How Wounds Heal: The Science of Recovery and Repair
Uncover the fascinating biological stages that enable your body to heal wounds and restore tissue after injury.
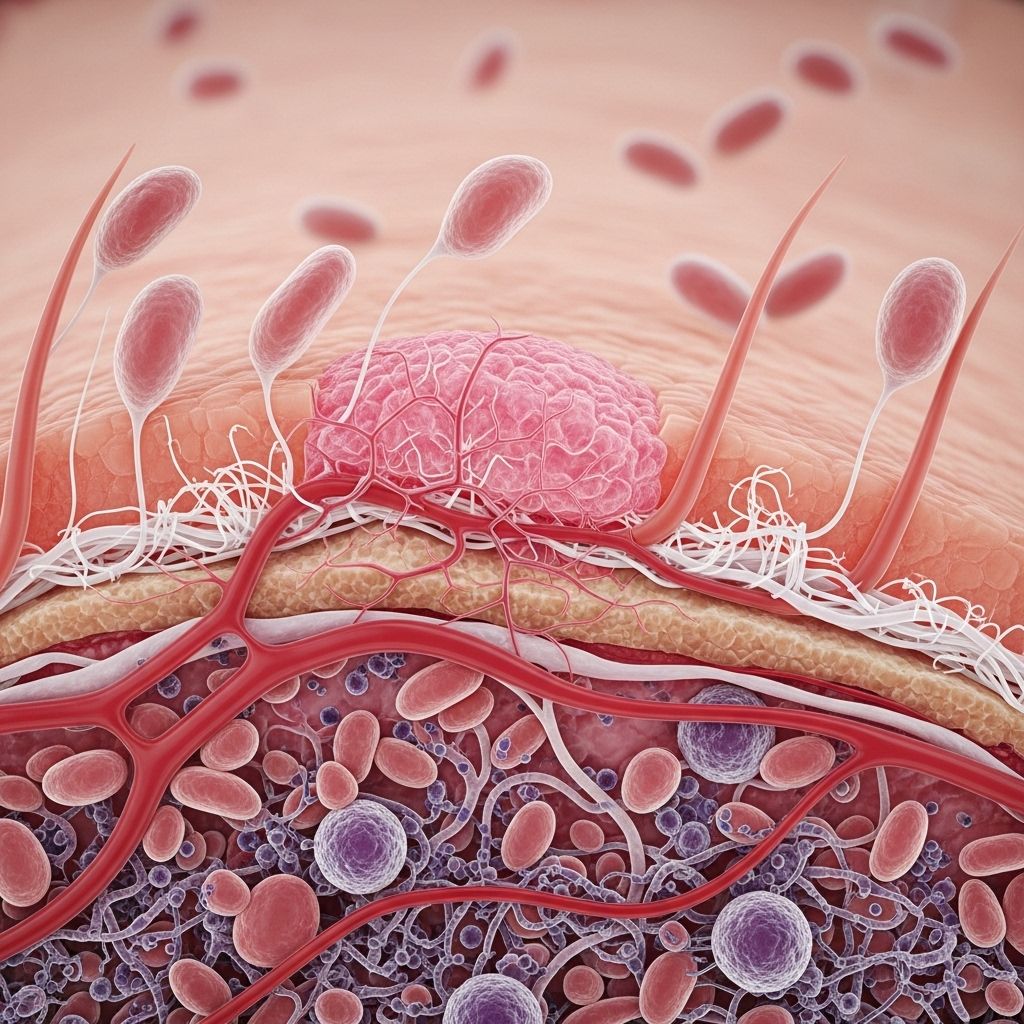
Every day, our bodies are exposed to countless minor injuries—from deeper cuts to superficial scrapes. The ability to repair wounded tissues is fundamental to human survival. Wound healing is a highly coordinated, complex biological process that restores the integrity and function of the skin and other tissues after injury. This article explores the main stages of wound healing, factors that affect healing, and what can go wrong when normal recovery is disrupted.
Understanding Wounds and the Need for Healing
A wound is any break in the body’s tissues, most commonly the skin. Wounds may be caused by trauma, surgery, burns, or underlying health conditions. The fundamental goal of the wound healing process is to restore the tissue’s structure and function by regenerating or repairing damaged cells.
- Acute wounds heal in a predictable time frame through an orderly sequence of events.
- Chronic wounds fail to progress normally and may persist for weeks or months, often due to underlying health issues or repeated trauma.
The Four Stages of Wound Healing
Healing occurs in four primary, overlapping stages. Each phase is vital, involving distinct cellular and chemical activity:
- Hemostasis (clotting)
- Inflammation
- Proliferation (tissue growth)
- Maturation (remodeling)
1. Hemostasis: Stopping the Bleed
Hemostasis is the immediate response to injury. It begins just seconds to minutes after tissue damage:
- Blood vessels around the wound constrict to reduce blood flow.
- Platelets—cells crucial to clotting—aggregate at the site, forming a temporary plug.
- Clotting factors trigger the conversion of fibrinogen to fibrin, a sticky web or mesh that stabilizes the platelet plug and effectively creates a scab.
This initial clot not only stops bleeding but also provides the framework for the successive healing phases.
2. Inflammation: Cleaning and Defending
The inflammatory phase begins soon after hemostasis and can last several days. Contrary to its negative connotation, controlled inflammation is essential to normal healing. Key events include:
- Blood vessels dilate, allowing greater blood flow to the injury. This explains why wounds may appear red, warm, or swollen in the first few days.
- White blood cells, especially neutrophils and macrophages, migrate to the wound to remove bacteria, debris, and dead tissue via phagocytosis.
- Macrophages release growth factors that attract and stimulate other cells needed for later stages of repair.
- A clear or slightly yellow fluid may be present; this is a sign of white blood cell activity.
Although inflammation is critical for defense and cleanup, prolonged inflammation can delay healing.
3. Proliferation: Rebuilding Tissue
The proliferative phase typically starts a few days after injury and can last for several weeks. It centers on rebuilding the damaged area with new tissue and closing the wound. Major activities in this phase include:
- Angiogenesis: New blood vessels form to supply the growing tissue with oxygen and nutrients.
- Fibroblast activity: Fibroblasts secrete collagen, the protein that forms the structural scaffold of new tissue.
- Formation of granulation tissue: A temporary, pink-red, bumpy tissue (due to new capillaries) fills the wound bed.
- Re-epithelialization: Skin cells (keratinocytes) multiply and migrate into the wound from the edges, gradually covering the defect with a new tissue layer.
- Wound contraction: Specialized cells called myofibroblasts pull the wound’s edges together to decrease the area needing healing.
At the end of this phase, you may observe a raised, reddish scar that looks and feels different from the surrounding skin.
4. Maturation: Strengthening and Remodeling
The final phase, maturation or remodeling, can last from several weeks up to two years. Key characteristics include:
- Collagen fibers are continuously realigned and cross-linked, increasing the wound’s tensile strength.
- The pink or red coloration fades as the blood vessels withdraw.
- The rebuilt skin—now a scar—may reach about 80% of the original strength but never fully regains its pre-injury elasticity or appearance.
Itching, puckering, and a stretched sensation are normal as the area continues to remodel.
How Long Does It Take for a Wound to Heal?
Healing times vary widely, depending on:
- The size and depth of the wound (larger or full-thickness wounds take longer).
- Type of wound (surgical vs. accidental; closed vs. open).
- The individual’s overall health, age, and underlying conditions (such as diabetes or vascular disease).
- Wound care practices—keeping wounds clean and covered generally speeds recovery.
| Wound Type | Typical Healing Time |
|---|---|
| Minor cuts and scrapes | 7–10 days |
| Surgical incisions | 6–8 weeks |
| Deep/larger wounds | Weeks to months |
| Chronic wounds | Several months—or longer if untreated |
Most wounds will form new tissue and close in about three months, but it can take up to two years for complete remodeling.
Factors That Affect the Wound Healing Process
Not all wounds heal at the same rate. Several factors can hasten or hinder the process:
- Infection: Bacterial contamination delays or halts healing and can lead to abscesses or cellulitis.
- Poor circulation: Insufficient blood supply, often due to vascular disease, diabetes, or smoking, impairs delivery of oxygen and nutrients.
- Underlying health conditions: Conditions like diabetes, immune deficiencies, and obesity can impair cell function and tissue repair.
- Medications: Some drugs (such as corticosteroids, chemotherapy agents, or certain anti-inflammatory agents) slow the repair process.
- Nutrition: Deficiencies in protein, vitamins (C, A, E), or zinc can impair collagen synthesis and immune defense.
- Age: The elderly typically heal more slowly due to thinner skin and underlying health issues.
- Repeated trauma or pressure: Persistent physical stress on the wound bed impedes healing (e.g., bedsores).
- Improper wound care: Not keeping the wound moist, clean, and protected can delay repair.
Why Do Some Wounds Refuse to Heal?
Chronic or non-healing wounds are a significant health issue, especially among older adults and people with underlying diseases. The most common chronic wound types include diabetic ulcers, venous ulcers, and pressure ulcers.
Reasons for poor healing may include:
- Prolonged infection or biofilm formation (bacterial colonies resisting antibiotics)
- Poor blood flow (ischemia)
- Repetitive trauma, pressure, or friction
- Impaired immune response or cell function
- Undiagnosed underlying disease such as diabetes
Non-healing wounds often require assessment and management by specialists, and may need advanced therapies, such as debridement (removal of dead tissue), negative-pressure wound therapy, or even surgical intervention.
Principles of Good Wound Care
Proper care can drastically improve healing rates and outcomes. General guidelines include:
- Cleanse the wound gently with sterile saline or an appropriate wound cleanser to remove debris and bacteria.
- Debridement: Removal of dead, damaged, or infected tissue is often needed to aid recovery.
- Moist wound environment: Keeping wounds moist (not wet) promotes the migration of cells and slows down tissue dehydration and cell death.
- Protect: Use appropriate dressings to shield the wound from further trauma, dirt, and bacteria.
- Off-load pressure: For wounds on the feet or pressure points, minimizing mechanical stress is vital.
- Monitor: Watch for signs of infection—such as increased redness, swelling, drainage, worsening pain, or fever—and seek prompt medical evaluation.
- Optimize general health: Address underlying health issues, maintain a balanced diet, and quit smoking to enhance healing capacity.
Scarring: The End Result of Wound Healing
Even after a wound appears healed, a visible scar remains—a section of skin with altered color, texture, and elasticity. Scars result when the deeper, supportive layers of skin (the dermis) are injured and replaced with fibrous collagen.
- Most scars gradually fade and flatten over time—but seldom disappear entirely.
- Excessive scarring (hypertrophic or keloid scars) can occur in some individuals, especially on certain body parts or with genetic predisposition.
- Gentle massage, sun protection, silicone sheets, or prescribed topical treatments may help improve scar appearance.
When to Seek Medical Attention
- Wounds that are deep, bleeding heavily, or expose muscle, bone, or tendon.
- Visible signs of infection—spreading redness, swelling, warmth, pus, fever.
- Wounds that do not close or show improvement after 2–3 weeks of care.
- Potential foreign objects within the wound.
- Signs of poor circulation, numbness, or chronic diseases interfering with healing.
Frequently Asked Questions (FAQs)
Q: What are the signs that a wound is healing normally?
A: Common signs of healthy healing include reduced pain and swelling, formation of new tissue or scab, absence of significant redness or pus, and the closure of the wound over time.
Q: How can I speed up the healing of a minor wound?
A: Keep the wound clean and covered, avoid picking scabs, maintain a healthy diet, and avoid smoking. If symptoms worsen, seek medical advice.
Q: Why do some wounds develop thick or raised scars?
A: Some people are genetically prone to producing excess collagen during healing, resulting in hypertrophic or keloid scars. Tension, repeated trauma, and location on the body also influence scar formation.
Q: When should a wound be closed with stitches or medical glue?
A: Deep, long, or gaping wounds, especially on the face, joints, or hands, often require closure by a healthcare professional to encourage fast healing and reduce scarring.
Q: What is the role of nutrition in wound healing?
A: Adequate protein, healthy fats, vitamins (especially C and A), and minerals like zinc are needed to support cell growth, collagen production, and immune function during repair.
Key Takeaways
- Wound healing is a multi-phase process involving hemostasis, inflammation, tissue proliferation, and remodeling.
- Most minor wounds heal in 1–2 weeks; major wounds require longer, and full-strength recovery can take months.
- Poor nutrition, infection, or underlying health issues can prolong healing.
- Proper care—cleaning, covering, and protecting—optimizes outcomes and minimizes scarring.
- Consult a healthcare professional for persistent, worsening, or complex wounds.
References
- https://www.healthline.com/health/skin/stages-of-wound-healing
- https://en.wikipedia.org/wiki/Wound_healing
- https://www.ncbi.nlm.nih.gov/books/NBK470443/
- https://www.hopkinsguides.com/hopkins/view/Johns_Hopkins_Diabetes_Guide/547150/all/Wound_Healing
- https://www.youtube.com/watch?v=I0gilO6Lah0
- https://pubmed.ncbi.nlm.nih.gov/29262065/
Read full bio of Sneha Tete












