Heart Valve Repair or Replacement Surgery: Procedures, Risks, and Recovery
A comprehensive guide to heart valve repair and replacement surgery, including when it's needed, surgical options, risks, and recovery expectations.
Heart Valve Repair or Replacement Surgery
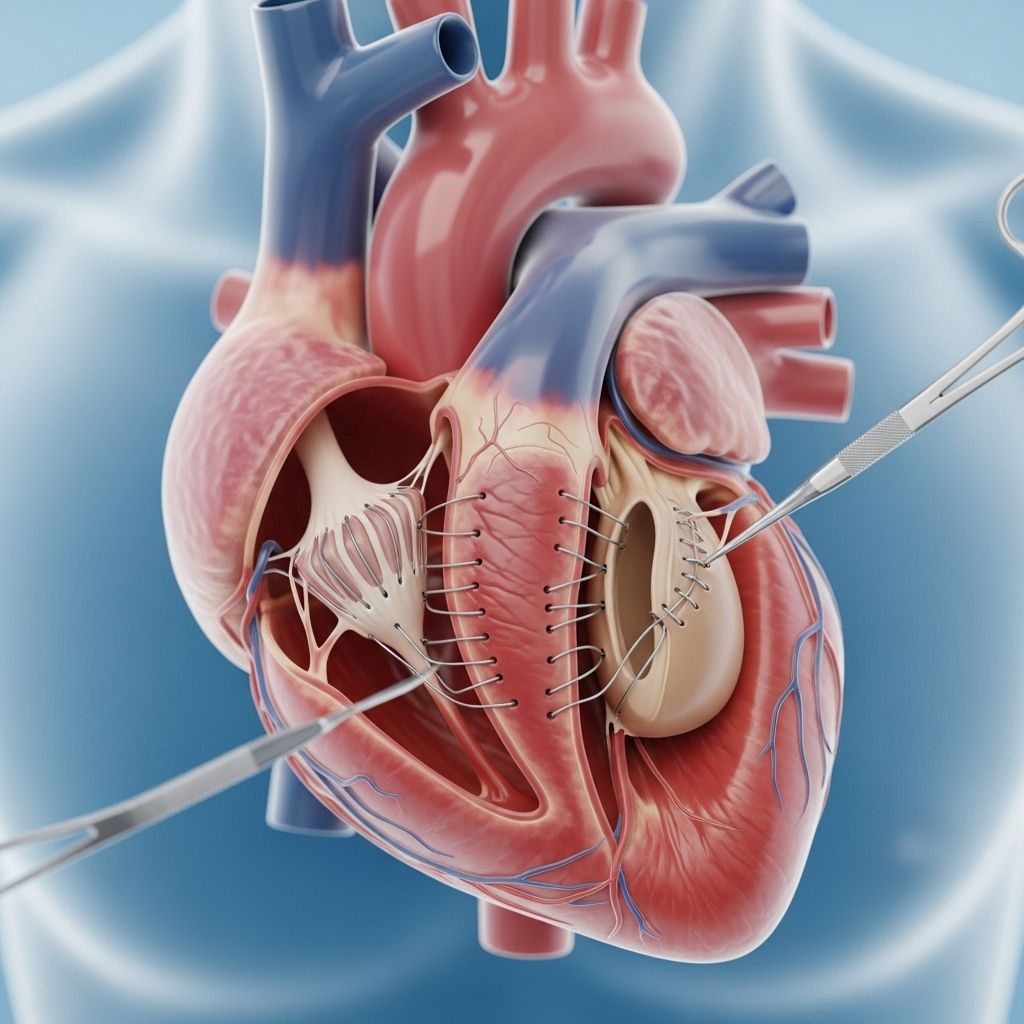
Heart valve repair or replacement surgery is a life-saving procedure for individuals suffering from heart valve disease. The heart’s four valves—mitral, aortic, tricuspid, and pulmonary—direct blood flow in and out of the heart. When these valves are diseased or damaged, they may not open or close properly, leading to serious complications. This article provides a thorough overview of the reasons for surgery, types of procedures, expected risks, what happens before, during, and after surgery, and frequently asked questions about heart valve repair or replacement.
What Is Heart Valve Repair or Replacement Surgery?
Heart valve surgery involves repairing or replacing one or more of the heart’s valves to ensure normal blood flow direction through the heart. Surgery is often recommended when valves do not open fully (stenosis) or do not close completely (regurgitation or insufficiency), leading to symptoms such as fatigue, shortness of breath, or heart failure.
- Repair: The valve is surgically corrected to function properly.
- Replacement: The diseased valve is removed and replaced with an artificial or biological valve.
When Is Heart Valve Surgery Needed?
Heart valve surgery is required when one or more of the heart’s valves are not functioning adequately. The most common reasons a patient might need surgery include:
- Valve Stenosis: The valve is narrowed, making it difficult for blood to flow through.
- Valve Regurgitation or Insufficiency: The valve does not close tightly, allowing blood to flow backward.
- Symptoms associated with valve dysfunction, such as:
- Shortness of breath
- Chest pain
- Edema (swelling in legs or abdomen)
- Palpitations
- Fatigue
- Dizziness or fainting
- Evidence of heart damage (found during echocardiograms or other tests), even if symptoms are mild or absent.
Surgery may also be recommended based on the specific valve affected, the patient’s age, overall health, and likelihood of complications from untreated valve problems.
Types of Heart Valve Surgery
Heart Valve Repair Surgery
Repairing a valve is generally preferable, as it preserves the patient’s own tissue, reduces the need for long-term anticoagulation, and lowers infection risk. Several repair techniques are available:
- Annuloplasty: Reshaping or reinforcing the ring around a valve, often using a ring device.
- Valvuloplasty: A balloon catheter is used to open a stiff (stenotic) valve, commonly performed for mitral or aortic stenosis.
- Commissurotomy: Surgical separation of fused valve leaflets to widen the valve opening.
- Leaflet Reshaping/Repair: Removing or modifying sections of a valve leaflet that are not functioning properly.
- Decalcification: Removing calcium build-up from valves.
- Chordal Transfer/Replacement: Repairing or replacing supporting chordae tendineae (tendinous cords attaching the valve leaflets to heart muscle).
Heart Valve Replacement Surgery
When a valve cannot be repaired due to extensive damage or deformation, replacement is necessary. There are two major types of replacement valves:
- Mechanical valves: Made from durable materials such as metal or carbon. They last many years but require lifelong blood-thinning medication (anticoagulants) to prevent clotting.
- Biological (tissue) valves: Made from animal tissue (usually cow or pig), or donated human valves. They may not last as long as mechanical valves but often do not require long-term anticoagulant use.
| Valve Type | Main Features | Typical Use |
|---|---|---|
| Mechanical | Durable; requires anticoagulation | Younger patients, those not contraindicated for anticoagulation |
| Biological (Tissue) | No long-term anticoagulation; less durable | Older patients, those unable to use anticoagulants |
| Allograft (Homograft) | Human donor valve, used in specialized cases | Specific anatomical needs or re-operations |
Minimally Invasive and Catheter-Based Procedures
- Minimally Invasive Valve Surgery: Performed through smaller incisions using special instruments, often between the ribs. This reduces recovery time and risk of complications compared to traditional open-chest surgery.
- Transcatheter Valve Replacement (TAVR/TAVI): A new valve is delivered via a catheter inserted typically through the femoral artery in the groin; commonly used for aortic valve replacement.
- Robotic-Assisted Surgery: Use of surgical robots for greater precision and minimal incisions.
- MitraClip™ and Other Devices: Special devices are used for minimally invasive mitral valve repairs, helpful in patients with high surgical risk.
Preparation for Heart Valve Surgery
To determine the best surgical approach, your medical team will consider several factors:
- Your age and overall health
- The specific valve(s) affected
- The degree of valve dysfunction and impact on heart function
- Presence of other heart conditions, such as coronary artery disease
- Your ability to tolerate blood thinners
- Pulmonary function and other comorbidities
Pre-surgery preparation typically involves:
- Medical evaluation (history and physical examination)
- Cardiac imaging (echocardiogram, MRI, CT scan)
- Blood tests and other laboratory work
- Discussion regarding medications (which medications to pause or continue)
- Instructions on fasting before surgery
- Arranging support for recovery after the hospital stay
What Happens During Heart Valve Surgery?
Although details may vary depending on the procedure, these are typical steps during heart valve repair or replacement:
- Anesthesia: You are given general anesthesia to ensure you are asleep and pain-free.
- Incision: For open-heart surgery, a large incision is made in the chest (sternotomy). Minimally invasive surgery requires much smaller incisions.
- Heart-Lung Machine: The heart is stopped temporarily, and a heart-lung machine takes over circulating the blood.
- Valve Repair or Replacement: The affected valve is repaired, or the diseased valve is removed and replaced.
- Restoration of Blood Flow: The new or repaired valve is tested, any other repairs are made, and the heart is restarted.
- Closing the Incision: Once the surgical work is complete and the heart is stable, the incision is closed with sutures or staples.
- Duration: The average surgery takes several hours, depending on number of valves treated and surgical approach.
- Team: It involves a highly specialized surgical and anesthesiology team and advanced perioperative care.
Risks and Possible Complications
As with any major surgery, heart valve repair or replacement carries specific risks. The likelihood of complications depends on your health, age, and the extent of the surgery. Notable risks include:
- Infection
- Bleeding
- Blood clots, which may result in stroke or heart attack
- Valve dysfunction or failure
- Arrhythmias (abnormal heart rhythms)
- Lung, kidney, or other organ dysfunction
- Swelling or bruising around the incision sites
Importantly, the risks must be weighed against the risk of not treating severe valve disease, which has its own serious consequences.
After Surgery: Recovery and Outlook
Hospital Recovery
- Most patients spend a few days in the intensive care unit (ICU) for close monitoring, then move to a standard hospital room.
- Breathing tubes and IV lines are removed as soon as it is medically safe.
- Pain is managed with medication, and you will begin gentle movement soon after surgery to prevent blood clots and improve recovery.
Home Recovery
- Most people can resume daily activities within 4-8 weeks after traditional open surgery, and sooner after minimally invasive or catheter-based procedures.
- You may be prescribed cardiac rehabilitation, a supervised program to gradually increase your activity and monitor recovery.
- Follow all instructions regarding incision care, wound signs, diet, and medications.
- Take blood thinners as directed if you have a mechanical valve, and keep all follow-up appointments with your cardiology and surgical teams.
Long-term outcomes are generally excellent. Most patients feel stronger, more energetic, and have a significant reduction in symptoms. However, lifelong medical follow-up is necessary to monitor valve function and adjust care as needed.
Living with a New or Repaired Heart Valve
Whether you receive a repaired or replaced valve, a few changes and careful monitoring are essential for your health:
- Anticoagulation: If you have a mechanical valve, you will take warfarin or other blood thinners for life.
- Monitoring: Regular checkups and periodic echocardiograms will be needed to assess the function of your valve(s).
- Infection Prevention: Antibiotics may be required before certain dental or surgical procedures to prevent endocarditis (heart infection).
- Healthy Lifestyle: Maintain heart health by eating a healthy diet, exercising within advised limits, not smoking, and managing other health conditions like diabetes or hypertension.
Frequently Asked Questions (FAQs)
Q: What types of heart valves can be repaired or replaced?
A: All four heart valves can be repaired or replaced: mitral, aortic, tricuspid, and pulmonary. The mitral and aortic valves are most commonly affected by valve disease and are the most frequently repaired or replaced.
Q: What are the signs I might need heart valve surgery?
A: Common signs are shortness of breath, chest pain, fainting, palpitations, fatigue, swelling in the ankles or legs, or symptoms of heart failure. Some candidates for surgery may have no symptoms, but tests show damage or dysfunction of the heart valves.
Q: How do mechanical and tissue (biological) valves differ?
A: Mechanical valves are highly durable and last for decades but require lifelong blood thinners. Biological valves mimic natural valves and may not require ongoing blood thinners, but they last 10–20 years on average and may need replacement in the future.
Q: What is a minimally invasive heart valve surgery?
A: Minimally invasive procedures use small incisions (instead of a large chest incision) and specialized tools, often leading to faster recovery and fewer complications. Examples include TAVR and MitraClip™ repairs.
Q: How soon can I return to normal activities after heart valve surgery?
A: Recovery depends on the type of surgery. After open surgery, people can usually resume most normal activities in 6 to 8 weeks. After minimally invasive or catheter-based surgery, recovery may be as short as 2 to 4 weeks, though driving and strenuous activity should only resume with doctor approval.
Q: Are there alternative treatments to valve surgery?
A: In early or mild valve disease, medications and close monitoring may suffice. For advanced disease, surgery or minimally invasive interventions remain the gold standard.
Key Points to Remember
- Heart valve repair is preferred over replacement when possible.
- Several surgical and minimally invasive techniques are available, tailored to patient needs.
- Risks are present but are outweighed by the benefits of correcting severe valve disease.
- Recovery involves time in the hospital and ongoing care, but most people experience substantial improvement in symptoms and quality of life.
- Continuing care and regular medical follow-up are essential after surgery.
References
- https://www.loyolamedicine.org/services/cardiothoracic-surgery/cardiothoracic-surgery-treatments/heart-valve-replacement-surgery
- https://www.ahn.org/services/cardiovascular/treatments/heart-valve-surgery
- https://medschool.cuanschutz.edu/surgery/divisions-centers-affiliates/cardiothoracic/patient-care/heart-valve-repair-replacement
- https://www.heart.org/en/health-topics/heart-valve-problems-and-disease/understanding-your-heart-valve-treatment-options/options-for-heart-valve-repair
- https://www.brighamandwomens.org/heart-and-vascular-center/resources/heart-valve-repair
- https://my.clevelandclinic.org/health/treatments/17089-heart-valve-surgery
- https://www.franciscanhealth.org/conditions-and-services/heart-care/valve-replacement-surgery
- https://www.umms.org/sjmc/health-services/heart-care/surgery/valve-surgery
Read full bio of Sneha Tete