How Long Do Stents Last? Lifespan, Effectiveness, and What to Expect
Discover the expected lifespan of stents, factors influencing their durability, and how to maximize your heart health after stent placement.
How Long Do Stents Last?
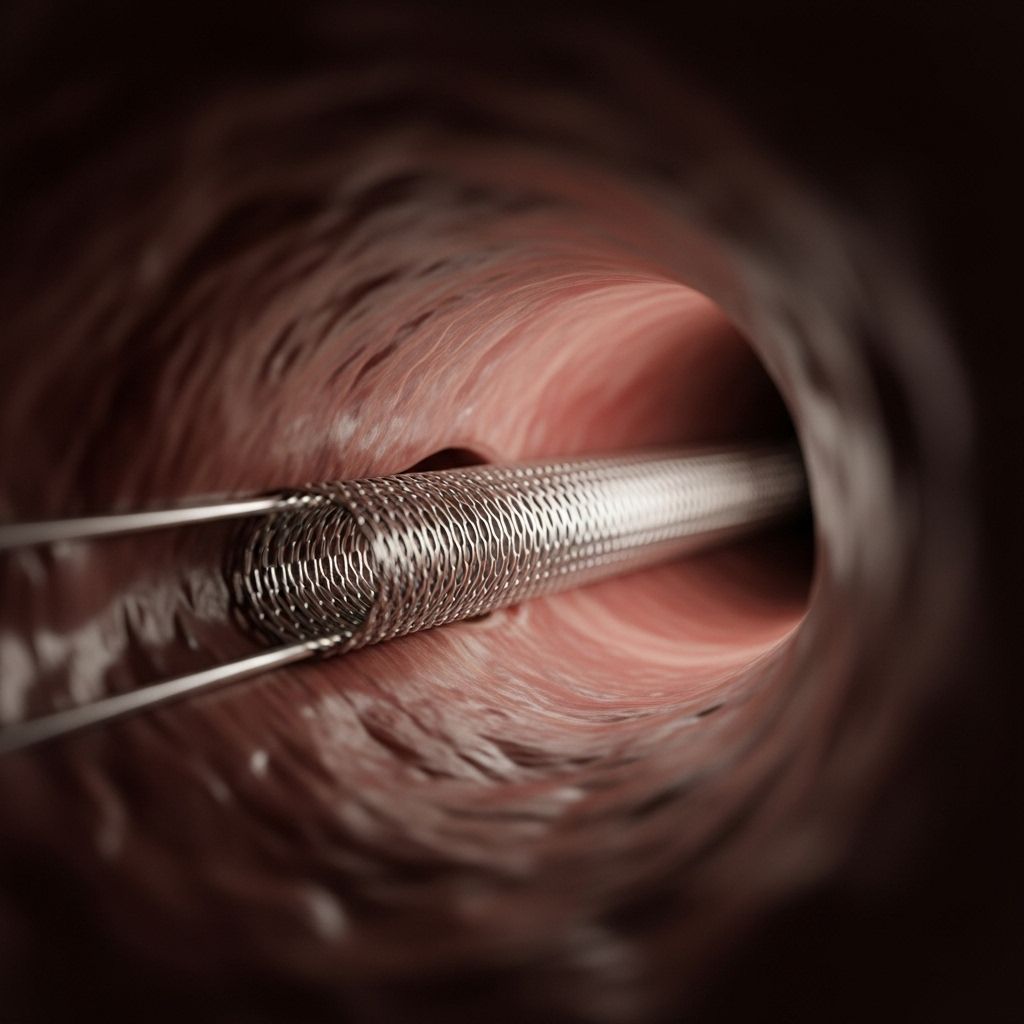
Stents play a vital role in the treatment of narrowed or blocked arteries, especially in coronary artery disease. These tiny mesh tubes help keep arteries open, restoring and maintaining proper blood flow. While stents are designed to be permanent fixtures in the body, various factors can influence their actual lifespan and effectiveness. This article explores how long stents usually last, what affects their durability, and how patients can enhance their heart health following stent placement.
What Is a Stent and Why Is It Used?
A stent is a small, expandable mesh tube placed inside an artery during a procedure known as angioplasty. Its primary purpose is to reopen a clogged or narrowed artery and help it remain open, reducing the risk of heart attack and other vascular complications.
- Permanent Solution: Once inserted, most stents stay in the body permanently and do not dissolve or degrade over time.
- Restores Blood Flow: Stents immediately restore proper circulation to tissue deprived of essential oxygen and nutrients.
- Commonly Used In:
- Coronary arteries (for heart attacks or coronary artery disease)
- Carotid arteries (to prevent stroke)
- Peripheral arteries (to treat conditions like peripheral artery disease)
The Typical Lifespan of a Stent
Stents are fabricated to be long-lasting, often intended to stay in place for the rest of a patient’s life. However, their long-term effectiveness can depend on the type of stent used, the location in the body, and the patient’s overall heart health and adherence to prescribed medications and lifestyle changes.
- Most metallic stents (such as bare-metal and drug-eluting stents) are intended as permanent implants and do not break down over time.
- Bioresorbable stents are designed to dissolve gradually, typically over 1–3 years, though these are less commonly used than permanent stents.
When a re-narrowing of a stented artery (restenosis) does occur, it typically happens within the first 1 to 6 months following placement. Beyond that period, the risk decreases, but blockages can develop over longer timeframes if underlying conditions aren’t well managed.
Where Are Stents Used in the Body?
Stents are most commonly placed in:
- Coronary arteries (supplying the heart muscle)
- Carotid arteries (supplying the brain)
- Peripheral arteries (supplying arms and legs)
- Renal arteries (supplying the kidneys)
Though the general function and lifespan of a stent are similar regardless of the vessel, the type of stent, risks of re-narrowing, and specific aftercare recommendations may vary by location.
Types of Stents and Their Durability
The longevity and performance of a stent depend significantly on its type. There are three main categories of stents used in clinical practice:
- Bare-Metal Stents (BMS):
- Simple metal mesh tubes.
- Designed to be a permanent support for the artery.
- Higher risk of restenosis (re-narrowing) compared to drug-eluting stents.
With advancements in technology, drug-eluting stents are becoming a preferred choice for many patients. Discover how they work and the vital benefits they offer by checking out our resource on drug-eluting stents: their function, benefits, risks, and preventive measures you should know. - Drug-Eluting Stents (DES):
- Metal mesh stents coated with slow-release medication.
- Designed to prevent excessive tissue growth inside the artery, reducing restenosis rates.
- Permanently implanted.
- Bioresorbable (Biodegradable) Stents:
- Made from materials that dissolve within months to a few years.
- Designed to leave the vessel as natural as possible, though clinical effectiveness and safety are still being studied.
The process of angioplasty combined with stent placement is critical for treating heart issues effectively. To gain a clear understanding of this procedure, explore our in-depth resource on angioplasty and stent placement for heart conditions, including procedures, recovery, and associated risks.
| Stent Type | Material | Lifespan | Restenosis Risk |
|---|---|---|---|
| Bare-Metal | Metal mesh | Permanently implanted | Higher |
| Drug-Eluting | Metal (& medicine) | Permanently implanted | Lower than BMS |
| Bioresorbable | Polymer/composite | 1–3 years (self-dissolving) | Data still emerging |
Why Arteries Can Re-Narrow (Restenosis) After Stenting
While stents keep arteries open, they only address the localized blockage, not the underlying disease that caused it. There are several reasons why an artery might re-narrow after a stent:
- Tissue Growth: Scar tissue may form inside the stent.
- Plaque Buildup: Fatty deposits can form again within or near the stent.
- Blood Clots (Stent Thrombosis): Blood may clot around the stent, potentially blocking the artery.
- Progression of Disease: Atherosclerosis or other vascular conditions can cause new blockages elsewhere in the arteries.
The highest risk for in-stent restenosis or clotting is typically within the first 1 to 6 months following the procedure. After that, the risk drops significantly as long as prescribed medications, such as blood thinners, are taken diligently.
Symptoms of Restenosis or Stent Complications
- Recurring chest pain (angina)
- Shortness of breath
- Unusual fatigue
- Heart palpitations
If you experience symptoms similar to those that resulted in your stent placement, seek medical evaluation promptly.
Do Stents Ever Need to Be Replaced?
Most stents are designed to be permanent, and needing a replacement is rare. However, a repeat angioplasty or additional stenting may be needed if:
- There is restenosis (re-narrowing) in the same artery segment.
- The patient develops new blockages in other parts of the arteries.
- There are complications such as stent thrombosis (a blood clot within the stent).
Replacement or additional stenting is based on ongoing symptoms and follow-up imaging findings, not on a routine schedule.
What Factors Affect How Long a Stent Lasts?
The longevity and effectiveness of a stent are influenced by several key factors:
- Stent type: Drug-eluting stents generally last longer and are more effective at preventing restenosis than bare-metal stents.
- Location: Some arteries may be more prone to complications or re-narrowing than others.
- Patient’s health: Smoking, high blood pressure, high cholesterol, and uncontrolled diabetes increase the risk of restenosis.
- Medication adherence: Not taking prescribed anti-platelet drugs can increase risk of blood clots and complications.
- Genetics and individual healing response: Some people heal with more scar tissue, increasing the risk of restenosis.
Lifestyle and Medical Management After Stent Placement
Stent placement is only one part of a broader plan to manage heart disease and prevent future blockages. The following steps are critical to long-term success:
- Take all prescribed medications: Anti-platelet drugs (such as aspirin and clopidogrel) are essential to prevent clotting around the stent.
- Follow a heart-healthy diet: Emphasize fruits, vegetables, whole grains, lean proteins, and healthy fats. Reduce salt, sugar, and saturated fats.
- Exercise regularly: Engage in moderate physical activity as recommended by your healthcare provider.
- Manage other health conditions: Keep blood pressure, cholesterol, and diabetes under control with personalized treatment plans.
- Quit smoking: Smoking dramatically increases the risk of heart disease progression and restenosis.
- Attend follow-up appointments: Regular medical check-ups help monitor the stent and overall heart health.
Outlook: Life After a Stent
The prognosis after stent placement varies depending on age, overall health, presence of other heart conditions, and lifestyle choices. Generally:
- Many people live healthy, active lives for many years after receiving a stent.
- Those diagnosed at a younger age with fewer additional health problems typically have the best long-term outcomes.
- Simply having a stent does not cure the underlying heart or vascular disease. Ongoing risk factor management is essential to prevent future issues.
Frequently Asked Questions (FAQs)
How long does a coronary stent actually last?
Most coronary stents are designed to last a lifetime and remain permanently in place. However, the risk of the artery narrowing again (restenosis) is highest in the first 6 months. With proper medical care and lifestyle management, most people do not require replacement of their stent.
Do stents dissolve over time?
Most stents are made of metal and are permanent. A few newer bioresorbable stents are designed to dissolve naturally within a few years, though their use is less widespread compared to permanent stents.
Can you need another stent or repeat procedure?
Yes, some people may require more than one stent, especially if new blockages occur or if there is restenosis in the original stented area. Repeat procedures are guided by new symptoms or imaging findings rather than routine scheduling.
What should I avoid after getting a stent?
Avoid stopping blood thinners or prescribed medications without your doctor’s guidance. Also avoid unhealthy habits such as smoking, poor diet, and inactivity, all of which increase your risk of restenosis and other complications.
Will a stent cure my heart disease?
No, a stent treats only the blocked segment of an artery. The overall process of atherosclerosis or vascular disease continues, so lifelong management with medications, healthy lifestyle, and regular doctor visits is critical.
Key Takeaways
- Stents are designed to be permanent.
- The risk of restenosis is highest within 1–6 months post-placement.
- Most stents don’t need replacement but may require additional stents if blockages occur elsewhere.
- Adhering to medication, healthy lifestyle, and regular follow-up care is crucial for long-term success.
References
- https://www.healthline.com/health/heart-disease/how-long-do-stents-last
- https://abcnews.go.com/Health/HeartDiseaseLivingWith/story?id=4224509
- https://www.vinmec.com/eng/blog/life-expectancy-with-coronary-stents-en
- https://www.medipulse.in/blog/understanding-the-lifecycle-of-a-stent-in-the-heart
- https://pubmed.ncbi.nlm.nih.gov/12081992/
- https://www.dxnimble.com/how-long-do-coronary-stents-last-and-factors-that-influence-their-lifespan/
- https://www.medicalnewstoday.com/articles/do-stents-need-to-be-replaced
- https://adcacardiology.com/your-health/video/heart-stent-life-span
Read full bio of Sneha Tete












