Complications of Hyperglycemia: Short-Term and Long-Term Risks
Explore both immediate and chronic complications of high blood sugar, why they occur, and strategies to reduce your health risks.
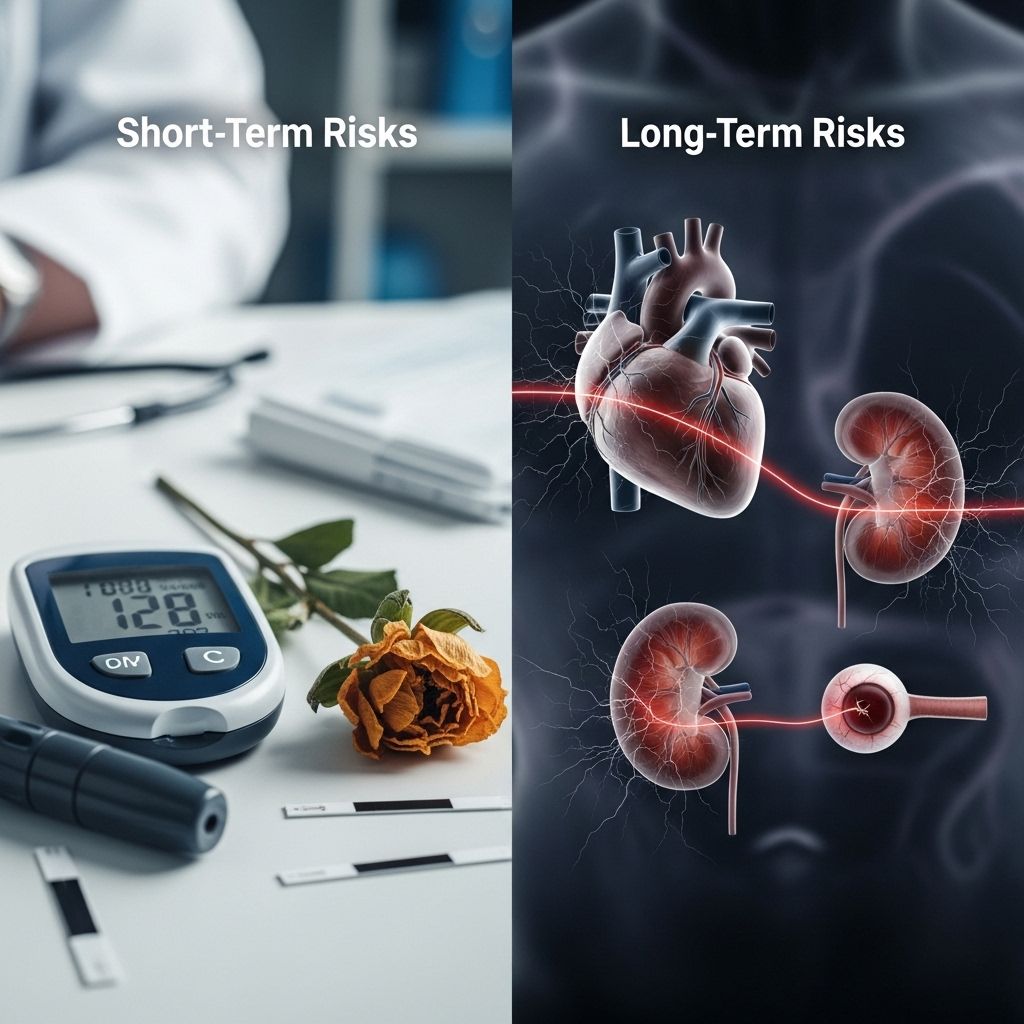
Hyperglycemia, or high blood sugar, is a critical aspect of diabetes that can lead to serious health complications if not managed appropriately. Whether blood sugar levels are slightly elevated or consistently high for long periods, the risk for acute, life-threatening emergencies and chronic, lasting damage to various organs increases. This article examines the immediate complications of hyperglycemia, explores the long-term risks, and highlights steps for prevention and management.
What Is Hyperglycemia?
Hyperglycemia refers to blood glucose levels that exceed the target range. While the exact definition varies depending on individual treatment goals, for most adults with diabetes, blood sugar levels are considered high when they consistently exceed 180 mg/dL (10 mmol/L) after meals, or are elevated above 130 mg/dL (7.2 mmol/L) when fasting. Hyperglycemia often signals issues with insulin production or use, and if persistent, it can damage blood vessels and organs throughout the body.
Immediate (Acute) Complications of Hyperglycemia
Sudden, substantial increases in blood sugar can result in immediate medical emergencies which, if not treated promptly, may become life-threatening. The two most significant acute complications are:
- Diabetic Ketoacidosis (DKA)
- Hyperosmolar Hyperglycemic State (HHS)
Diabetic Ketoacidosis (DKA)
DKA is a dangerous complication that is more common in individuals with type 1 diabetes, though it can occur in those with type 2 diabetes under certain circumstances. It happens when the body does not have enough insulin to allow glucose into the cells, so it starts to break down fat as an alternative energy source. This process leads to an accumulation of acids called ketones in the blood. High ketone levels can make the blood acidic and severely disrupt bodily functions, leading to coma or death if not treated quickly.
DKA can develop slowly, but severe symptoms can appear quickly (within hours):
- Intense thirst and frequent urination
- Extreme fatigue and general weakness
- Nausea, vomiting, and abdominal pain
- Fruity-smelling breath (due to the presence of ketones)
- Rapid, deep breathing
- Flushed or dry skin
- Headache and confusion
- Potential progression to loss of consciousness or coma
DKA requires prompt emergency medical attention and is most frequently triggered by missed insulin doses, infections, or significant physical/emotional stressors.
Hyperosmolar Hyperglycemic State (HHS)
HHS (also called Hyperosmolar Hyperglycemic Syndrome) is a severe complication most commonly seen in older adults with type 2 diabetes. Unlike DKA, HHS does not typically involve significant ketone buildup and blood acidity, but it leads to extremely high blood sugar and severe dehydration. Before HHS develops, an illness or infection often lowers fluid intake, worsening dehydration and concentrating the blood (increasing osmolarity).
Symptoms of HHS develop more gradually and may include:
- Extreme thirst
- Peeing more than usual
- Weakness or lethargy
- Malaise (general feeling of being unwell)
- Dry mouth or skin
- Headache
- Rapid heartbeat
- Low blood pressure when standing (orthostatic hypotension)
- Blurry vision
- Confusion, delirium, or seizures (in advanced cases)
HHS is a life-threatening emergency and demands immediate treatment to gradually reduce blood sugar and correct dehydration.
Table: Acute Complications of Hyperglycemia
| Complication | Population Most Affected | Main Features | Key Differences |
|---|---|---|---|
| Diabetic Ketoacidosis (DKA) | Type 1 Diabetes (also possible in Type 2) | Ketones, Blood Acidity, Nausea, Fruity Breath | High ketones/acidosis |
| Hyperosmolar Hyperglycemic State (HHS) | Type 2 Diabetes (esp. older adults) | Very High Blood Sugar, Severe Dehydration, Confusion | No significant ketones/acidosis |
Long-Term Complications of Hyperglycemia
Chronic, inadequately managed hyperglycemia can silently affect many body systems over years. These long-term complications are largely due to persistent damage to blood vessels, nerves, and other tissues. The risk increases with poor glucose control but can still develop in people with well-managed diabetes over time.
Common Long-Term Complications
- Cardiovascular Disease: Includes high blood pressure, atherosclerosis (narrowing of the arteries), heart attacks, and strokes. High blood sugar damages blood vessels, increases the risk for fatty deposits, and forces the heart to work harder.
- Nerve Damage (Peripheral Neuropathy): Affects up to 50% of people with longstanding diabetes. Tingling, numbness, pain, and loss of sensation usually start in the feet and legs, increasing the risk of wounds, infections, and even amputations.
- Chronic Kidney Disease (Nephropathy): High sugar levels injure delicate vessels in the kidneys. Over time, this can reduce kidney function, cause protein leakage (albuminuria), and even require dialysis or transplant.
- Eye Problems (Retinopathy, Cataracts, Glaucoma): Damage to blood vessels in the retina can cause vision loss and blindness. Diabetic retinopathy is a leading cause of blindness in adults.
- Foot Issues: Poor blood supply and nerve damage increase the risk of slow-healing sores, infections, and ulcers. Without prompt care, this can progress to gangrene and amputation.
- Bone and Joint Disorders: Osteoporosis (bone thinning) and osteoarthritis (joint damage) are more likely in people with uncontrolled diabetes.
- Gum and Tooth Disease: High glucose in saliva feeds bacteria, increasing the risk of gum disease (periodontitis), tooth decay, and tooth loss.
- Weakened Immune System: Leads to more frequent and severe infections, including skin infections, pneumonia, and urinary tract infections.
- Dementia: Recent research has observed that chronic hyperglycemia may increase the risk of dementia, even in milder forms or those without a diagnosis of diabetes.
Table: Chronic Effects of Hyperglycemia
| Organ System / Complication | Potential Effects |
|---|---|
| Heart & Vessels | High blood pressure, atherosclerosis, heart attack, stroke, poor circulation |
| Nerves | Peripheral neuropathy, pain, numbness, loss of sensation, increased injury risk |
| Kidneys | Chronic kidney disease, kidney failure |
| Eyes | Retinopathy, cataracts, vision loss/blindness |
| Feet | Ulcers, infections, amputation |
| Gums & Teeth | Periodontitis, tooth loss |
| Immune System | Increased infection risk |
| Brain | Dementia, cognitive decline |
Why Do Complications Occur?
High blood sugar damages blood vessels in several ways:
- It stiffens vessel walls, making them less able to dilate and more prone to blockages.
- Persistent glucose exposure inflames and injures the lining of vessels.
- Nerve cells and tiny blood vessels are especially vulnerable to metabolic damage.
With time, this damage impairs nutrient and oxygen delivery to tissues, slows healing, and disturbs function at both the whole-organ and microvessel level.
Who Is at Risk?
Anyone living with diabetes (type 1, type 2, or other forms) is at risk of hyperglycemia and its complications. However, the risk increases with:
- Inadequate blood sugar management
- Missed medication or insulin doses
- Periods of illness or infection
- Physical or emotional stress
- Poor diet and lack of physical activity
- Adverse reactions to certain medications (like steroids)
Prevention and Management Strategies
Reducing the risk and severity of hyperglycemia complications involves consistent blood sugar management and healthy habits. The cornerstone strategies include:
- Regular Monitoring: Check your blood glucose as advised to spot rising trends early.
- Take Medications as Prescribed: Adhere strictly to insulin and/or oral medication regimens.
- Balanced Diet: Focus on whole grains, vegetables, healthy fats, and lean protein. Limit high-sugar and highly processed foods.
- Consistent Physical Activity: Regular exercise helps improve insulin use and controls blood sugar levels.
- Manage Stress: Emotional stress can raise blood sugar. Practice relaxation techniques and seek support as needed.
- Promptly Treat Illness/Infection: Being ill or having an infection can cause blood sugar to spike, requiring extra monitoring and, sometimes, medication adjustments.
- Report Persistent High Readings: Notify your healthcare provider if high blood sugar persists despite following your plan.
- Routine Health Screenings: Regular eye exams, foot checks, kidney function tests, and dental visits can detect issues early, when they are easier to treat.
- Wear Medical Identification: People with diabetes should consider a medical ID to inform first responders in emergencies.
Frequently Asked Questions (FAQs)
What blood sugar level is considered an emergency?
Any reading persistently above 240 mg/dL (13.3 mmol/L) can be dangerous, particularly if accompanied by symptoms like nausea, rapid breathing, or confusion. Seek emergency care if you experience symptoms of DKA or HHS.
How quickly can complications from high blood sugar develop?
Acute complications like DKA or HHS can develop in hours (DKA) or days/weeks (HHS) if high blood sugar is untreated. Chronic complications like nerve or kidney damage develop over months to years of poorly managed glucose.
Can I still have complications with good blood sugar control?
While good blood sugar management greatly lowers risk, some individuals still develop complications over the long term. Genetics, age at diagnosis, duration of diabetes, and concurrent illnesses can all influence risk.
Do people without diabetes ever experience hyperglycemia?
Yes, it is possible due to stress, medications (steroids), critical illness, or undiagnosed diabetes. However, chronic hyperglycemia is most often linked to diabetes.
Takeaway
Hyperglycemia poses both immediate and long-term health dangers, but most complications can be prevented or minimized through diligent self-care and collaboration with healthcare providers. Stay vigilant for acute symptoms and prioritize regular follow-up to protect your heart, nerves, kidneys, eyes, and more.
References
- https://www.healthline.com/health/diabetes/hyperglycemia-complications
- https://beyondtype1.org/what-are-the-complications-of-chronic-hyperglycemia/
- https://www.medicalnewstoday.com/articles/323699
- https://www.healthline.com/health/type-2-diabetes/hyperglycemia
- https://www.healthline.com/health/video/top-things-to-know-about-diabetes-complications
- https://my.clevelandclinic.org/health/diseases/7104-diabetes
- https://www.healthline.com/health/video/how-to-lower-blood-sugar-quickly-emergency
- https://www.healthline.com/health/video/blood-sugar-spike
- https://www.medicalnewstoday.com/articles/317462
- https://www.healthline.com/health/video/diabetes-blood-sugar-spikes-levels
Read full bio of medha deb












