Hypercalcemia and Kidney Failure: Causes, Symptoms, and Treatment
Understand the link between hypercalcemia and kidney failure, including causes, symptoms, risks, and recommended management strategies.
Hypercalcemia and Kidney Failure: What You Need to Know
Hypercalcemia refers to an abnormally high level of calcium in the blood. It can significantly affect kidney health, leading to both acute and chronic kidney problems, including renal failure. Understanding the causes, symptoms, complications, and treatments of hypercalcemia is crucial to maintaining kidney function and overall well-being.
Understanding Hypercalcemia
Calcium plays an essential role in many bodily functions, including bone health, nerve transmission, and muscle contraction. The body tightly regulates calcium levels, primarily through the actions of the parathyroid hormone (PTH), vitamin D, and calcitonin. When calcium levels rise above the healthy range, typically above 10.5 mg/dL (milligrams per deciliter), hypercalcemia is diagnosed.
- Mild hypercalcemia: Calcium levels just above the normal range; may not cause symptoms.
- Moderate hypercalcemia: Noticeable symptoms can occur.
- Severe hypercalcemia: Immediate risk to organs such as the kidneys and heart.
The Link Between Hypercalcemia and Kidney Failure
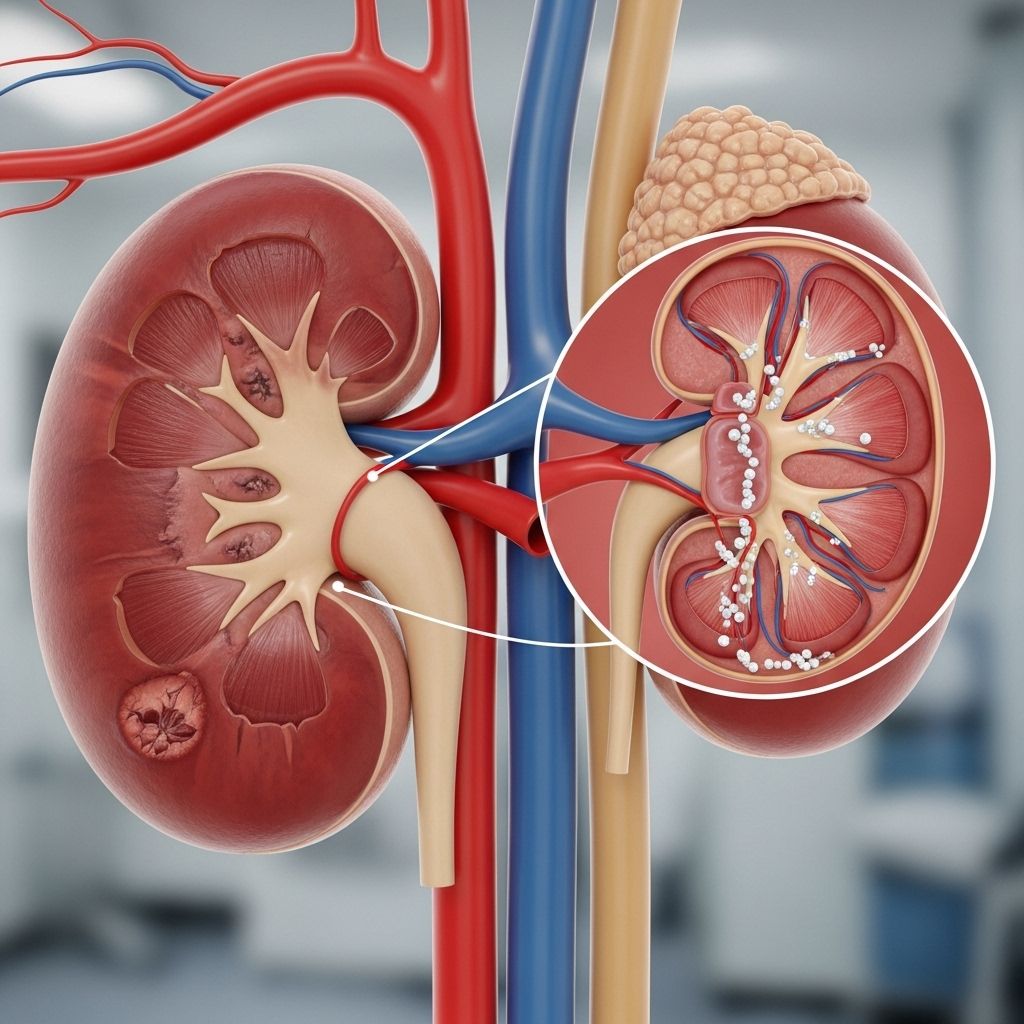
The kidneys are central in filtering excess calcium from the blood. When calcium levels are consistently elevated, the kidneys become overworked, resulting in damage over time. In some cases, hypercalcemia can cause acute kidney injury (AKI) or accelerate underlying chronic kidney disease (CKD). Severe or prolonged hypercalcemia is a risk factor for both forms of kidney failure.
How Does Hypercalcemia Affect the Kidneys?
- Dehydration: High calcium weakens the kidneys’ ability to concentrate urine, causing excessive urination and fluid loss.
- Kidney Stones: Calcium buildup can crystalize, forming stones that block urine flow and injure the kidneys.
- Calcification and Nephrocalcinosis: Calcium deposits can form directly in the kidney tissue, impairing function.
- Reduced Filtration: Hypercalcemia can interfere with the glomerular function, reducing the kidney’s ability to filter blood.
Causes of Hypercalcemia
Hypercalcemia can result from a variety of underlying disorders, medications, dietary habits, and even dehydration. The two most common causes account for about 80-90% of all cases:
- Primary hyperparathyroidism: Overactivity of the parathyroid glands leading to excess PTH secretion and high blood calcium levels.
- Malignancy: Cancers such as breast, lung, kidney, multiple myeloma, leukemia, and lymphoma may release hormone-like substances that raise blood calcium.
Other causes include:
- Excess vitamin D or A (supplements or medications)
- Milk-alkali syndrome: Overconsumption of calcium (via supplements, antacids) and absorbable alkali
- Medications: Thiazide diuretics, lithium
- Sarcoidosis and other granulomatous diseases
- Thyroid disorders (hyperthyroidism, hypothyroidism)
- Dehydration
- Addison’s disease
Symptoms and Warning Signs
Many cases of mild hypercalcemia have no symptoms. However, as blood calcium rises, symptoms can affect multiple organ systems. The classic mnemonic for hypercalcemia is:
- Stones: Kidney stones, frequent urination
- Bones: Bone pain, bone loss
- Abdominal moans: Nausea, vomiting, constipation, abdominal pain, reduced appetite
- Psychic groans: Fatigue, confusion, depression, irritability, forgetfulness
Other possible symptoms include:
- Muscle aches, cramps, twitches, or weakness
- Headaches
- High blood pressure
- Abnormal heart rhythms (shortened QT interval)
- Signs of dehydration: thirst, dry mouth, decreased sweating
When to See a Doctor
If you experience the above symptoms, especially in combination, or have a known risk factor for hypercalcemia, seek medical attention promptly. Early diagnosis can prevent complications, including kidney failure.
How Hypercalcemia Leads to Kidney Failure
The prolonged presence of elevated calcium levels gradually impairs kidney structure and function. Mechanisms include:
- Dehydration: Hypercalcemia causes kidneys to lose their ability to properly concentrate urine, causing frequent dehydration.
- Impairment of Nephron Function: High calcium directly reduces glomerular filtration, leading to a buildup of waste products (elevated creatinine, reduced eGFR).
- Tubular Necrosis: Calcium deposits and direct toxicity can damage tubular cells, further lowering kidney function.
- Calcification of Renal Tissues: Permanent calcium deposits (nephrocalcinosis) decrease functional kidney mass.
Severe or prolonged hypercalcemia, particularly if combined with underlying kidney disease or other comorbidities (like cancer or sarcoidosis), increases the risk of progressing to chronic kidney disease (CKD) or acute kidney injury (AKI). Early and effective treatment of hypercalcemia is essential to reverse or limit kidney damage.
Diagnosis of Hypercalcemia and Kidney Dysfunction
Diagnosis involves a combination of medical history, physical examination, and laboratory tests. Important steps include:
- Measurement of serum calcium: Total and ionized calcium levels
- Kidney function assessment: Blood urea nitrogen (BUN), creatinine, glomerular filtration rate (eGFR)
- Electrolyte panel: Includes sodium, potassium, phosphorus, and bicarbonate
- Urinalysis: Detects calcium oxalate stones, proteinuria, other abnormalities
- Hormone levels: PTH, vitamin D (25-OH and 1,25-dihydroxy), thyroid function tests
- Imaging: Renal ultrasound or CT if stones/obstruction suspected
Identifying the Cause
Further tests may be needed to determine the underlying cause of hypercalcemia, such as cancer workup, parathyroid imaging, or specific screening for granulomatous diseases.
Treatment of Hypercalcemia and Kidney Involvement
Successful treatment depends on the underlying cause, the severity of hypercalcemia, and the degree of kidney dysfunction. The primary goals are to lower blood calcium, protect kidney function, and address the root cause.
Initial Treatments
- Hydration: Intravenous (IV) fluids (usually saline) help dilute blood calcium and correct dehydration.
- Diuretics: After adequate hydration, loop diuretics (e.g., furosemide) help remove excess calcium in urine. Thiazide diuretics are not used, as they raise calcium levels further.
- Monitor heart and kidney function: Continuous monitoring may be necessary in severe cases.
Medications
- Calcitonin: Rapid, short-term reduction of blood calcium, especially in acute severe cases.
- Bisphosphonates: Inhibit bone resorption (breakdown), commonly used for hypercalcemia in cancer.
- Corticosteroids: Reduce high calcium in cases related to granulomatous diseases and vitamin D overload.
- Dialysis: For life-threatening hypercalcemia, especially in patients with advanced kidney failure who cannot tolerate IV fluids.
Treating Underlying Conditions
- Surgical removal of parathyroid adenomas in primary hyperparathyroidism
- Cancer therapy for malignancy-induced hypercalcemia
- Discontinuing causative medications or supplements
Long-Term Management and Prevention
- Regular monitoring of serum calcium and kidney function
- Limiting intake of calcium and vitamin D supplements unless prescribed
- Addressing risk factors (such as dehydration or high doses of antacids)
- Medical management of chronic illnesses that can precipitate hypercalcemia
Outlook and Complications
Timely recognition and treatment of hypercalcemia can often reverse its effects on the kidneys. However, severe or recurring episodes, especially those that go untreated, can lead to permanent kidney damage and increased risk of end-stage renal disease (ESRD).
| Complication | Explanation |
|---|---|
| Dehydration | Impaired urine concentrating ability increases water loss |
| Kidney Stones | Calcium crystals cause obstruction and pain |
| Nephrocalcinosis | Calcium deposits damage kidney tissue |
| Acute Kidney Injury | Sudden kidney failure from calcium overload |
| Chronic Kidney Disease | Progressive loss of kidney function |
Frequently Asked Questions (FAQ)
What is hypercalcemia?
Hypercalcemia is the medical term for abnormally high levels of calcium in the blood, typically defined as calcium above 10.5 mg/dL.
Can hypercalcemia cause kidney failure?
Yes. Extended or severe hypercalcemia can directly damage kidney structures, impair their function, and even trigger kidney failure (both acute and chronic).
What are common symptoms of hypercalcemia?
Many individuals experience fatigue, thirst, frequent urination, abdominal pain, muscle weakness, depression, and sometimes confusion. Severe cases can present with kidney stones or heart arrhythmias.
What are the most frequent causes of hypercalcemia?
The leading causes are overactive parathyroid glands (primary hyperparathyroidism) and certain cancers. Other causes include excessive vitamin D or calcium supplement intake and some medications.
How is hypercalcemia treated if I have kidney problems?
Treatment often includes IV fluids, loop diuretics, and, in severe situations, medications like calcitonin or bisphosphonates. Dialysis is reserved for life-threatening cases or for those with advanced kidney failure who cannot tolerate fluids.
Can kidney damage from hypercalcemia be reversed?
If treated promptly, kidney function can often recover. However, persistent or severe hypercalcemia may cause permanent damage, making early intervention crucial.
Takeaway
Hypercalcemia and kidney failure are interlinked conditions that require prompt evaluation and treatment. Recognizing symptoms early, identifying the underlying cause, and following your physician’s recommendations are key to protecting your kidneys and overall health. Routine follow-up and avoiding unnecessary supplements or medications are important steps in prevention.
References
- https://pubmed.ncbi.nlm.nih.gov/16538974/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4908746/
- https://www.medparkhospital.com/en-US/disease-and-treatment/hypercalcemia
- https://www.aafp.org/pubs/afp/issues/2003/0501/p1959.html
- https://my.clevelandclinic.org/health/diseases/14597-hypercalcemia
- https://www.mayoclinic.org/diseases-conditions/hypercalcemia/symptoms-causes/syc-20355523
- https://www.upmc.com/services/kidney-disease/conditions/hypercalcemia
- https://www.pennmedicine.org/conditions/hypercalcemia
- https://openurologyandnephrologyjournal.com/VOLUME/11/PAGE/22/FULLTEXT/
Read full bio of Sneha Tete












