Herpes Simplex Virus (HSV-1 and HSV-2): Types, Symptoms, and Treatment
Learn about HSV-1 and HSV-2: key differences, signs, complications, and effective treatment strategies.
Herpes Simplex Virus (HSV-1 and HSV-2): Understanding Types, Symptoms, and Treatment
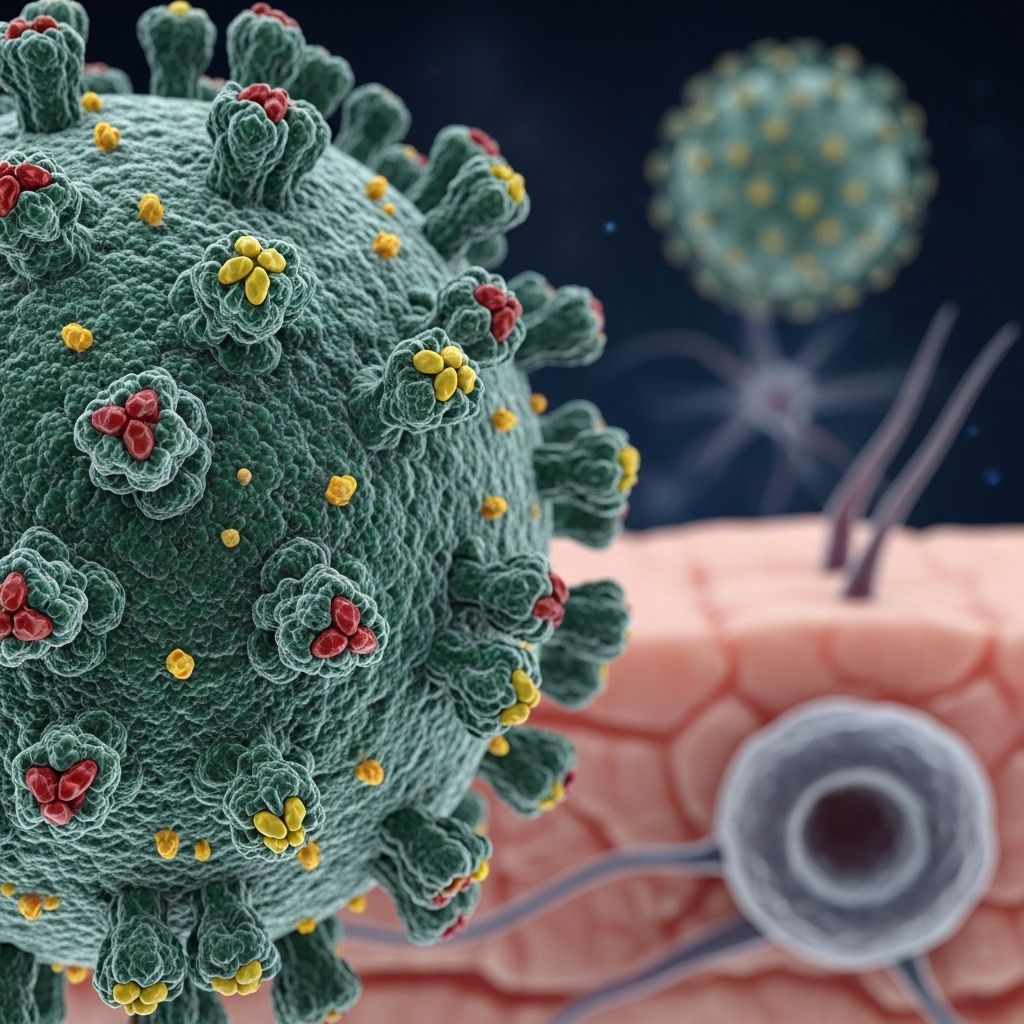
The herpes simplex virus (HSV) is a widespread and persistent infection that can cause sores and blisters on the mouth, genitals, or other parts of the body. There are two main types of HSV: HSV-1, typically linked to oral herpes, and HSV-2, more commonly associated with genital herpes. Both types are lifelong infections, and understanding their transmission, clinical features, and management is vital for effective care and prevention.
What is Herpes Simplex Virus?
Herpes simplex virus belongs to the herpesvirus family and is categorized mainly into two strains:
- HSV-1: Often causes oral herpes — cold sores or fever blisters around the mouth and on the face but can also infect the genital area.
- HSV-2: Primarily responsible for genital herpes, characterized by sores in the genital and rectal area but can occasionally affect the mouth.
How Widespread is HSV?
HSV infections are extremely common worldwide:
- HSV-1: Most people contract HSV-1 in childhood through nonsexual contact, such as kissing or sharing utensils.
- HSV-2: Typically acquired in adolescence or adulthood, mainly through sexual activity.
According to global public health data, an overwhelming majority of adults have HSV-1, and a significant portion of the population contracts HSV-2 by mid-adulthood.
Differences Between HSV-1 and HSV-2
| Feature | HSV-1 | HSV-2 |
|---|---|---|
| Common Site of Infection | Mouth/lips (oral region), possible genital area | Genital and anal regions |
| Transmission Pathway | Oral secretions or sores (kissing, utensils) | Sexual contact (vaginal, anal, oral sex) |
| Typical Recurrence | Less frequent when in genital area | Often more severe and recurrent outbreaks |
| Age of Initial Infection | Usually childhood | Usually adolescence/adulthood |
Both HSV-1 and HSV-2 can infect the oral or genital regions, but their primary and most common sites of infection help distinguish them. Notably, HSV-2 is almost always sexually transmitted, while HSV-1 can be spread via nonsexual or sexual contact.
Causes and Transmission
HSV spreads via direct contact with infected skin or bodily fluids. The likelihood of transmission is highest during an active outbreak (when sores are present), but the virus can also spread when no symptoms are visible due to asymptomatic viral shedding.
- HSV-1: Passed through saliva, kissing, sharing eating utensils, lip balm, or razors. It can also be transmitted to the genital area during oral sex.
- HSV-2: Primarily transmitted through vaginal, anal, or oral sex. Condoms reduce risk but do not eliminate it entirely.
Symptoms are more likely to occur the first time someone gets infected, and recurrences can be triggered by factors like stress, illness, sun exposure, or a weakened immune system.
Signs and Symptoms of HSV-1 and HSV-2
Many individuals infected with HSV remain unaware because symptoms can be mild or absent. When symptoms do appear, they typically follow these patterns:
- Initial Infection
- Painful blisters or sores on the mouth, lips, genitals, or nearby skin
- Tingling, itching, or burning sensation before sores appear
- Swollen lymph nodes
- Fever, muscle aches, and general malaise (especially with first episode)
It's crucial to differentiate between various skin conditions, especially if you're experiencing recurring sores. For clarity on distinguishing between angular cheilitis and cold sores, review our comparison of Angular Cheilitis vs. Cold Sores: Signs, Causes, and Treatments. Understanding these conditions can significantly affect management and treatment choices. - Recurrent Episodes
- Milder symptoms: fewer sores, less pain
- Often limited to a specific area and heal faster than initial outbreak
Triggers for Recurrence include:
- Physical or emotional stress
- Fever or illness
- Menstruation
- Sun exposure (especially with oral herpes)
- Injury to affected area
Complications of HSV
Most HSV infections remain localized and resolve without lasting effects. However, complications can occasionally occur, especially in people with weakened immune systems:
- Secondary skin infections by bacteria (due to open sores)
- Eye infections (herpes keratitis), can threaten vision if untreated
- Spread to the central nervous system (e.g., herpes encephalitis, rare)
- Neonatal herpes: dangerous infection in newborns, can occur if the mother has active genital herpes during vaginal delivery
Diagnosing Herpes Simplex Virus
An accurate diagnosis ensures appropriate management and helps prevent transmission:
- Clinical examination: Identifying characteristic sores or blisters.
- Viral culture or PCR test: Swab of active sore can confirm HSV and determine type (HSV-1 or HSV-2).
- Blood tests: Can detect HSV antibodies, indicating past or current infection–useful when no active sores are present.
Early medical evaluation is important because other conditions can resemble herpes, and a correct diagnosis will guide both physical and emotional management.
Treatment Options for HSV-1 and HSV-2
Goals of Treatment
- Relieve symptoms during outbreaks
- Shorten duration and severity of episodes
- Reduce frequency of recurrences
- Lower risk of transmitting HSV to others
There is no cure for herpes simplex. The virus remains dormant in nerve cells and can reactivate later. However, antiviral medicines can manage symptoms effectively and reduce outbreaks.
Types of Treatment
- Episodic Treatment
- Short course of antiviral medication (e.g., acyclovir, famciclovir, valacyclovir) at onset of outbreak
- Reduces pain, severity, and duration of current episode
- Suppressive Therapy
- Daily antiviral medication for people with frequent recurrences or severe symptoms
- Helps reduce outbreaks by up to 80%
- Lowers the likelihood of transmitting the virus to sexual partners
- Supportive Care
- Over-the-counter pain medications (acetaminophen, ibuprofen)
- Benzocaine/lidocaine creams for local numbing
- For oral herpes: sucking on ice pops, avoiding acidic foods
- For genital herpes: sitz baths, loose-fitting clothing
Suppressive therapy is also recommended for people seeking to reduce the risk of transmission to an uninfected partner. Routine lab monitoring is not needed, as long-term antiviral use is considered safe.
Managing Recurrent HSV Infections
- People with frequent outbreaks or severe psychological distress may benefit from daily suppressive therapy.
- Triggers like stress and illness should be minimized where possible (e.g., stress management, adequate rest, using sunscreen for oral herpes).
- Suppressive therapy is discontinued periodically to reassess the frequency of recurrences; frequency often decreases over time.
Prevention Strategies
- Avoid sex during active symptoms or when prodromal signs (itching, tingling) appear
- Consistent and correct condom use reduces (but does not eliminate) risk
- Open communication with sexual partners regarding HSV status
- No sharing of personal items that touch an individual’s mouth or sores (lip balm, utensils, razors)
- Pregnant women with genital herpes must inform their health care provider to prevent neonatal herpes
Living with Herpes Simplex Virus
A diagnosis of HSV can cause emotional distress and anxiety. It is important to know that HSV is a common medical condition and can be managed effectively. Most people with HSV lead full, healthy lives with few restrictions.
- Support groups and counseling can help address emotional concerns
- Education about the virus reduces stigma and improves self-care
- Medical therapy and preventive practices help minimize long-term impact
Frequently Asked Questions (FAQs)
Q: Is there a cure for herpes simplex virus?
A: No, there is no cure for HSV. The virus remains in the body for life, but symptoms can be managed and outbreaks reduced with medication and self-care.
Q: Can HSV-1 cause genital herpes?
A: Yes, HSV-1 can infect the genital area, especially through oral-genital contact. Both HSV-1 and HSV-2 can cause genital herpes, though HSV-2 is most common.
Q: How is herpes most commonly transmitted?
A: HSV-1 is usually spread via oral secretions, while HSV-2 is mainly transmitted through sexual contact. Both types can spread even if no visible sores are present.
Q: Are there any serious complications?
A: Most cases are mild, but HSV can rarely cause severe complications like herpes encephalitis, neonatal herpes (if a mother has active genital herpes during delivery), or eye infections. Prompt medical attention is important for these cases.
Q: How can I reduce the risk of passing HSV to someone else?
A: Avoid contact during active outbreaks, use condoms consistently, talk to partners about your HSV status, and consider daily suppressive therapy if you have frequent recurrences or are concerned about transmission.
Q: What should pregnant women know about HSV?
A: Pregnant women with HSV should inform their healthcare provider, as precautions may be necessary to prevent transmission to the newborn, which can be serious.
Q: Can I get HSV from public surfaces or pools?
A: HSV is not transmitted via surfaces, pools, or toilet seats—it requires direct contact with infected skin or secretions.
Key Points to Remember
- Herpes simplex virus infections (HSV-1 and HSV-2) are extremely common and lifelong.
- Symptoms can range from none to painful sores; both types can infect the mouth or genitals.
- Diagnosis is made by examining sores, viral or blood testing.
- While there is no cure, antiviral treatments can decrease outbreaks and transmission.
- Simple strategies—like avoiding contact during outbreaks, using condoms, and communicating with partners—help reduce transmission risk.
- Most people with HSV live healthy, active lives, and emotional support is available for those affected.
References
- https://ccrsfl.com/understanding-hsv-1-and-hsv-2-a-comprehensive-guide-to-herpes-simplex-virus/
- https://www.cdc.gov/std/treatment-guidelines/herpes.htm
- https://www.who.int/news-room/fact-sheets/detail/herpes-simplex-virus
- https://my.clevelandclinic.org/health/diseases/22855-herpes-simplex
- https://www.webmd.com/genital-herpes/pain-management-herpes
- https://health.mit.edu/faqs/herpes
- https://virologyresearchservices.com/2024/12/11/herpes-simplex-virus-understanding-hsv-1-and-hsv-2/
- https://www.ondemand.labcorp.com/blog/what-to-know-herpes-hsv-1-hsv-2
Read full bio of Sneha Tete












