Helicobacter pylori: Infection, Symptoms, Treatment, and Prevention
Understand the causes, symptoms, complications, and treatment of Helicobacter pylori infections and how to prevent them.
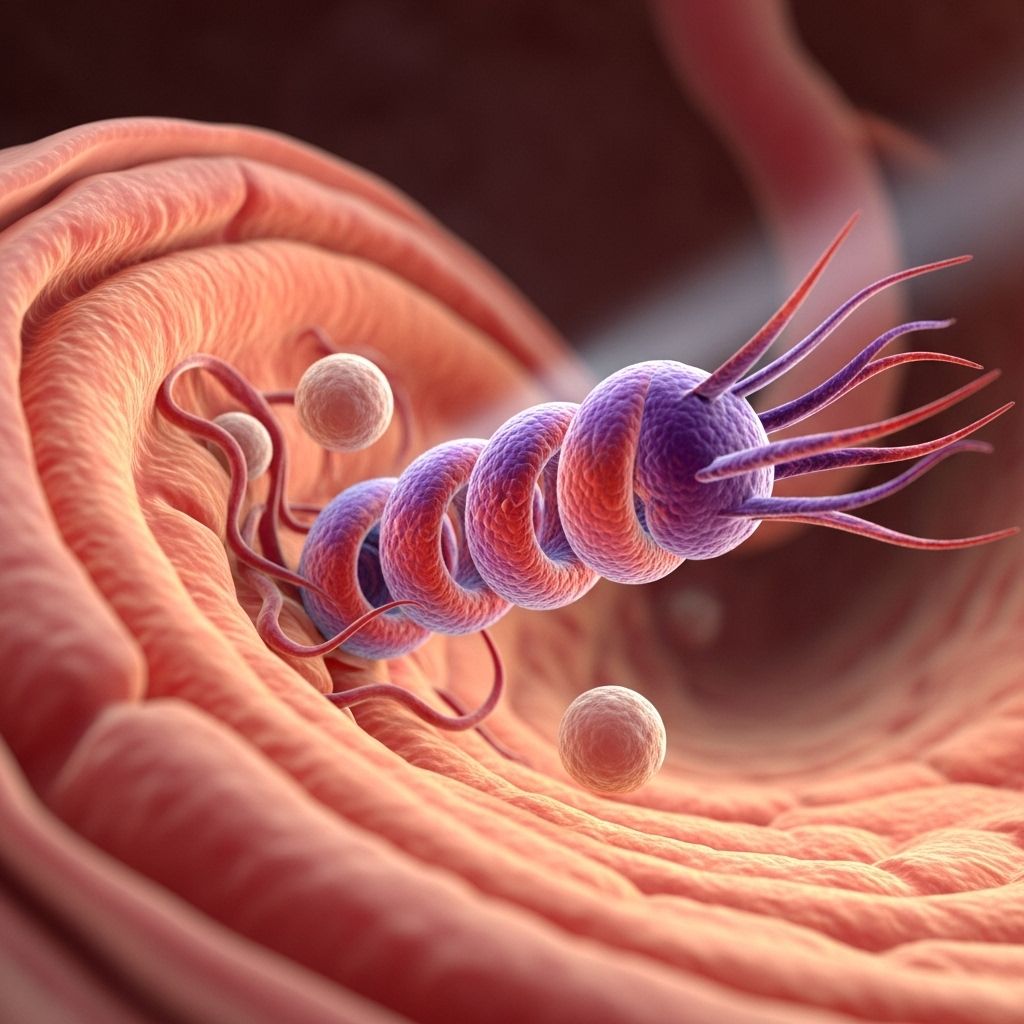
Helicobacter pylori (H. pylori) is a type of bacteria that infects the stomach and affects more than half the world’s population at some point in their lives. Although most infections occur in childhood and many people show no symptoms, H. pylori remains a major cause of gastritis, peptic ulcers, and can contribute to the risk of stomach cancer. Understanding its transmission, associated health effects, diagnosis, and management is essential for maintaining digestive health.
Overview of Helicobacter pylori Infection
H. pylori is a spiral-shaped, gram-negative bacterium adapted to live in the harsh, acidic environment of the stomach. Once established, its unique mechanisms enable it to evade the immune system, causing inflammation and damage to the stomach lining. These bacteria spread predominantly through person-to-person contact and, less commonly, via contaminated food or water. The infection is especially prevalent in developing regions, with socioeconomic, sanitary, and age-related factors influencing its transmission rate.
- Prevalence: Over 50% of global population infected at some point
- Age-related trend: More common in older adults and in populations in developing countries
- Transmission: Via body fluids (saliva, vomit, stool), poor hand hygiene, contaminated food/water
Causes & Risk Factors
| Risk Factor | Description |
|---|---|
| Poor sanitation/hygiene | Exposure to contaminated food, water, and objects |
| Living conditions | Overcrowded environments or shared living spaces |
| Geographic region | Developing countries have higher prevalence rates |
| Family history | Close contact with infected individuals increases risk |
| Age | More common in older adults |
Symptoms of Helicobacter pylori Infection
Most people infected with H. pylori remain asymptomatic. When symptoms do develop, they are often related to gastritis or peptic ulcer disease due to inflammation or erosion of the stomach or duodenal lining.
- Ache or burning pain in the upper abdomen (may worsen with an empty stomach)
- Bloating and frequent burping
- Nausea or vomiting
- Loss of appetite and unexplained weight loss
- Indigestion or heartburn
- In severe cases: Stool that is dark or tarry (a sign of gastrointestinal bleeding)
It is important to note that severe symptoms like vomiting blood, black-tarry stools, or acute abdominal pain may signal a complication and require immediate medical attention.
Clinical Complications Associated with H. pylori
- Chronic Gastritis: Persistent inflammation of the stomach lining
- Peptic Ulcers: Open sores in the lining of the stomach or duodenum
- Gastric Cancer: Long-term infection increases risk, though relatively rare
- Mucosa-Associated Lymphoid Tissue (MALT) Lymphoma: Uncommon, but associated with chronic infection
How H. pylori Bacteria Cause Disease
H. pylori attach to the gastric epithelial cells and induce an inflammatory response. The bacteria secrete enzymes and toxins (such as urease, which neutralizes stomach acids), weakening the protective mucus layer. This process makes the lining more susceptible to acid, leading to tissue damage, ulcers, and chronic inflammation. Prolonged infection may result in cellular changes that increase cancer risk.
Who Should Be Tested For H. pylori?
Testing for H. pylori is recommended for individuals who present with:
- Symptoms of peptic ulcers or unexplained stomach pain
- Persistent gastritis or chronic indigestion
- History of gastric cancer or strong family history
- Unexplained iron-deficiency anemia or vitamin B12 deficiency
Diagnosis of H. pylori Infection
Several methods are used to detect H. pylori infection. Physicians select diagnostic tests based on clinical presentation, patient age, availability, and the likelihood of complications.
- Non-invasive tests:
- Urea breath test: Measures breakdown of urea by H. pylori urease
- Stool antigen test: Detects H. pylori proteins in feces
- Blood antibody tests: Less commonly used, may indicate prior rather than current infection
Knowing how H. pylori is diagnosed can empower you during your healthcare journey. For a closer look at the diagnostic procedures, including endoscopic techniques and what to expect during these evaluations, explore our comprehensive guide on endoscopy for stomach ulcers. This information can help prepare you for your medical consultations. - Invasive tests:
- Endoscopy with gastric biopsy: Allows direct visualization and sampling for histology, rapid urease testing, and culture
- Cultures: Performed after treatment failure or in research settings
Treatment Options for H. pylori Infection
Eradicating H. pylori requires a combination of medications due to the bacteria’s adaptability and resistance patterns. The main objective is to clear the infection, heal ulcers, and reduce the risk of complications.
Standard Treatment Regimens
- Triple Therapy:
- Two antibiotics (commonly amoxicillin, clarithromycin, metronidazole, or tetracycline)
- Plus a proton pump inhibitor (PPI) to reduce stomach acid and promote healing
- Bismuth Quadruple Therapy:
- Bismuth subsalicylate, two antibiotics, and a PPI
- Often used as second-line treatment or in areas of high antibiotic resistance
- Alternative therapies:
- In special cases, rifabutin-based triple therapy or clarithromycin triple therapy
- Histamine (H-2) blockers when PPIs are contraindicated
| Medication Type | Examples |
|---|---|
| Antibiotics | Amoxicillin, Clarithromycin, Metronidazole, Tetracycline, Tinidazole, Rifabutin |
| Proton pump inhibitors (PPIs) | Omeprazole, Esomeprazole, Lansoprazole, Pantoprazole, Rabeprazole |
| Bismuth compounds | Bismuth subsalicylate |
| Histamine (H-2) blockers | Cimetidine, Nizatidine (only if PPIs are unsuitable) |
Antimicrobial resistance is an increasing concern. Resistance rates for metronidazole and clarithromycin can be significant (up to 39% and 24% in certain populations), requiring appropriate antibiotic selection based on regional data and history of prior treatments.
Follow-up Care After Treatment
- Symptom reassessment and confirmation of eradication (typically with a urea breath test or stool antigen test several weeks after completing therapy)
- Management of remaining or recurrent symptoms with further diagnostic testing as indicated
Preventing H. pylori Infection
Though it’s difficult to completely prevent infection, certain measures help reduce the risk of transmission:
- Wash hands thoroughly with soap and water, especially after using the toilet and before eating
- Avoid sharing food, drinks, or utensils with others
- Eat only foods that are properly prepared and drink safe, clean water
- Practice good kitchen hygiene when handling raw foods
Public health strategies, including improving sanitation and access to clean water, play a critical role in lowering infection rates globally.
Living With H. pylori and Long-term Outcomes
For most individuals, successfully treated H. pylori infections lead to symptom resolution and a decreased risk of ulcer recurrence. Ongoing digestive issues should prompt follow-up care. Those who remain untreated risk chronic gastritis, ulcer development, and—over years—potential progression to serious stomach diseases, including cancer.
Frequently Asked Questions (FAQs)
Q: Is H. pylori contagious?
A: Yes, H. pylori can spread through person-to-person contact via saliva, vomit, stool, and contaminated food or water.
Q: What foods should be avoided if I have H. pylori?
A: There is no specific diet required for H. pylori; however, avoiding spicy, fatty, or acidic foods may reduce stomach irritation. Focus on eating balanced, easily digestible meals and maintaining good nutrition.
Q: How is H. pylori diagnosed?
A: Diagnosis involves non-invasive tests like the urea breath test and stool antigen test, or invasive endoscopic methods if complications are suspected.
Q: Are ulcers always caused by H. pylori?
A: While H. pylori is the leading cause of peptic ulcers, ulcers can also result from non-steroidal anti-inflammatory drug (NSAID) use and other medical conditions.
Q: Can I get reinfected after treatment?
A: Reinfection is possible, especially if exposed to contaminated food, water, or close contact with infected individuals, but in many developed regions it is uncommon.
Q: Is H. pylori linked to cancer?
A: Chronic H. pylori infection increases the risk of developing gastric cancer, though such progression is rare and usually found in people with long-standing, untreated inflammation.
When to See a Doctor
- Unexplained, persistent stomach pain
- Symptoms suggesting a peptic ulcer (burning abdominal pain, especially between meals or at night)
- Blood in vomit or stool (which may appear black or tarry)
- Unintentional weight loss or persistent loss of appetite
If you experience any of these symptoms or have concerns regarding your digestive health, seek medical evaluation promptly for appropriate diagnosis and management.
Summary Table: Key Facts about H. pylori Infection
| Feature | Detail |
|---|---|
| Bacteria type | Gram-negative, spiral-shaped |
| Main complications | Chronic gastritis, peptic ulcers, gastric cancer (rare) |
| Symptoms | Stomach pain, bloating, burping, nausea, vomiting, weight loss |
| Diagnosis | Urea breath test, stool antigen test, endoscopic biopsy |
| Treatment | Combination antibiotics & proton pump inhibitors |
| Prevention | Hand hygiene, safe food/water, avoid sharing utensils |
References
- This article is synthesized and rephrased based on authoritative health sources including Johns Hopkins Medicine, Mayo Clinic, WebMD, and peer-reviewed literature.
References
- https://www.mayoclinic.org/diseases-conditions/h-pylori/symptoms-causes/syc-20356171
- https://www.hopkinsguides.com/hopkins/view/Johns_Hopkins_ABX_Guide/540252/all/Helicobacter_pylori
- https://pure.johnshopkins.edu/en/publications/the-role-of-helicobacter-pylori-in-the-pathogenesis-of-acid-pepti-3
- https://www.webmd.com/digestive-disorders/h-pylori-helicobacter-pylori
- https://zerotb.jhmi.edu/projects/h-pylori/
- https://pure.johnshopkins.edu/en/publications/treatment-of-helicobacter-pylori-infection-3
Read full bio of Sneha Tete












