Hepatitis C: Symptoms, Causes, and Risk Factors
Understand the symptoms, causes, and risk factors of hepatitis C, a silent viral infection that can severely damage the liver over time.
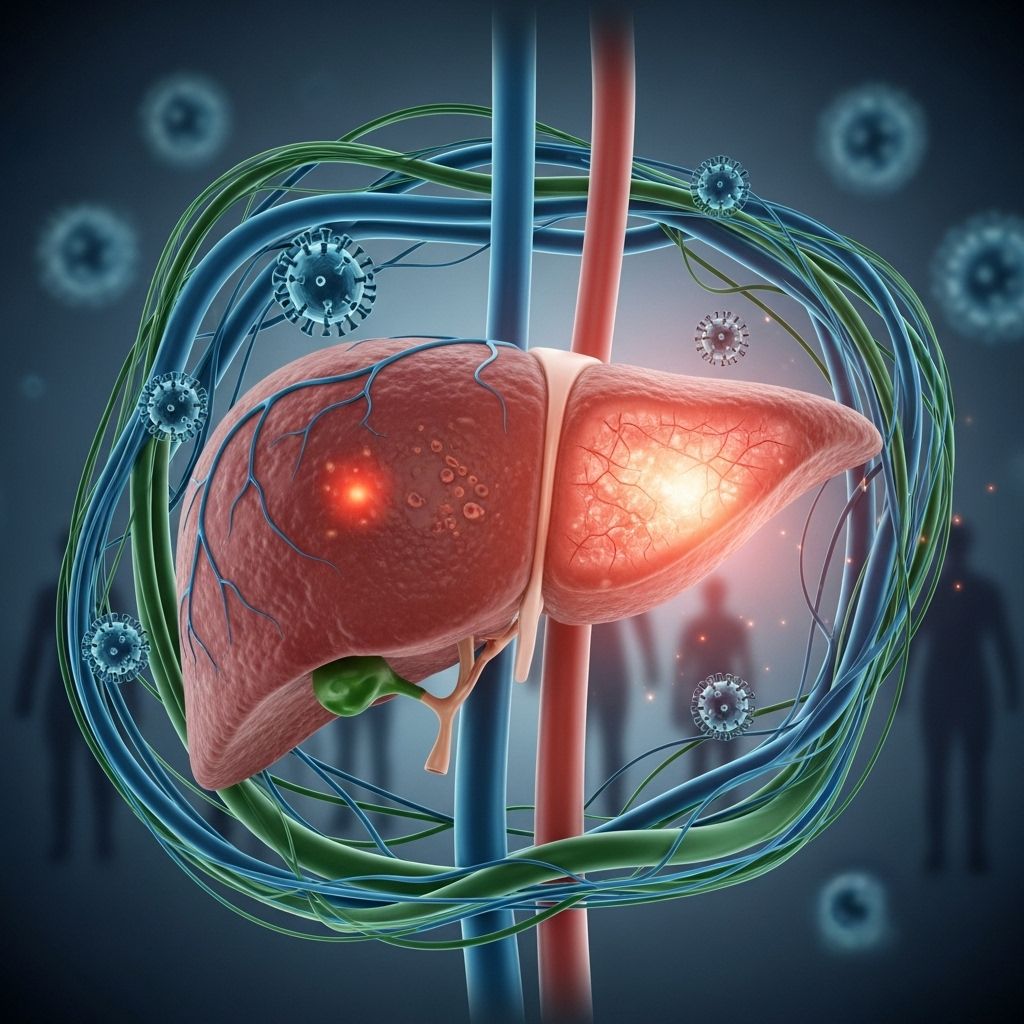
Hepatitis C is a viral infection primarily affecting the liver, causing inflammation and possibly leading to severe liver damage if left untreated. Unlike many other diseases, hepatitis C often remains unnoticed for years due to its subtle or absent early symptoms, making awareness and early screening essential for effective management and prevention of complications.
Overview of Hepatitis C
Hepatitis C is caused by the hepatitis C virus (HCV). This infection can appear in two forms:
- Acute hepatitis C: The initial stage, sometimes producing mild or no symptoms. Many acute cases go undetected.
- Chronic hepatitis C: A long-term infection that persists over years, progressing silently and leading to substantial liver damage over time.
Globally, hepatitis C is a significant health concern, with millions affected. The development of advanced antiviral treatments in recent years has improved outcomes, but undiagnosed cases remain common due to the infection’s stealthy nature.
Symptoms
The clinical presentation of hepatitis C varies according to the phase of infection and the extent of liver damage.
Acute Hepatitis C
During the acute phase, most people experience few or no symptoms. When symptoms do occur, they often resemble a mild illness and may appear one to three months after exposure. Symptoms of acute hepatitis C, if present, can include:
- Jaundice (yellowing of skin and eyes, more noticeable in lighter skin tones)
- Fatigue
- Nausea
- Fever
- Muscle aches
- Loss of appetite
Most acute cases are not diagnosed as symptoms are non-specific or absent.
Chronic Hepatitis C
The infection becomes chronic when the virus persists for more than six months. Chronic hepatitis C is often asymptomatic for years. When symptoms develop as liver damage advances, they may include:
- Easy bleeding or bruising
- Prolonged fatigue
- Poor appetite
- Jaundice, especially evident in the whites of the eyes
- Dark-colored urine
- Itchy skin
- Fluid buildup in the abdomen (ascites)
- Swelling in the legs
- Weight loss
- Confusion, drowsiness, and slurred speech (hepatic encephalopathy)
- Spiderlike blood vessels visible on the skin (spider angiomas)
These symptoms generally appear only after extensive liver injury has occurred. Many individuals learn of their hepatitis C infection incidentally, often through routine blood tests or screening.
End-Stage Disease and Complications
If chronic hepatitis C is not treated, it may lead to:
- Cirrhosis: Irreversible scarring of the liver, leading to loss of liver function.
- End-stage liver disease: Marked by severe symptoms such as persistent jaundice, intense itching, abdominal pain, inability to concentrate, and easy bleeding.
- Hepatocellular carcinoma: Elevated risk for liver cancer.
- Liver failure: The only effective treatment at this stage is often liver transplantation.
Treating hepatitis C before the onset of cirrhosis is crucial for improving long-term prognosis.
Causes
Hepatitis C infection is caused by the hepatitis C virus (HCV), which is transmitted primarily through blood-to-blood contact. The most common methods of transmission include:
- Sharing of injection drug equipment: Contaminated needles and syringes are the leading cause of new infections.
- Blood transfusion and organ transplants: Becoming much less common since the introduction of HCV screening in blood products in the early 1990s, but possible before those safeguards.
- Healthcare exposures: Accidental needle-stick injuries and occupational exposure to blood in healthcare settings.
- Mother-to-child transmission: Infection passed from mother to newborn during childbirth.
- Unprotected sex: Especially among men who have sex with men or people with multiple partners, though this mode is less common than direct blood exposure.
- Sharing personal items: Such as razors or toothbrushes that may contain traces of infected blood, though this is rare.
- Piercings and tattoos: Done with non-sterile equipment.
Saliva, urine, and other body fluids are not significant routes of transmission unless visibly contaminated with blood.
HCV Genotypes
Globally, HCV has multiple genotypes—seven major types and numerous subtypes. The most common genotype in the United States is type 1. The clinical course of hepatitis C is similar for all genotypes, but treatment plans may vary depending on the genotype, as some respond differently to antiviral medications. Modern therapies target a broad range of genotypes, improving outcomes across populations.
Risk Factors
Understanding who is at risk for hepatitis C enables effective prevention, early diagnosis, and management. People at higher risk include:
- Anyone who has ever injected, inhaled, or snorted an illegal drug (even once)
- Individuals with unexplained abnormal liver test results
- Babies born to mothers with hepatitis C
- Pregnant individuals (screening is recommended during pregnancy)
- Healthcare and emergency workers exposed to blood or accidental needle-stick injuries
- People with hemophilia treated with clotting factor products before 1987
- Long-term hemodialysis patients
- Recipients of blood transfusions or organ transplants before 1992
- Sexual partners of anyone diagnosed with hepatitis C
- People with HIV infection
- Men who have sex with men
- Sexually active people about to start pre-exposure prophylaxis (PrEP) for HIV
- Individuals with a history of incarceration (prison populations)
Screening Recommendations
The U.S. Preventive Services Task Force recommends all adults between 18 and 79 years old undergo hepatitis C screening at least once, with repeat testing for those at higher ongoing risk. This universal screening is vital because hepatitis C causes few or no symptoms for many years and can silently damage the liver.
Progression of Hepatitis C Infection
The pathway of hepatitis C infection typically follows these stages:
- Acute phase: May resolve spontaneously in some people (called spontaneous viral clearance) without medical intervention. Others progress to chronic infection.
- Chronic infection: Ongoing inflammation over years, leading to fibrosis, cirrhosis, liver failure, or liver cancer.
- Spontaneous clearance: Occurs in a minority who, after acute infection, clear HCV naturally, especially with strong individual immune responses.
- Response to treatment: Modern antiviral therapy can cure hepatitis C in most cases, even after chronic infection.
Complications of Chronic Hepatitis C
| Complication | Description | Potential Outcomes |
|---|---|---|
| Cirrhosis | Long-term scarring and damage of the liver tissue | Can progress to liver failure, increased cancer risk |
| Liver Cancer (Hepatocellular carcinoma) | Development of malignant tumors in liver tissue | May be fatal, requires early detection and possible liver transplantation |
| Liver Failure | Severe loss of liver function due to widespread tissue destruction | Mainly treatable with liver transplant at this stage |
| Other Systemic Complications | Kidney disease, metabolic disorders, blood vessel conditions | Compromised overall health and increased mortality risk |
Frequently Asked Questions (FAQs)
Q: What is hepatitis C?
A: Hepatitis C is a viral liver infection caused by hepatitis C virus (HCV) that leads to liver inflammation. Chronic infection can result in significant liver damage, including cirrhosis and liver cancer.
Q: What are the main symptoms?
A: Most people have no symptoms for years. When symptoms arise, they may include fatigue, easy bruising or bleeding, jaundice, itchy skin, fluid buildup in the abdomen or swelling in the legs, and cognitive changes due to liver dysfunction.
Q: How is hepatitis C transmitted?
A: Transmission occurs primarily through contact with blood infected by HCV, most commonly via shared needles, past unscreened blood transfusions, or needle-stick injuries. Less common routes include sex with an infected partner, mother-to-child transmission at birth, or using unsterilized tattoo or piercing equipment.
Q: Who should be tested for hepatitis C?
A: The U.S. Preventive Services Task Force recommends all adults aged 18–79 years be screened once. Those with ongoing risk factors should be tested more frequently.
Q: Can hepatitis C be cured?
A: Yes. Modern direct-acting antiviral medications can eliminate the virus in the vast majority of cases with appropriate treatment, significantly reducing complication risks and improving long-term outcomes.
Q: What happens if hepatitis C is not treated?
A: Untreated hepatitis C may lead to progressive liver disease, cirrhosis, liver failure, and liver cancer. Early detection and treatment are paramount to preventing serious complications.
Key Takeaways for Prevention and Screening
- Practice safe injection behaviors and avoid sharing personal items that might come in contact with blood.
- Be cautious with tattoos and piercings; use only reputable facilities with sterile equipment.
- Ensure safe sex practices, particularly for populations at higher risk.
- Get screened if you fall into any of the risk categories or as per routine recommended adult screening guidelines.
- Seek medical guidance if you suspect exposure or have a diagnosis of hepatitis C—early intervention can prevent severe outcomes and offer a high chance of cure.
Conclusion
Hepatitis C, though often silent in the initial years, can have devastating consequences if left unchecked. Participate in regular health screenings, remain informed about risk factors, and adopt measures to minimize transmission. Advancements in antiviral treatments offer hope, with most chronic hepatitis C cases now curable if detected and treated appropriately.
References
- https://www.mayoclinic.org/diseases-conditions/hepatitis-c/symptoms-causes/syc-20354278
- https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/hepatitis-c-testing-could-save-your-life
- https://newsnetwork.mayoclinic.org/discussion/mayo-clinic-q-and-a-understanding-hepatitis-c/
- https://www.mayoclinic.org/diseases-conditions/hepatitis-c/expert-answers/hepatitis-c/faq-20058533
- https://www.mayoclinic.org/diseases-conditions/hepatitis-c/diagnosis-treatment/drc-20354284
- https://www.youtube.com/watch?v=hbUOnMSyd0g
- https://newsnetwork.mayoclinic.org/discussion/mayo-clinic-minute-what-is-hepatitis-c/
- https://www.amerikanhastanesi.org/mayo-clinic-care-network/mayo-clinic-health-information-library/diseases-conditions/hepatitis-c
- https://www.mayoclinic.org/tests-procedures/hepatitis-c-antibody-test/about/pac-20588681
Read full bio of medha deb












