Hip Labral Tear: Causes, Symptoms, Diagnosis & Treatment
A comprehensive guide to understanding hip labral tears, from causes and symptoms to modern diagnosis methods and advanced treatment options.
Hip Labral Tear
A hip labral tear is a condition that affects the soft tissue surrounding the hip joint, leading to pain, joint instability, and difficulty performing daily activities. This injury commonly affects athletes but can impact anyone. Early diagnosis and proper management are essential to prevent complications and restore optimal function.
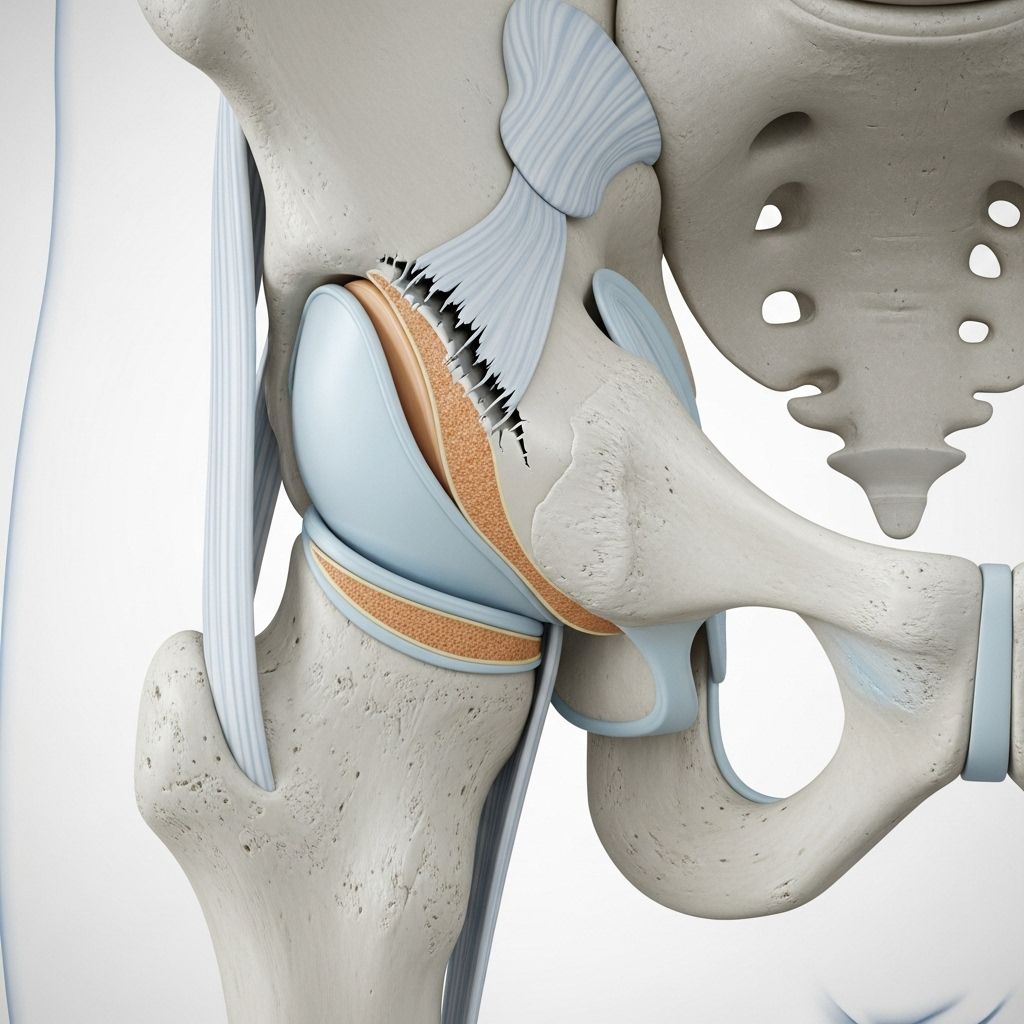
What is a Hip Labral Tear?
The labrum is a ring of strong, rubbery cartilage (fibrocartilage) that lines the outer rim of the hip socket (acetabulum). The labrum acts as a cushion and seal, stabilizing the “ball and socket” joint formed between the acetabulum and the femoral head (the top of the thighbone). When the labrum is torn, the seal can be disrupted, allowing the joint to become less stable and less lubricated, leading to pain and mechanical symptoms (like clicking or locking).
- Acetabular labrum: The specific labral structure in the hip, covers the acetabulum’s rim.
- Functions: Provides hip stability, absorbs shock, and maintains normal joint fluid pressure.
- Location: Encircles the socket where the femur (thighbone) meets the pelvis.
Causes of Hip Labral Tears
Hip labral tears develop due to a range of structural, mechanical, and traumatic factors. Sometimes, more than one cause may be present simultaneously.
- Structural Abnormalities: Conditions like femoroacetabular impingement (FAI) and hip dysplasia alter bone contours, causing excess stress on the labrum during hip movement.
- Repetitive Motions: Activities involving frequent hip flexion, twisting, or pivoting (e.g., soccer, ballet, hockey) may gradually wear down and eventually tear the labrum.
- Trauma: Acute incidents, such as falls, traffic accidents, or sports collisions, can damage the labral tissue and even dislocate the hip.
- Degenerative Changes: With aging or in osteoarthritis, the hip joint and labral tissue may gradually weaken and tear due to long-term wear and tear.
Risk Factors
- Active involvement in sports with repetitive hip movements (soccer, football, ballet, hockey).
- Femoroacetabular impingement (FAI) or hip dysplasia (congenital abnormal hip shapes).
- Previous hip injury, particularly high-impact trauma leading to joint instability.
- Age-related degeneration, especially in older adults with preexisting osteoarthritis.
- Repeated twisting or pivoting motions associated with jobs or activities that require frequent hip motion.
Signs & Symptoms
Symptoms of a hip labral tear can be subtle or pronounced, and occasionally mistaken for other hip problems. Common signs include:
- Hip or groin pain, typically described as a deep ache, sometimes sharp, worsened by sitting, motion, or prolonged standing.
- Mechanical symptoms, such as locking, clicking, or “catching” of the hip joint during movement.
- Stiffness or reduced range of motion when moving or rotating the hip.
- Sensation of instability—feeling that the hip might “give way.”
- Increased discomfort during activities requiring flexion or rotation (running, squatting, getting out of a car).
When to See a Doctor
Consult a healthcare provider if you experience:
- Persistent hip or groin pain lasting more than a few days.
- Repeated popping, clicking, or catching sensations in the hip.
- Difficulty with activities such as walking, bending, rotating the hip, or engaging in sports.
- Any significant injury to the hip, especially with immediate pain and loss of motion.
Diagnosis of Hip Labral Tears
A comprehensive approach is used to diagnose a hip labral tear. This may include a combination of medical history, physical examination, and advanced imaging. Key diagnostic steps are:
- Medical History: Review of symptoms, onset of pain, injury history, and activity level.
- Physical Exam: Doctors assess hip motion, looking for pain with flexion, internal rotation, or provocative maneuvers (such as impingement or FABER test). They inspect gait and check for mechanical symptoms.
- X-rays: Help assess bone shape abnormalities and rule out arthritis or bone spurs.
- Magnetic Resonance Imaging (MRI) or MR Arthrogram: These scans visualize the labrum and provide direct evidence of a tear, as well as helping rule out other causes of hip pain.
- Diagnostic Injections: Occasionally, a local anesthetic may be injected into the joint. If pain relief follows, this suggests the hip joint (and potentially the labrum) is the origin of symptoms.
| Diagnostic Tool | Description | What It Shows |
|---|---|---|
| X-ray | Standard imaging of bone anatomy. | Bony abnormalities, spurs, dysplasia, no direct labrum detail. |
| MRI/MR Arthrogram | Advanced imaging of soft tissue with/without contrast. | Labral tears, cartilage and some ligament injury. |
| Physical Exam Tests | Hands-on movements and provocative maneuvers. | Pain, instability, mechanical symptoms, and limited motion. |
| Diagnostic Injection | Injecting anesthetic into joint space. | Confirms the joint as primary pain source. |
Treatment Options
Treatment for a hip labral tear is individualized, based on the severity, underlying cause, and activity goals. Management options include conservative (nonsurgical) and surgical interventions.
Conservative (Nonsurgical) Treatments
- Rest and Activity Modification: Limiting activities that aggravate hip pain, such as high-impact sports, and adopting alternatives like swimming or cycling.
- Physical Therapy: Aimed at strengthening the muscles that stabilize the hip (core, gluteal muscles), improving flexibility, and correcting movement patterns. Therapy includes guided exercises, functional training, and sometimes neuromuscular reeducation.
- Medications: Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen help reduce pain and inflammation.
- Corticosteroid Injections: Sometimes used to reduce swelling and pain within the hip joint, allowing improved participation in therapy and daily activities.
Surgical Treatments
If conservative treatments are unsuccessful, especially for those with persistent pain or mechanical symptoms, arthroscopic hip surgery may be recommended. Surgical options include:
- Labral Repair: Sewing the torn labrum back together using sutures and anchors. Preserves as much of the labral tissue as possible.
- Labral Debridement: Removing or smoothing out torn, frayed labral segments that cannot be repaired.
- Labral Reconstruction: For severely damaged or irreparable labra, a graft (usually tendon tissue) is used to replace the labrum’s function.
- Bony Correction: If structural abnormalities (like FAI) are present, surgeons may reshape the femoral head or acetabular rim to prevent recurrence.
Arthroscopic surgery is minimally invasive, uses small incisions, and usually performed outpatient. Postoperative periods involve crutch use (about 2 weeks), with a planned, gradual return to activities based on healing and physical therapy progress.
Recovery and Rehabilitation
Recovery from a hip labral tear depends on the method of treatment and the underlying cause. Physical therapy is central to both nonsurgical and postoperative recovery. Key steps include:
- Pain and swelling control: Using ice, medications, and careful activity progression.
- Restoration of hip range of motion: Gradual stretching and mobility exercises guided by a physical therapist.
- Strengthening the hip and core muscles: Prevents future injury by stabilizing the joint.
- Functional retraining: Includes movements and activities of daily living as well as sport-specific drills when ready.
- Return to sports or vigorous activity: Usually several months after surgery, based on pain resolution and strength/mobility benchmarks.
Prevention and Long-term Outlook
- Maintain strong hip and core muscles to support joint stability.
- Warm up thoroughly before exercise; incorporate flexibility and strengthening routines.
- Use correct form during activities involving hip loading and rotation.
- Avoid repetitive high-impact activities when possible, especially if you have anatomic predispositions.
- Address hip pain early—timely intervention can prevent worsening of the injury and reduce complications like arthritis.
With proper treatment—including early recognition, structured rehabilitation, and surgical options for severe cases—most individuals return to pre-injury activity levels. Left untreated, recurrent symptoms may accelerate cartilage damage and increase the risk for developing osteoarthritis in the hip.
Frequently Asked Questions (FAQs)
Q: What happens if a hip labral tear is left untreated?
A: Untreated labral tears may lead to chronic pain, worsening mechanical symptoms (clicking, catching), and increased risk of cartilage degradation or hip osteoarthritis over time.
Q: Can you walk with a labral tear in your hip?
A: Many people can walk, though pain, stiffness, or instability may be present. Walking might be more difficult during flares or after activity. Severe tears or those with impingement may cause significant movement limitations.
Q: Is hip labral tear surgery always required?
A: Not always. Many people recover with rest, therapy, and medication. Surgery is reserved for tears that do not resolve with conservative treatment or those causing persistent symptoms or instability.
Q: How long does recovery from hip labral repair surgery take?
A: Full recovery varies. Most people use crutches for about 2 weeks, begin gentle therapy within the first week, and return to sports or strenuous activity in 3–6 months, depending on the repair, rehabilitation progress, and overall health.
Q: What activities should I avoid after a hip labral tear?
A: Activities involving deep flexion (squatting, lunges), high-impact sports (running, jumping), or rapid pivoting/rotating movements should be avoided until advised by your healthcare provider. Gradual return to these activities is guided by pain levels, hip strength, and range of motion improvements.
Resources
- Consult a board-certified orthopedic surgeon or sports medicine specialist for assessment and individualized treatment planning.
- Physical therapists can tailor rehabilitation programs based on your injury, activity level, and recovery phase.
- For persistent or worsening symptoms, advanced imaging and multidisciplinary hip preservation programs are available at major hospitals and academic centers.
References
- https://www.yalemedicine.org/conditions/hip-labral-tears
- https://www.ucsfhealth.org/conditions/hip-labral-tear
- https://my.clevelandclinic.org/health/diseases/17756-hip-labral-tear
- https://www.mayoclinic.org/diseases-conditions/hip-labral-tear/diagnosis-treatment/drc-20354878
- https://www.massgeneralbrigham.org/en/patient-care/services-and-specialties/sports-medicine/conditions/hip/labral-tear
- https://www.pennmedicine.org/conditions/hip-labral-tear
- https://www.hss.edu/health-library/conditions-and-treatments/list/hip-labral-tear
- https://www.froedtert.com/orthopaedics/hip-preservation/torn-labrum-hip
- https://www.mayoclinic.org/diseases-conditions/hip-labral-tear/symptoms-causes/syc-20354873
Read full bio of Sneha Tete












