Humerus Fracture: Symptoms, Treatment, and Recovery
Comprehensive guide to humerus (upper arm) fractures, symptoms, diagnosis, and modern treatment strategies.
Humerus Fracture (Upper Arm Fracture): What You Need to Know
The humerus is the long, strong bone in the upper arm connecting the shoulder to the elbow. A humerus fracture, also known as an upper arm fracture, occurs when this bone breaks due to trauma, falls, or certain medical conditions. Humerus fractures are common injuries among both adults and children, often resulting from falls, direct blows, or medical problems that weaken bone structure. This article provides a comprehensive overview of humerus fractures, including anatomy, causes, risk factors, symptoms, diagnostic strategies, treatment options, and what to expect during the recovery process.
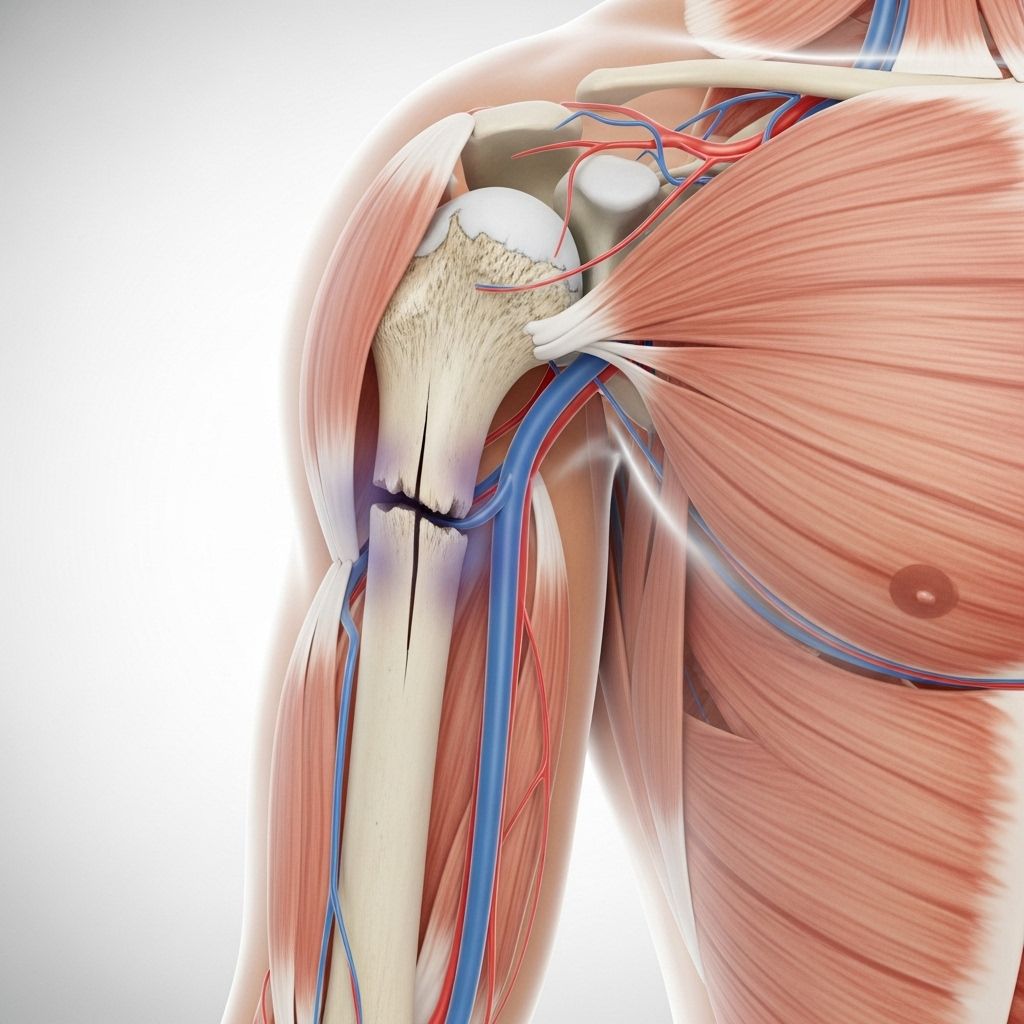
Anatomy of the Humerus
The humerus runs from the shoulder to the elbow, playing a critical role in the movement and function of both the upper arm and forearm. There are three primary regions where fractures can occur:
- Proximal Humerus: Near the shoulder joint.
- Mid-Shaft (Diaphyseal): Along the cylindrical main portion of the bone.
- Distal Humerus: Near the elbow joint.
Each section has unique fracture patterns, clinical presentations, and treatment considerations.
Types of Humerus Fractures
- Proximal Humerus Fractures: Occur at the top of the bone, often associated with shoulder injuries, especially in older adults due to falls.
- Mid-Shaft Humerus Fractures: Involve the central section of the bone. These may result from direct impacts or twisting injuries.
- Distal Humerus Fractures: Located near the elbow, commonly seen in children but occur in adults as well, often from high-impact trauma.
- Open (Compound) Fractures: The bone breaks through the skin, increasing infection risk and urgency for treatment.
- Closed Fractures: The bone does not puncture the skin.
Causes of Humerus Fractures
Humerus fractures most commonly occur as a result of:
- Falls: Particularly common in older adults, falling onto an outstretched hand, shoulder, or elbow can generate enough force to break the humerus.
- Direct trauma: Car accidents, sports injuries, and workplace injuries are frequent causes, especially for diaphyseal and distal humerus fractures.
- Pathologic fractures: Medical conditions such as osteoporosis, tumors, or bone cysts weaken the bone, making it more susceptible to breaking even with mild trauma or regular activities.
Risk Factors
- Osteoporosis: Age-related loss of bone mass is the biggest risk factor, particularly for women post-menopause and older adults.
- High-impact activities: Participation in contact sports, cycling, or high-risk occupations increases trauma risk.
- Chronic conditions: Bone-weakening medical conditions, prior fractures, or long-term steroid use elevate susceptibility.
- Motor vehicle accidents: Young adults and adults in car crashes are at high risk for complex humerus fractures.
Symptoms of a Humerus Fracture
The hallmark symptoms of a humerus fracture can be dramatic and usually include:
- Severe pain at the site of injury, often immediate and persistent.
- Swelling and noticeable bruising around the upper arm or elbow.
- Inability to move the arm or a significant reduction in movement capacity.
- Visible deformity: The arm may appear bent, misaligned, or shorter than normal.
- Crepitus: A grinding or crackling sound may be felt or heard at the site of the break.
- Numbness or tingling: Suggests nerve involvement, especially if the radial or ulnar nerve is affected.
- Open wounds: In cases where the bone pierces the skin (open fracture).
Symptoms may vary based on the fracture location and severity. Children may have difficulty articulating pain but typically refuse to use the affected arm.
Diagnosis
Prompt and accurate diagnosis of a humerus fracture is crucial. Assessment typically involves:
- Physical exam: The doctor examines the arm, assessing for deformity, swelling, wounds, and checking for tenderness along the humerus, pulse in the wrist, and nerve sensation in the hand and fingers.
- Medical history: Questions about the injury’s cause, previous fractures, chronic illnesses, and symptoms experience are common.
- Imaging studies:
- X-rays: Primary tool for confirming the type, location, and severity of the fracture. Multiple views may be needed, including the shoulder, arm, elbow, and sometimes forearm and wrist to rule out additional injuries.
- CT scans: Used when the fracture pattern is complex or not clearly seen on X-ray, especially around the joint or in preparation for surgery.
- MRI scans: Occasionally used to evaluate soft tissue damage (tendons, muscles, ligaments) or nerve involvement if symptoms dictate.
Treatment Options
The method of treatment depends primarily on the type and severity of the fracture, the patient’s age, bone health, and overall functional needs. Treatment is grouped into non-surgical and surgical approaches.
Non-Surgical (Conservative) Treatment
- Immobilization: Applying a sling, splint, or cast to hold the bone in position while it heals. Most non-displaced or minimally displaced fractures heal well with this approach.
- Fracture bracing: For mid-shaft fractures, functional bracing allows limited early motion while still stabilizing the bone.
- Pain management: Medications, ice, and elevation to reduce pain and swelling.
- Physical therapy: Gradual exercises to restore motion, strength, and function once healing allows.
- Regular monitoring: Follow-up X-rays to ensure proper bone alignment and healing.
Surgical Treatment
- Open Reduction and Internal Fixation (ORIF): Metal plates and screws are attached to the bone to stabilize complex, displaced, or open fractures.
- Intramedullary nailing: A metal rod is inserted into the center of the bone to stabilize mid-shaft or long fractures with fewer surgical incisions.
- External fixation: Pins and a stabilizing frame may be used outside the limb in rare or severe cases, like open or contaminated fractures.
- Arthroplasty (joint replacement): In elderly patients or severely shattered fracture patterns, especially near the shoulder, partial or total joint replacement may be needed.
- Tendon and nerve repair: Surgery may correct simultaneous soft tissue or nerve injuries.
Surgical intervention is typically recommended for fractures with significant displacement, joint involvement, multiple fracture lines, or failure to heal using conservative measures.
Complications of Humerus Fractures
- Nerve injury: The radial and ulnar nerves are at risk, especially with mid-shaft and distal fractures. Injury can lead to numbness, tingling, and weakness in the hand and wrist.
- Nonunion: Failure of the bone to heal properly, sometimes necessitating revision surgery or bone grafts.
- Malunion: Healing in an abnormal position, potentially causing deformity or reduced limb function.
- Infection: Primarily with open fractures or after surgical repair.
- Joint stiffness/adhesions: Particularly around the shoulder or elbow if immobilization is prolonged or rehabilitation is inadequate.
- Vascular injury: Rare but serious—damage to blood vessels may compromise blood supply to the limb.
Recovery and Rehabilitation
Healing time varies according to the location and severity of the fracture, patient age, treatment method, and general health. Typical recovery milestones include:
- Bone healing: Most humerus fractures heal in 6–12 weeks, though elderly patients or those with complicated fractures may take longer.
- Physical therapy: Early motion exercises start as soon as safely possible to limit stiffness and muscle atrophy.
- Strengthening: Gradual increase in activity and resistance exercises as bone healing progresses.
- Functional return: Many patients regain most of their pre-injury function, but some—especially after severe or complex injury—may have lingering deficits.
- Follow-up care: Regular medical visits with X-rays to monitor healing and respond to complications promptly.
Summary Table: Humerus Fracture Types and Management
| Fracture Type | Common Cause | Treatment Preferred | Special Considerations |
|---|---|---|---|
| Proximal | Fall, direct impact | Sling/cast, sometimes ORIF | Shoulder function, elderly more affected |
| Mid-Shaft | Direct trauma, twisting | Brace, rarely nail/plate | Radial nerve at risk |
| Distal | High impact, fall on elbow | ORIF common | Elbow joint, nerve/blood vessels nearby |
Preventing Humerus Fractures
- Maintain bone health: Adequate calcium and vitamin D intake, regular weight-bearing exercise.
- Reduce fall risks: Use of mobility aids, home safety modifications for older adults (e.g., handrails, good lighting, removing tripping hazards).
- Treat osteoporosis: Screening and appropriate treatment for bone loss in high-risk populations.
- Use protective equipment: Helmets, pads, and safe sports techniques to limit trauma risk in active individuals and athletes.
When to Seek Medical Help
Immediate medical attention is necessary if you experience:
- Severe pain and obvious deformity in the arm after trauma
- Significant swelling and bruising near the shoulder or elbow
- Numbness, weakness, or loss of movement in the hand or fingers
- Bone protruding through the skin (open fracture)
Frequently Asked Questions (FAQs)
What is the most common site for a humerus fracture?
The proximal humerus (the portion of the bone near the shoulder) is the most frequently fractured segment, especially in older adults who fall.
How long does it take to recover from a humerus (upper arm) fracture?
Bone healing typically takes 6 to 12 weeks, but full function may not return for several months, particularly if surgery or extensive rehabilitation are needed.
When is surgery necessary for a humerus fracture?
Surgery is recommended for fractures that are significantly displaced, involve the joint surface, result in instability, or are associated with nerve, blood vessel, or soft tissue injuries. Failure to heal with non-surgical treatment is also an indication.
Can children and adults recover differently from humerus fractures?
Yes. Children’s bones heal more rapidly, and non-surgical treatment is often successful. Adults and elderly may require longer immobilization or surgery, and recovery can be more challenging due to osteoporosis or comorbidities.
Is it possible to regain full movement after a humerus fracture?
Many patients recover most of their movement and strength, especially with timely and appropriate rehabilitation. However, severe, complex, or inadequately treated fractures can result in residual stiffness or weakness.
Key Takeaways
- Humerus fractures are significant injuries of the upper arm that can occur at the shoulder, shaft, or elbow regions.
- Prompt diagnosis and treatment are crucial to prevent complications and optimize recovery.
- Most simple fractures heal well with immobilization and rehabilitation, while surgical intervention is required for severe, displaced, or open fractures.
- Ongoing physical therapy and follow-up care are the cornerstones of regaining mobility and function.
- Prevention strategies include fall avoidance, treatment of osteoporosis, and use of safety equipment where appropriate.
References
- https://orthoinfo.aaos.org/en/diseases–conditions/distal-humerus-fractures-of-the-elbow/
- https://www.bmc.org/patient-care/conditions-we-treat/db/distal-humerus-fracture-broken-elbow
- https://www.mohitgilotramd.com/mid-shaft-humerus-fracture-shoulder-elbow-surgeon-baltimore-maryland-hardford/
- https://my.clevelandclinic.org/health/diseases/22990-humerus-fracture
- https://education.columbiaorthogroup.com/patient-education-article/humerus-fracture-broken-upper-arm-690/?pesource=5
- https://www.ncbi.nlm.nih.gov/books/NBK482281/
- https://www.orthobullets.com/trauma/1015/proximal-humerus-fractures
- https://www.medstarhealth.org/services/proximal-humerus-fracture-shoulder-fracture
- https://orthozane.com/specialties/trauma/humerus-fracture-upper-arm-fracture/
Read full bio of medha deb












