Hemorrhoids: Symptoms, Causes, Diagnosis, and Treatment
Understand hemorrhoids — types, symptoms, causes, prevention, diagnosis, and treatments for comfortable relief and care.
Hemorrhoids
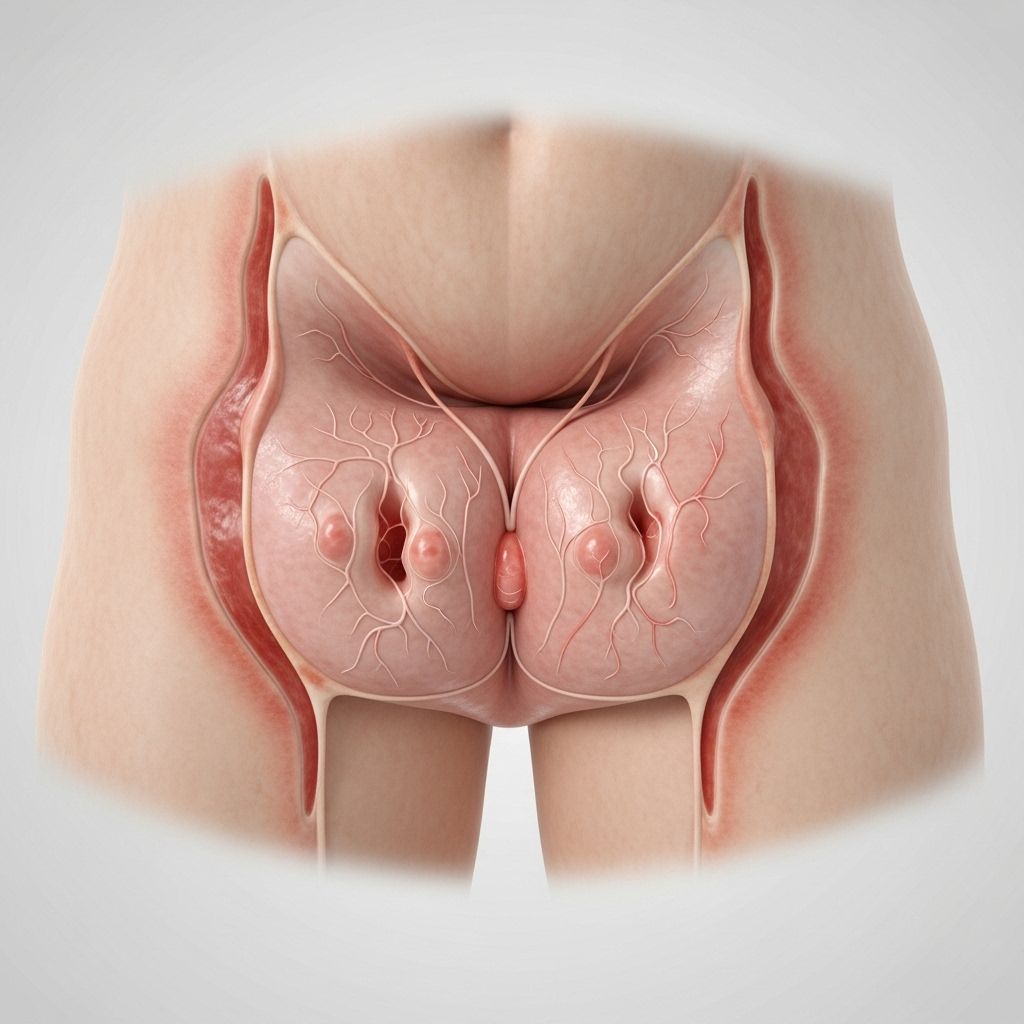
Hemorrhoids, sometimes called piles, are swollen veins in the lowest part of the rectum and anus, similar to varicose veins elsewhere. These veins can stretch and bulge, leading to irritation and uncomfortable symptoms, particularly during bowel movements. While hemorrhoids are common and usually not life-threatening, they can cause significant discomfort and distress.
What are Hemorrhoids?
Hemorrhoids are one of the most common causes of rectal bleeding. They affect about 1 in 20 people in the United States, and over half of people over 50 will experience them at some point in their lives.
Most cases resolve on their own or with simple treatments, but severe cases may require medical intervention.
- Internal hemorrhoids: Located inside the rectum; typically painless but can cause bleeding.
- External hemorrhoids: Develop under the skin around the anus; known for pain and swelling.
- Prolapsed hemorrhoids: Internal hemorrhoids that slip outside the anus.
- Thrombosed hemorrhoids: External hemorrhoids where blood clots cause severe pain, swelling, and bluish discoloration.
Hemorrhoid Symptoms
- Bleeding during bowel movements (bright red blood on toilet paper or in the toilet bowl)
- Itching and irritation in the anal region
- Pain or discomfort around the anus
- Swelling or a lump near the anus
- Mucus discharge or a feeling of fullness in the rectum
What Causes Hemorrhoids?
Several factors increase the likelihood of developing hemorrhoids:
- Straining during bowel movements
- Chronic constipation or diarrhea
- Sitting for long periods on the toilet
- A low-fiber diet
- Obesity
- Pregnancy and childbirth
- Aging
- Family history of hemorrhoids
- Heavy lifting or other activities increasing pressure on the rectal veins
Where Do Hemorrhoids Occur?
| Type | Location | Main Symptoms |
|---|---|---|
| Internal | Inside rectum | Painless bleeding, possible prolapse |
| External | Under skin around anus | Pain, swelling, itching |
| Thrombosed | External hemorrhoid with blood clot | Severe pain, swelling, bluish color |
| Prolapsed | Internal hemorrhoid protruding outside anus | Discomfort, visible lump |
How Common Are Hemorrhoids?
Hemorrhoids are very common, particularly in older adults. They affect over half of people fifty years and older and are frequently encountered in primary care, gastroenterology, and colorectal surgery.
Types and Grades of Hemorrhoids
Internal Hemorrhoids
These occur inside the rectum and are often painless because the area has few pain-sensing nerves. Symptoms may include painless rectal bleeding, a sense of fullness, and occasional prolapse (internal hemorrhoid protrudes outside the anus).
Grades of Internal Hemorrhoids (Goligher’s Classification)
- Grade I: Bleed but do not prolapse.
- Grade II: Prolapse during straining but reduce spontaneously.
- Grade III: Prolapse and require manual reduction.
- Grade IV: Prolapsed and cannot be reduced; may be thrombosed.
External Hemorrhoids
This type forms under the skin around the anus. They contain many pain-sensing nerves and can be very uncomfortable, especially if they become thrombosed (form a clot).
Prolapsed Hemorrhoids
These are internal hemorrhoids that become so enlarged that they protrude outside the anus. Depending on severity, they may retract on their own or require manual replacement.
Thrombosed Hemorrhoids
When a blood clot forms in an external hemorrhoid, it becomes thrombosed, appearing as a hard lump and causing significant pain, swelling, and irritation.
Hemorrhoid Complications
- Persistent bleeding, leading to anemia in rare cases
- Severe pain, often from thrombosed hemorrhoids
- Mucus discharge or irritation causing itching
- Difficulty with hygiene due to prolapsed or swollen tissues
- Necrosis or ulceration with untreated, severe cases
Prevention: How Can I Prevent Hemorrhoids?
- Eat a high-fiber diet (fruits, vegetables, whole grains)
- Drink plenty of water
- Avoid straining during bowel movements
- Exercise regularly to maintain bowel health and prevent constipation
- Don’t sit on the toilet too long
- Avoid reading or using a phone in the bathroom which increases sitting time
- Manage chronic diarrhea or constipation with medical guidance
Diagnosing Hemorrhoids
Diagnosis depends on clinical symptoms and physical examination. Often, external hemorrhoids are visible to a healthcare provider.
- External hemorrhoids: Usually detected by direct visual exam
- Internal hemorrhoids: May require a digital rectal exam (gloved finger) or instruments like an anoscope, proctoscope, or sigmoidoscope
- Colonoscopy: Might be needed if there are signs of other diseases (e.g., colorectal cancer) or if a colon exam hasn’t been done recently
Diagnosis helps rule out more serious causes of rectal bleeding such as colon polyps, colorectal cancer, or inflammatory bowel disease.
Hemorrhoid Treatment Options
Home Remedies
- Eat fiber-rich foods (whole grains, vegetables, fruits)
- Take fiber supplements (if advised)
- Drink more fluids to soften stools
- Take warm sitz baths several times a day to relieve symptoms
- Apply topical creams, ointments, or suppositories (e.g., hydrocortisone cream, witch hazel)
- Avoid straining during bowel movements
Medical and Minimally Invasive Treatments
- Non-surgical medical procedures:
- Injection sclerotherapy (chemical injection to shrink hemorrhoid)
- Rubber band ligation (a rubber band cuts off blood supply; hemorrhoid falls off)
- Infrared coagulation (uses infrared light to clot hemorrhoidal blood vessels)
- Surgical procedures:
- Hemorrhoidectomy (removal of hemorrhoids)
- Stapled hemorrhoidopexy (using a special stapling device to remove and reposition hemorrhoidal tissue)
- Laser therapy (directs laser beam to shrink hemorrhoid)
Most treatments are effective in reducing symptoms. Selection depends on severity, grade, and response to initial therapies. Surgery is usually reserved for severe cases that do not respond to other treatments.
Grades and Recommended Treatment Options
| Grade | Main Features | Treatment Options |
|---|---|---|
| Grade I | Bleeding, no prolapse | Diet, medication, sclerotherapy, rubber band ligation, infrared coagulation |
| Grade II | Prolapse with straining, returns spontaneously | Rubber band ligation, sclerotherapy, infrared coagulation |
| Grade III | Prolapse, requires manual reduction | Minimally invasive surgery, rubber band ligation, laser removal |
| Grade IV | Irreducible prolapse/thrombosis | Surgical removal, advanced procedures |
Living with Hemorrhoids
For many, hemorrhoid symptoms are mild and manageable with good self-care. Chronic or severe hemorrhoids, however, may require medical treatment to restore comfort and avoid complications.
- Maintain a balanced and fiber-rich diet
- Stay hydrated
- Develop healthy bathroom habits (don’t delay bowel movements, avoid straining)
- Keep the anal area clean with gentle wipes after bowel movements
- Monitor for persistent symptoms (seek medical help if pain, bleeding, or lumps don’t improve)
Frequently Asked Questions (FAQs)
Q: Are hemorrhoids dangerous or life-threatening?
A: Typically, hemorrhoids are not dangerous but they can cause significant discomfort and complications if untreated. Persistent bleeding should always be evaluated by a medical professional.
Q: Do hemorrhoids always require surgery?
A: Most hemorrhoids resolve with lifestyle modifications or simple medical treatments. Surgery is reserved for severe, persistent, or complicated cases.
Q: Can hemorrhoids be prevented?
A: Prevention includes eating a high-fiber diet, staying hydrated, exercising regularly, and avoiding prolonged straining during bowel movements.
Q: How do I know if I have hemorrhoids or something else?
A: Common symptoms (pain, bleeding, swelling, itching) suggest hemorrhoids, but similar symptoms occur in other rectal conditions. A healthcare provider can diagnose hemorrhoids through an exam.
Q: How long do hemorrhoids take to heal?
A: Mild cases can resolve within a few days to a couple of weeks if managed well. Persistent symptoms should be assessed by a professional.
Q: Can internal hemorrhoids cause bleeding?
A: Yes, internal hemorrhoids often cause bright red, painless bleeding during bowel movements. However, other serious causes of rectal bleeding should be ruled out.
Tips for Healthy Digestion and Hemorrhoid Prevention
- Eat regular meals rich in fiber
- Drink at least 6-8 cups of water daily
- Engage in moderate physical activity most days of the week
- Respond promptly to the urge to have a bowel movement
- Avoid overuse of laxatives which may worsen constipation and hemorrhoids
- Practice proper hygiene; choose gentle, fragrance-free products for cleaning the anal area
- Follow medical advice if hemorrhoid symptoms persist
References
- https://www.ibilasertherapy.com/four-grades-of-hemorrhoids/
- https://www.webmd.com/digestive-disorders/understanding-hemorrhoids-basics
- https://www.mayoclinic.org/diseases-conditions/hemorrhoids/diagnosis-treatment/drc-20360280
- https://www.georgiahae.com/what-are-hemorrhoids/internal-hemorrhoids/
- https://www.aapc.com/blog/93132-a-simple-fix-for-internal-hemorrhoids/
- https://prodiadigital.com/en/articles/hemorrhoid-treatment
Read full bio of Sneha Tete












