Hemodialysis for Advanced Chronic Kidney Disease: A Comprehensive Guide
Learn how hemodialysis works, who needs it, what to expect, risks, costs, and frequently asked questions.
nn
Hemodialysis is a medical treatment that replaces the waste-filtering function of the kidneys for people with advanced chronic kidney disease (CKD). When kidneys can no longer effectively filter excess fluids, waste, and toxins from the blood, hemodialysis becomes a crucial, often life-saving intervention. This comprehensive guide explains how hemodialysis works, who needs it, what to expect, potential risks, preparation steps, costs, and answers to commonly asked questions.
nn
Understanding Chronic Kidney Disease and Hemodialysis
nn
Chronic kidney disease affects more than 1 in 7 adults in the United States. The kidneys’ primary job is to remove waste and excess fluids from the blood by producing urine. Over time, various conditions—such as diabetes, high blood pressure, or genetic disorders—can damage kidney tissue, impairing these vital functions. When kidney function drops below 15% of normal, waste products and fluid can quickly build up to dangerous levels in the body.
nn
- n
- CKD is progressive — the damage often happens over years, with early symptoms mild or absent.
- Common signs as the disease advances include fatigue, swelling in the legs or around the eyes, muscle cramps, poor appetite, and trouble concentrating.
- People with late-stage CKD typically require treatment to filter their blood: hemodialysis, peritoneal dialysis, or a kidney transplant.
n
n
n
nn
How Does Hemodialysis Work?
nn
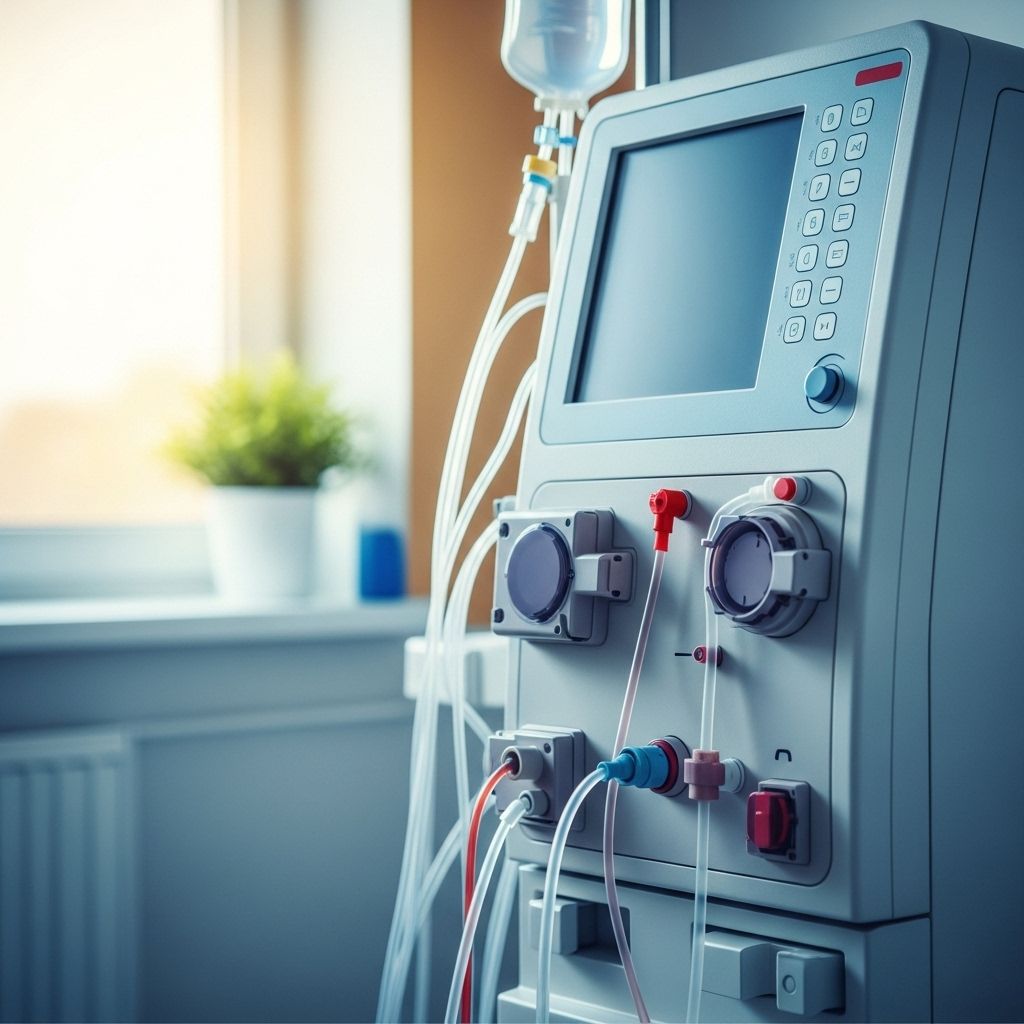
Hemodialysis serves as an artificial kidney for individuals with advanced CKD. The process uses a special filter called a hemodialyzer to remove excess fluids, toxins, and wastes from the blood. A machine draws blood from the patient, passes it through the filter, and then returns the cleaned blood to the body.
nn
Main Functions of Hemodialysis
n
- n
- Removes waste products (like urea and creatinine)
- Eliminates extra fluid from the blood
- Helps regulate essential electrolytes such as potassium, sodium, and calcium
- Aids in controlling blood pressure
n
n
n
n
nn
Dialysis is not a cure; rather, it replaces the kidneys’ vital role, allowing people with advanced kidney disease to manage symptoms and maintain their health.
nn
Who Needs Hemodialysis: Indications for Treatment
nn
Hemodialysis is recommended for individuals whose kidneys are functioning poorly or not at all—most often, people with stage 5 CKD, also known as end-stage renal disease (ESRD). Treatment may be considered if you have:
nn
- n
- Severe loss of kidney function (typically below 10–15% of normal)
- Severe symptoms of kidney failure, such as persistent vomiting, loss of appetite, severe itching, or swelling
- Dangerous electrolyte imbalances (e.g., high potassium levels)
- Volume overload that doesn’t respond to medication
n
n
n
n
nn
Your doctor will assess your kidney health using blood tests, urine tests, and assessment of symptoms to determine when dialysis is necessary. The timing and approach can be individualized based on your overall health, preferences, and lifestyle.
nn
Hemodialysis vs. Conservative Management
nn
While most people with advanced kidney failure begin dialysis, it’s important to understand that not everyone benefits equally. Conservative management is an alternative for some individuals, particularly those who are elderly, have significant additional health problems, or wish to focus on symptom relief and quality of life rather than prolonging life by dialysis.
nn
According to recent research, people who choose conservative care—meaning careful symptom management without dialysis—may experience fewer hospitalizations than those who undergo dialysis. Patients aged over 80, those with advanced liver disease, severe disabilities, or limited self-care ability often do not see a survival benefit from starting dialysis, and may even have a higher risk of hospitalization and complications than with conservative care alone.
nn
Preparation for Hemodialysis
nn
Preparing for hemodialysis involves several steps, often starting weeks or months before the first session. The key preparation is establishing an access point for the dialysis machine to remove and return blood efficiently. The three main types of vascular access are:
nn
- n
- Arteriovenous (AV) Fistula: Surgically connects an artery and a vein, typically in your arm. The preferred, most durable option.
- AV Graft: Uses a synthetic tube to connect an artery and vein if your blood vessels are unsuitable for a fistula.
- Central Venous Catheter: A temporary tube inserted into a vein in the neck, chest, or groin, usually for urgent or short-term dialysis.
n
n
n
nn
Early planning for access surgery is critical—fistulas, for example, may take weeks to months to mature. Your healthcare team will give you instructions on how to care for your access site and prepare for your initial dialysis treatment.
nn
What to Expect When Starting Hemodialysis
nn
Although each patient’s experience is unique, most follow a standardized schedule for treatment, which can be performed in various settings:
nn
- n
- Dialysis center (outpatient clinic): The most common setting, with trained staff supervising your care. Sessions typically last 3–4 hours and occur three times per week.
- Hospital: Used if you have unstable health or require close monitoring.
- At home: With adequate training, some people can complete dialysis at home. Schedules are more flexible—people may do shorter, more frequent sessions (3–7 times per week) on their own timetable.
n
n
n
nn
Your doctor or care team will customize your schedule, considering your health, preferences, and support system.
nn
During Each Treatment
n
- n
- Vital signs—like blood pressure and heart rate—are closely monitored during every dialysis session.
- Mild side effects are possible, including abdominal cramping or nausea.
- Most people pass the time watching TV, reading, working on a laptop, or listening to music.
n
n
n
nn
Hemodialysis Procedure: Step-by-Step
nn
Each hemodialysis session follows a similar process:
nn
- n
- A healthcare provider cleans the access site and inserts two specialized needles: one withdraws blood, another returns filtered blood back to your body.
- Your blood flows through tubing into the hemodialyzer, a filter that removes excess fluids, wastes, and balanced electrolytes.
- Cleansed blood is returned through the second needle or catheter.
- Throughout the session, the team monitors your blood pressure and overall comfort.
- After the treatment, needles are removed, and bleeding is stopped.
n
n
n
n
n
nn
Results and Effectiveness of Hemodialysis
nn
Hemodialysis can be highly effective at managing the symptoms and dangers of kidney failure:
nn
- n
- Reduces buildup of toxins and fluid
- Helps control blood pressure and electrolyte imbalances
- Improves appetite, energy, and overall well-being
n
n
n
nn
However, it is not a cure. Most people will need regular dialysis treatments indefinitely unless they are eligible for a kidney transplant. The effectiveness also depends on attending all sessions, adhering to diet/fluid restrictions, and caring for your dialysis access.
nn
Living Between Hemodialysis Treatments
nn
Managing your health between dialysis sessions is essential for optimal outcomes.
nn
Key Aspects of At-Home Care
n
- n
- Diet: Restrict sodium, potassium, phosphorus, and excess fluids as recommended.
- Medication: Take all prescriptions exactly as directed, including medicines for blood pressure, anemia, or preventing bone disease.
- Access care: Keep your access site clean and monitor for swelling, redness, or pain to prevent infection or clotting.
- Activity: You may feel tired after sessions but can maintain a typical, active lifestyle as tolerated between treatments.
- Symptom monitoring: Report shortness of breath, fever, chest pain, or excessive swelling to your care team promptly.
n
n
n
n
n
nn
Risks and Side Effects of Hemodialysis
nn
While hemodialysis is generally safe and life-extending, it comes with potential risks and side effects:
nn
- n
- Low blood pressure (hypotension) during or after treatment
- Muscle cramps
- Nausea and vomiting
- Fatigue or weakness, especially after sessions
- Blood clotting or infection at the access site
- Anemia (low red blood cell count)
- Skin itching or dryness
- Poor appetite or nutritional deficiencies
n
n
n
n
n
n
n
n
nn
Close medical follow-up and reporting any new or concerning symptoms will help your care team adjust your treatment and address issues early.
nn
Potential Long-Term Complications
nn
| Complication | Description |
|---|---|
| Access failure | Blockage, infection, or clotting of fistula, graft, or catheter |
| Cardiovascular stress | Fluctuations in blood pressure, risk of heart strain |
| Bone disease | Problems with calcium and phosphorus management affecting bone strength |
| Electrolyte imbalance | Difficulties keeping potassium, sodium, or phosphorus at safe levels |
| Malnutrition | Nutrient loss and appetite problems can cause weight loss, weakness |
nn
Cost of Hemodialysis
nn
The expense of hemodialysis can be significant, with costs varying based on treatment site, insurance coverage, and frequency:
nn
- n
- In the United States, Medicare typically covers dialysis for people with end-stage kidney disease, regardless of age.
- Private insurance and Medicaid may also help with costs.
- Additional expenses—such as prescription medications, travel to dialysis centers, and lost work time—should be considered By patients and families.
n
n
n
nn
Consult your treatment team to understand your financial coverage and resources. Social workers are often available to guide you to appropriate support programs.
nn
Alternatives to Hemodialysis
nn
While hemodialysis is the most commonly used type, other options exist:
nn
- n
- Peritoneal dialysis: Involves filtering blood via the lining of your abdomen. It can be done at home, offering more flexibility, but suitability varies by individual.
- Kidney Transplant: Surgical replacement of failed kidneys with a healthy kidney from a donor. This is often the preferred long-term solution, but not all patients are candidates, and donor organs may not be immediately available.
- Conservative care: Focuses on symptom control and quality of life without dialysis or transplant, as described above.
n
n
n
nn
Frequently Asked Questions (FAQs)
nn
References
- https://www.healthline.com/health/kidney-disease/hemodialysis-for-advanced-disease
- https://www.healthline.com/health-news/advanced-kidney-disease-why-dialysis-may-not-always-be-the-best-treatment
- https://www.youtube.com/watch?v=6L2oOUl3dJ8
- https://hlic.net/what-is-hemodialysis/
- https://www.healthline.com/health/video/ckd-stages
- https://californiahealthline.org/news/listening-to-older-patients-who-want-to-stop-dialysis/
- https://hlic.net/what-is-dialysis/
- https://www.youtube.com/watch?v=7JF-55DGDbQ
- https://aakp.org/programs-and-events/aakp-healthline/
- https://www.medicalnewstoday.com/articles/172179
- https://www.healthline.com/health/kidney-disease/hemodialysis-for-advanced-disease
- https://www.healthline.com/health-news/advanced-kidney-disease-why-dialysis-may-not-always-be-the-best-treatment
- https://www.youtube.com/watch?v=6L2oOUl3dJ8
- https://hlic.net/what-is-hemodialysis/
- https://www.healthline.com/health/video/ckd-stages
- https://californiahealthline.org/news/listening-to-older-patients-who-want-to-stop-dialysis/
- https://hlic.net/what-is-dialysis/
- https://www.youtube.com/watch?v=7JF-55DGDbQ
- https://aakp.org/programs-and-events/aakp-healthline/
- https://www.medicalnewstoday.com/articles/172179
Read full bio of Sneha Tete












