How Many Heart Stents Can You Have? Insights, Safety, and Recovery
Discover how many heart stents a person can receive, when they're recommended, and factors affecting treatment choices.
How Many Heart Stents Can You Have?
Heart stents are a critical tool in treating coronary artery disease and restoring blood flow to the heart. But many people wonder: how many stents can be placed in the heart, and what factors play into this decision? This comprehensive guide explores what heart stents are, how they work, what determines the number you might need, and important considerations for safety and recovery.
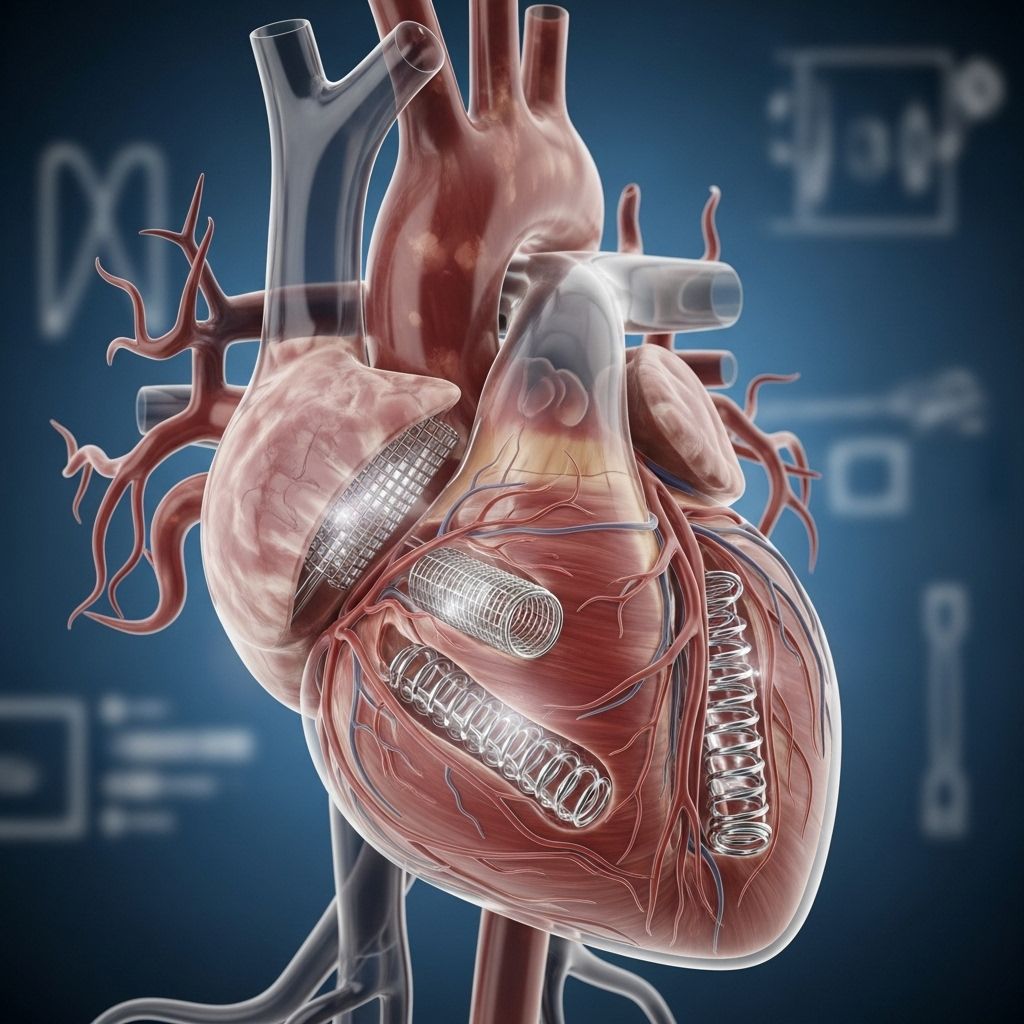
What Is a Heart Stent?
A heart stent is a tiny mesh tube, typically made of metal or sometimes coated with medication, inserted into narrowed or blocked coronary arteries during a procedure called angioplasty. Its primary role is to prop open the artery, ensuring adequate blood flow to the heart muscle. Over time, the body’s tissue can grow around or into the stent, further stabilizing its position and integrating it with the artery wall.
- Stents are used to treat coronary artery disease (CAD), a condition where plaque buildup narrows arteries.
- The stent helps prevent re-narrowing (restenosis) of the artery after angioplasty.
- Most modern stents are drug-eluting, releasing medication to reduce the risk of restenosis.
Why Are Heart Stents Used?
Heart stents are recommended under specific conditions, typically when arteries are so narrowed or blocked that blood flow is significantly restricted, which may lead to chest pain (angina) or even a heart attack. Stents can:
- Open up blocked arteries and improve blood flow immediately after a heart attack.
- Alleviate symptoms such as chest pain and shortness of breath.
- Serve as an alternative to more invasive surgery, like coronary artery bypass grafting (CABG), especially when fewer arteries are involved.
However, stents are not always the first-line treatment. If symptoms of angina can be managed effectively with medication, angioplasty and stent placement may not be necessary. Current evidence suggests stents are primarily used to relieve symptoms rather than prolong survival in stable coronary artery disease.
How Many Stents Can Be Put in the Heart?
There is no fixed upper limit to the number of heart stents a person can receive. Instead, the decision is based on multiple medical considerations, including:
- The number of arteries affected and the extent of blockages.
- Location and length of the narrowed segments.
- Overall health of the patient and comorbidities, such as diabetes or chronic kidney disease.
- Prior procedures and the presence of existing stents.
- The degree of improvement expected from additional stenting versus alternative treatments, like bypass surgery.
Some patients may have one stent, while others may require several over the course of their lifetimes, either in a single procedure or across multiple procedures as new blockages form.
Multiple Stents: Is There a Limit?
- It is not uncommon for some people to have three or more stents placed over time, especially if coronary artery disease is diffuse or progressively worsens with age.
- Some individuals may have as many as six or more stents — the maximum number depends on the individual’s specific anatomy and risk profile.
- In general, if blockages exist in several major arteries, coronary artery bypass grafting (CABG) may be recommended instead of multiple stents.
When Do You Need Multiple Heart Stents?
Multiple stents may be needed:
- If there are blockages in more than one coronary artery.
- When a long segment or multiple segments of a single artery are narrowed and each requires its own stent.
- Over time, as new blockages form in other parts of the coronary arteries, necessitating additional procedures and stent placements.
- If a stent restenoses (re-narrows), a new stent may be inserted to re-establish good blood flow.
Key Factors Considered by Doctors
- Overall patient health and ability to tolerate another procedure.
- Risks of further stenting versus benefits for symptom management or preventing major cardiac events.
- Presence of conditions (such as diffuse multi-vessel disease) that may make bypass surgery preferable.
- Potential for overlapping stents, which can increase complication risks.
Stents vs. Bypass Surgery
When blockages are extensive or present in multiple major vessels, doctors may recommend bypass surgery over the placement of several stents. Some general guidelines:
- Stenting is common for one or two blocked arteries.
- If you have three or more arteries with severe blockages, bypass surgery could be a better long-term solution, as it can treat more diffuse disease.
- Bypass surgery is more invasive and has a longer recovery period, but may be more effective for people with complex or diffuse coronary artery disease.
The best approach is tailored to individual circumstances, weighing factors such as symptom severity, overall risk, and the extent of disease.
What Are the Benefits of Heart Stents?
- Immediate symptom relief: Most patients experience rapid improvement in symptoms such as chest pain and breathing difficulties.
- Reduced need for open-heart surgery: Stenting is less invasive than bypass, requiring only a small incision for catheter insertion, and recovery time is much shorter.
- Can be lifesaving: Especially when performed during or soon after a heart attack to quickly restore coronary blood flow.
- Short hospital stay: Most people return home within a few days after a stenting procedure.
What Are the Risks and Complications of Stents?
While placing a stent is generally safe, there are some risks and potential complications associated with the procedure and device.
- Allergic reactions to contrast dye or materials used in the stent.
- Bleeding at the catheter insertion site.
- Blood clot formation within the stent, raising the risk of a heart attack, particularly if antiplatelet medications are not taken as prescribed.
- Scar tissue growth (restenosis): Excessive tissue buildup at the site of the stent can cause the artery to narrow again, though drug-eluting stents have reduced this risk.
- Damage to the artery or, rarely, other complications such as heart attack, stroke, or kidney problems from the dye.
Long-term outcomes are generally improved by following prescribed medications and attending regular follow-up appointments.
How Is a Heart Stent Placed?
The process of stent placement is called percutaneous coronary intervention (PCI) or angioplasty with stenting. It follows these basic steps:
- A small incision is made in the groin, wrist, or arm to access an artery.
- A thin tube (catheter) is guided through blood vessels to the site of the blockage using x-ray guidance and dye for visibility.
- A small balloon at the tip of the catheter is inflated to widen the artery; a stent mounted on the balloon is expanded into place.
- The balloon is deflated and withdrawn, leaving the stent to support the opened artery.
Most procedures use a local anesthetic, and patients are typically awake but sedated.
What Happens After Getting a Stent?
Post-procedure care is crucial for the success of stent placement and includes:
- Medications: You’ll need to take medications (e.g., aspirin and other antiplatelet agents) to prevent blood clots from forming inside the stent, usually for at least 6–12 months.
- Lifestyle changes: To reduce the risk of future blockages, you should stop smoking, eat a heart-healthy diet, maintain a healthy weight, control blood pressure, and get regular physical activity.
- Routine follow-up: Regular checkups allow your cardiologist to monitor stent function and general heart health.
Alternative Treatments to Stenting
- Medication: For some patients, especially with less severe symptoms or stable angina, doctors may recommend medications to control chest pain and reduce cardiac risk.
- Coronary artery bypass surgery: Typically considered when multiple arteries are blocked or when blockages are hard to access with stents.
- Lifestyle modification: Can slow or even reverse the progression of coronary artery disease and is recommended alongside other treatments.
Frequently Asked Questions (FAQs)
Is there a maximum number of stents a person can have?
There is no strict maximum, but practical and safety considerations often guide doctors to recommend alternatives such as surgery when extensive disease is present. Each case is unique, and decisions are made individually.
Can all patients with heart disease get stents?
No. Stents are best suited for certain kinds of blockages, usually significant narrowings in larger coronary arteries. Some patients with complex, diffuse disease benefit more from surgical bypass or medication management.
Does having more stents increase my risk?
The risk of complications, such as blood clots or restenosis, may modestly increase with more stents or overlapping stents. Careful planning and use of antiplatelet therapy help minimize these risks. Following your doctor’s medication instructions is essential.
Will stents cure coronary artery disease?
Stents treat the symptoms by opening blocked arteries, but they do not cure the underlying disease process. Continued lifestyle changes and medications are needed to manage coronary artery disease long term.
How long do stents last?
Stents are designed to be permanent, but they can sometimes develop complications such as restenosis or blood clots. With appropriate care and medication, most stents function well for many years.
Takeaway
Heart stents are a valuable treatment for coronary artery blockages. The number a person can receive is determined by their overall heart health, the nature of their disease, and the balance of risks and benefits. While some may require multiple stents over time, others might be better suited to alternative therapies. Always discuss your specific circumstances with your cardiologist to determine the best approach for you.
References
- https://www.healthline.com/health/heart-disease/stent
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8507088/
- https://www.health.harvard.edu/heart-health/does-a-coronary-stent-make-sense-for-stable-angina
- https://www.nhlbi.nih.gov/health/stents
- https://www.ahajournals.org/doi/10.1161/circinterventions.110.960872
- https://www.heart.org/en/health-topics/heart-attack/treatment-of-a-heart-attack/stent
- https://medlineplus.gov/ency/article/007473.htm
- https://med.stanford.edu/news/all-news/2019/11/invasive-heart-treatments-not-always-needed.html
Read full bio of medha deb












