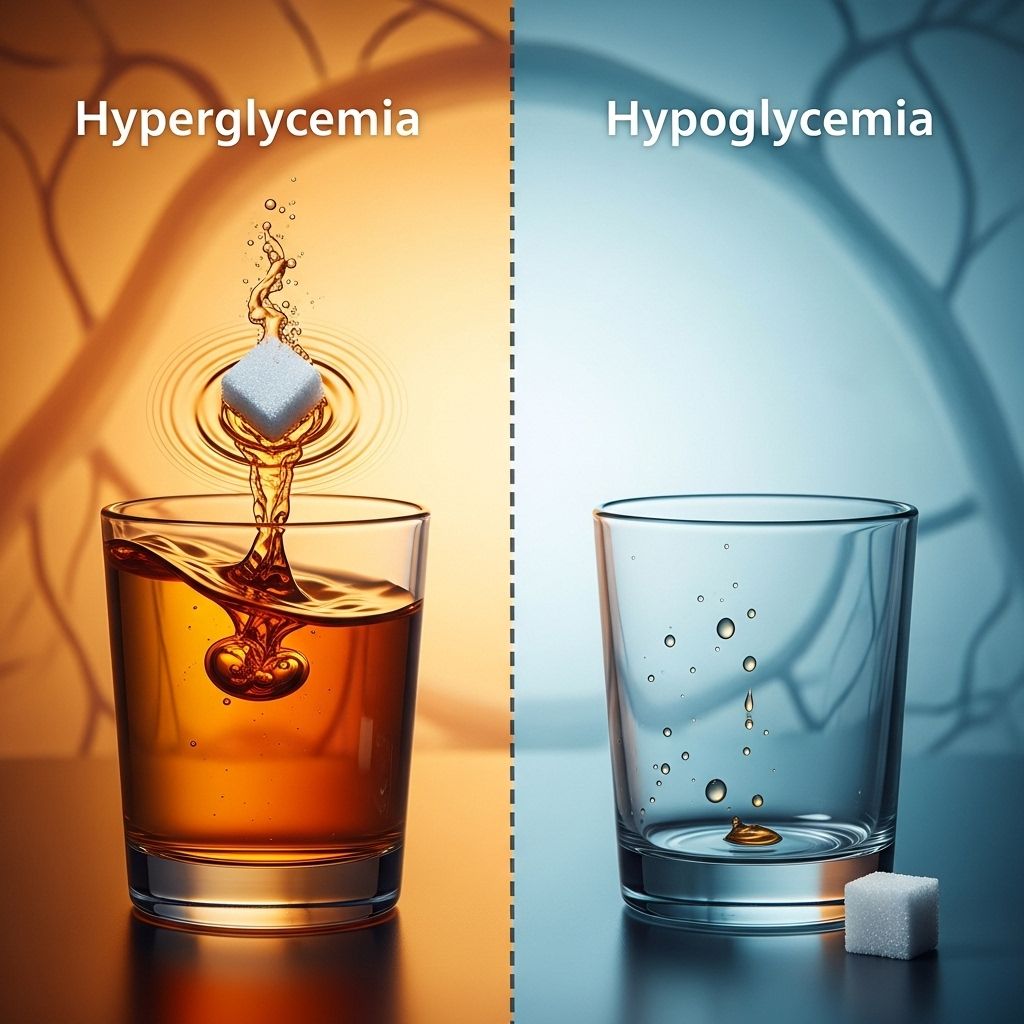
What Is the Difference Between Hyperglycemia and Hypoglycemia?
Hyperglycemia refers to blood sugar levels that are too high, while hypoglycemia refers to blood sugar levels that are too low.
These conditions are essentially opposites but both pose key risks if not addressed promptly.
| Hypoglycemia (Low) | Hyperglycemia (High) | |
|---|---|---|
| Definition | Blood sugar less than 70 mg/dL | Blood sugar over 125 mg/dL fasting or over 180 mg/dL post-meal |
| Common in | People taking insulin or diabetes meds; rarely, those without diabetes | People with diabetes (type 1 and type 2) |
| Key Symptoms | Shakiness, dizziness, sweating, confusion, fast heartbeat | Increased thirst, frequent urination, fatigue, blurred vision |
| Risks | Seizures, loss of consciousness, coma | Serious complications, long-term organ damage |
Understanding Blood Sugar and Insulin
Glucose is the main fuel for the body’s cells. Insulin is a hormone produced by the pancreas that enables glucose to enter cells, where it is used for energy. When this system fails—either from too little insulin, insulin resistance, or over-treatment with insulin—abnormal blood sugar levels can occur.
- Type 1 diabetes: The body produces little or no insulin. People need lifelong insulin therapy.
- Type 2 diabetes: The body doesn’t use insulin effectively (insulin resistance) and may not produce enough.
Normal and Target Blood Sugar Ranges
While blood sugar ranges may differ depending on guideline and health status, the following are commonly accepted targets:
- Non-diabetic adults: 70–140 mg/dL
- People with diabetes: 80–180 mg/dL (varies with individual goals)
- Hypoglycemia threshold: <70 mg/dL
- Hyperglycemia threshold: >180 mg/dL two hours after eating, >125 mg/dL fasting
What Is Hypoglycemia?
Hypoglycemia is a state of low blood sugar, most commonly defined as a blood glucose reading below 70 mg/dL on a glucometer or a continuous glucose monitor (CGM).
Causes of Hypoglycemia
- Too much insulin or diabetes medication
- Skipping or delaying meals
- Excessive exercise without enough food intake
- Alcohol consumption (especially without food)
- Rarely, certain non-diabetes medications or health conditions (such as tumors, malnutrition, or adrenal insufficiency)
Symptoms of Hypoglycemia
- Shakiness or trembling
- Sweating
- Heart palpitations or rapid heartbeat
- Dizziness or light-headedness
- Hunger
- Fatigue or weakness
- Headache
- Confusion or irritability
- Slurred speech
- In severe cases: seizures, fainting, loss of consciousness
Treatment for Hypoglycemia
- Follow the 15-15 rule: Eat 15 grams of fast-acting carbohydrates (such as glucose tablets, juice, or regular soda); wait 15 minutes and recheck blood sugar.
- Repeat as needed until blood sugar returns to 70 mg/dL or higher.
- For severe cases (unconsciousness), emergency glucagon injection may be necessary. Seek medical help immediately if a person cannot swallow or loses consciousness.
What Is Hyperglycemia?
Hyperglycemia describes high blood sugar, often defined as blood glucose levels exceeding 125 mg/dL fasting, or 180 mg/dL two hours after eating for people with diabetes. In non-diabetics, levels this high are unusual and may signal other health issues.
Causes of Hyperglycemia
- Insufficient insulin or diabetes medications
- Consuming excessive carbohydrates or sugary foods
- Lack of physical activity
- Physical or emotional stress
- Illness or infection
- Certain medications (like steroids)
Symptoms of Hyperglycemia
- Increased thirst (polydipsia)
- Frequent urination (polyuria)
- Dry mouth and dehydration
- Fatigue or weakness
- Blurred vision
- Headache
- Nausea or vomiting
- Confusion or difficulty concentrating
- In severe cases: shortness of breath, fruity-smelling breath, or coma
Treatment for Hyperglycemia
- Take extra insulin or prescribed diabetes medication as directed (after checking blood sugar and with guidance from your healthcare provider)
- Increase physical activity
- Hydrate by drinking water
- If symptoms are severe or persist, seek medical attention
- In some cases, hospitalization may be required due to risk of diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemic state (HHS)
Key Differences Between Hypoglycemia and Hyperglycemia
- Origin: Hypoglycemia is often due to excess diabetes treatment or skipping meals, while hyperglycemia usually results from inadequate treatment or other physical stressors.
- Frequency: Both can occur in people with diabetes; hypoglycemia is rare in those without, hyperglycemia can be the first sign of diabetes.
- Symptoms: Hypoglycemia symptoms start suddenly and can escalate quickly; hyperglycemia often develops more slowly with subtler symptoms early on.
- Short-term risk: Hypoglycemia can cause immediate harm (coma, death) if not treated fast; hyperglycemia’s short-term risks lie in severe elevations (“diabetic emergencies” like DKA or HHS).
- Long-term risk: Repeated hyperglycemia causes chronic complications (eye, kidney, nerve, and heart damage); frequent hypoglycemia can blunt the body’s warning signs or increase cardiovascular risks.
Complications Associated with Blood Sugar Extremes
Hypoglycemia Complications
- Seizures and loss of consciousness
- Brain damage after prolonged, untreated hypoglycemia
- Increased risk of injury (e.g., falls, car accidents)
Hyperglycemia Complications
- Short-term: Diabetic ketoacidosis (DKA), hyperosmolar hyperglycemic syndrome (HHS)—both are life-threatening
- Long-term: Nerve damage (neuropathy), kidney failure, retinopathy (eye disease), heart attack, stroke, poor circulation leading to limb amputation
Who Is at Risk?
- People with diabetes: Both hyper- and hypoglycemia can occur due to changes in medication, diet, activity, illness, or stress.
- People without diabetes: Hypoglycemia is rare, but can result from certain medications, critical illnesses, hormonal deficiencies, alcohol abuse, or rare tumors. Hyperglycemia without diabetes is uncommon, but can occur with certain illnesses or as an early sign of developing diabetes.
Diagnosis and Monitoring
Blood sugar monitoring is key for both prevention and management.
- Fingerstick testing (glucometer): Measures capillary blood glucose at home or in clinical settings.
- Continuous glucose monitoring (CGM): Tracks glucose trends throughout the day and night, providing real-time alerts for dangerous highs or lows.
- Laboratory blood tests: Used for formal diagnosis and monitoring (such as fasting plasma glucose, HbA1c for long-term averages).
Prevention Strategies
Preventing Hypoglycemia
- Eat regular meals and snacks
- Take diabetes medications as prescribed and never skip meals if on insulin or sulfonylureas
- Monitor blood sugar more frequently during changes in routine, illness, or after exercise
- Limit alcohol intake and never drink on an empty stomach
Preventing Hyperglycemia
- Follow your diabetes care plan and check blood sugar regularly
- Adhere to medication and insulin regimens
- Moderate carbohydrate intake as needed
- Stay active and maintain a healthy weight
- Manage stress levels
- Address illnesses promptly and follow sick-day rules
When to Seek Medical Attention
- For hypoglycemia: If symptoms do not improve with treatment; if person becomes unconscious, call emergency medical services immediately.
- For hyperglycemia: If blood sugar remains >250 mg/dL for several hours; if symptoms of DKA develop (nausea, vomiting, stomach pain, confusion, fruity breath, rapid breathing); seek urgent care.
Outlook and Living With Diabetes
People living with diabetes can minimize the risk of both hyperglycemia and hypoglycemia through education, consistent monitoring, medication management, and healthy lifestyle choices. Work closely with your healthcare provider to create a personalized plan and gain confidence in responding to symptoms before they become emergencies.
Frequently Asked Questions (FAQs)
Q: Can you have symptoms of high and low blood sugar at the same time?
A: It’s rare but possible for symptoms to overlap, such as fatigue, confusion, or headache, which can be present in both conditions. Monitoring blood sugar is essential to determine the actual problem.
Q: Which is more dangerous, hypoglycemia or hyperglycemia?
A: Both are dangerous. Hypoglycemia can cause life-threatening issues quickly (within minutes or hours), while hyperglycemia usually causes serious complications if sustained over longer periods. Severe, acute hyperglycemia (such as diabetic ketoacidosis) is also life-threatening.
Q: Can someone with diabetes prevent all blood sugar extremes?
A: Not always, but with diligent management—regular testing, appropriate medication, balanced diet, and healthy lifestyle—the frequency and severity of extremes can usually be minimized.
Q: What should you do if you’re not sure whether your symptoms are due to high or low blood sugar?
A: Test your blood sugar immediately if possible; treat according to the reading and symptoms. If in doubt and unable to test, treat for low blood sugar, as it is the more immediate danger, and seek medical advice.
Q: Do hyperglycemia and hypoglycemia affect people without diabetes?
A: Hypoglycemia without diabetes is rare and usually linked to other health conditions or medications. Persistent hyperglycemia in non-diabetics may be an early sign of diabetes or another medical problem and should be evaluated by a doctor.
References
- https://www.drugs.com/medical-answers/difference-between-hypoglycemia-hyperglycemia-3562492/
- https://www.tandemdiabetes.com/support/diabetes-education/managing-diabetes/hypoglycemia-vs-hyperglycemia
- https://www.goodrx.com/conditions/diabetes/hyperglycemia-vs-hypoglycemia-whats-the-difference
- https://diatribe.org/diabetes-management/detecting-signs-hyperglycemia-vs-hypoglycemia
- https://www.healthline.com/health/diabetes/hyperglycemia-vs-hypoglycemia
- https://www.nebraskamed.com/health/conditions-and-services/diabetes/whats-the-difference-between-hyperglycemia-and-hypoglycemia
- https://www.ncbi.nlm.nih.gov/books/NBK279340/
- https://www.youtube.com/watch?v=e55Ql5JTsjs
- https://www.woundcareinc.com/resources/hyperglycemia-vs-hypoglycemia-what-you-need-to-know
Read full bio of Sneha Tete












