Heart Valve Blockage Treatment: Approaches, Options, and Care
Learn about heart valve blockages, symptoms, causes, and the treatment strategies available—from medications to advanced surgery.
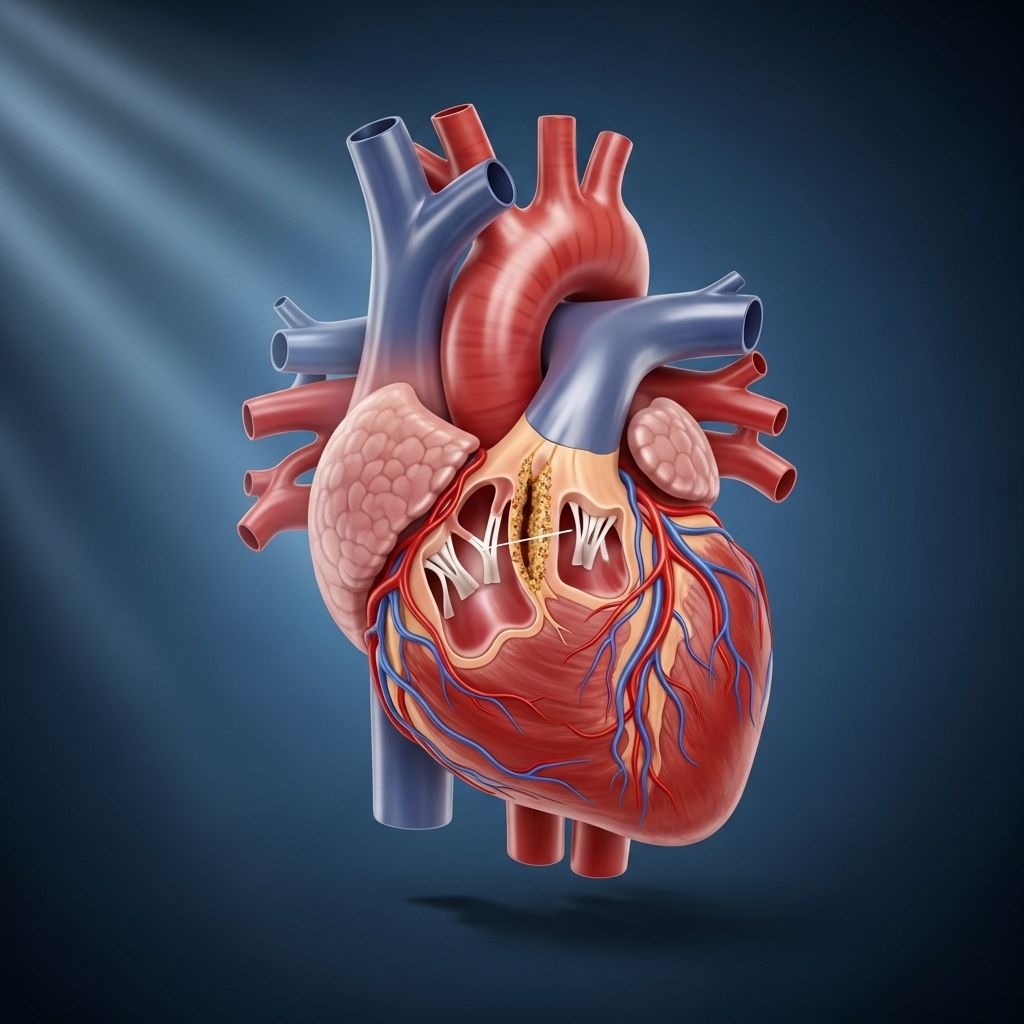
Heart valve blockages represent a serious disruption in the cardiovascular system, restricting the normal flow of blood through the heart’s chambers and to the rest of the body. Blockages may result from several forms of valve disease, such as regurgitation, stenosis, or atresia, each with distinct features and consequences. Timely diagnosis and treatment are essential to prevent complications, enhance heart function, and improve quality of life.
Why Is Treatment Needed for Heart Valve Blockage?
Normal heart function relies on the seamless movement of blood from chamber to chamber, regulated by valves that prevent backflow. If a valve malfunctions or is blocked, not enough blood moves forward, risking leakage (backward flow), inefficient circulation, and severe symptoms. Left untreated, heart valve blockages may lead to:
- Heart failure
- Arrhythmias (irregular heartbeats)
- Stroke
- Organ damage due to poor blood supply
Prompt intervention is critical when symptoms of blockage — such as fatigue, shortness of breath, or chest pain — emerge or worsen.
What Types of Heart Valve Blockage Need Treatment?
Heart valve disorders are categorized by how they impact valve function. These include:
- Regurgitation: Occurs when a valve doesn’t close properly, causing blood to leak backward. The mitral valve is especially susceptible to this problem, which may present with bulging or flapping (prolapse).
- Stenosis: Results from thickened, stiff, or fused valve flaps, which impede full opening and restrict blood flow. Aortic stenosis is a common and serious form, affecting circulation to the body’s largest artery.
- Atresia: Most often congenital, this is when a valve forms without an opening, blocking blood passage entirely. Atresia requires immediate medical assessment after birth.
Symptoms of Heart Valve Blockage
Symptoms may vary in severity and onset, depending on the type and progression of blockages. Common signs to watch for include:
- Fatigue
- Shortness of breath—especially during exertion
- Swelling in ankles, feet, or abdomen
- Chest pain or pressure
- Palpitations
- Fainting (syncope)
Consult your doctor if these symptoms are persistent or worsening, as early treatment can prevent complications.
Causes of Heart Valve Blockage
A heart valve blockage can stem from multiple underlying factors:
- Congenital defects: Problems present at birth, including atresia or malformed valves.
- Age-related changes: Valves may thicken, stiffen, or calcify over time.
- Rheumatic heart disease: Resulting from untreated streptococcal infections leading to valve scarring.
- Endocarditis: Infection of the inner heart lining, potentially damaging valve tissue.
- Degenerative disease: Natural wear and tear causes valve deterioration.
- Other medical conditions: Such as connective tissue disorders or previous heart attacks.
Treatment for Heart Valve Blockage
Treatment varies depending on the type, severity, and progression of valve disease. Therapeutic approaches include:
Medications
Medications are often used to manage symptoms, prevent complications, or improve heart function while preparing for surgery. Key drug classes include:
- Beta-blockers: Reduce heart rate and the workload on the heart.
- Diuretics: Lessen fluid buildup, reducing blood pressure and heart stress.
- Vasodilators: Relax blood vessels to further lower blood pressure.
- Antiarrhythmics: Control abnormal heart rhythms.
- Blood thinners (anticoagulants): Prevent clot formation, especially with atrial fibrillation or valve disease.
- Antibiotics: Used preventatively for those at risk of endocarditis during invasive procedures.
- Prostaglandins: In infants, maintain blood flow pathways in critical congenital cases.
While medications can alleviate symptoms and reduce risk, they do not cure structural valve blockages. They are typically used as supportive therapy.
Surgical Options
Surgery is often the definitive treatment for structural blockages or severe valve malfunction. The main types are:
- Valve Repair: Preferred when feasible, as it preserves native tissue and generally carries fewer risks. Repairs may involve:
- Patching holes in the valve
- Separating fused flaps
- Repairing or replacing supportive structures
- Reshaping or reducing valve tissue for better closure
- Valve Replacement: Necessary if repair is not possible. Replacement valves might be:
- Biologic (from pig, cow, or human tissue)
- Mechanical (made of durable materials)
- Minimally Invasive Procedures: For some, transcatheter replacements (TAVR/TAVI) offer effective treatment without open-heart surgery. Most often used to address aortic stenosis or mitral regurgitation, these procedures use a catheter to insert a new valve, leaving the old valve in place.
- Annuloplasty: Tightening or reinforcing the valve’s outer ring, often performed with other repairs.
- Valvuloplasty: Uses a balloon catheter to widen a stenotic (narrowed) valve. The balloon inflates to stretch the valve open, then is removed.
| Feature | Valve Repair | Valve Replacement |
|---|---|---|
| Preserves native valve | Yes | No |
| Risk of long-term blood thinners | Lower | May be needed (especially mechanical valves) |
| Durability | May require repeat procedures | Biologic: ~10-20 years; Mechanical: long term |
| Suitability | Preferred when possible | Used if repair isn’t feasible |
Can Heart Valve Blockages Be Treated Without Surgery?
In mild or early stages, medications and lifestyle adjustments may be sufficient to manage symptoms and delay progression. However, severe blockages, atresia, and advanced stenosis generally require surgical correction for lasting improvement.
Non-surgical strategies include:
- Lifestyle modifications: Heart-healthy diet, regular exercise (as advised), smoking cessation, and blood pressure management
- Routine monitoring: Echocardiograms and follow-ups to track disease progression
Sometimes less invasive procedures, such as catheter-based valvuloplasty, can relieve symptoms temporarily. Your doctor will tailor the approach to your diagnosis, overall health, and surgical risk.
Prevention of Heart Valve Blockages
While some causes of valve blockages are congenital or age-related, certain steps can reduce risk and protect your heart health:
- Treat strep throat promptly to avoid rheumatic fever and valve scarring
- Practice good oral hygiene and visit the dentist regularly
- Manage chronic diseases such as hypertension and diabetes
- Engage in regular, moderate exercise approved by your doctor
- Avoid tobacco products
- Follow a heart-healthy diet, rich in fruits, vegetables, and whole grains
- Attend routine heart check-ups especially if you’re at higher risk
Frequently Asked Questions (FAQs)
Can heart valve blockages be treated with medications only?
Medications can ease symptoms and lower complication risk, but they do not correct severe structural blockages. Surgery is usually required for significant stenosis, regurgitation, and atresia.
What is a transcatheter valve replacement (TAVR or TAVI)?
This minimally invasive procedure is for select patients with aortic stenosis or mitral regurgitation. A new valve is inserted via a catheter into the groin artery, without removing the failed valve. Recovery is typically faster than with open-heart surgery.
How do I know if I need heart valve surgery?
Surgery may be advised if you have severe symptoms, worsening valve function, or risk complications like heart failure—even if you feel well. Regular cardiac evaluations guide treatment timing.
Are valve repairs safer than replacements?
Valve repair, when possible, preserves natural tissue and often carries fewer long-term risks. However, replacement may be necessary for severely damaged or malfunctioning valves.
Can children have heart valve blockage?
Yes. Some blockages, especially atresia, are congenital and can affect newborns or children. Pediatric cardiac specialists provide tailored treatment options, which may include surgery or prostaglandin medications to ensure blood flow.
Takeaway: Individualized Treatment and Ongoing Care
Heart valve blockages require prompt medical attention and an individualized treatment approach. While medications can manage symptoms and minimize complications, surgery is the mainstay for lasting correction in moderate to severe cases. Regular follow-up, lifestyle adjustments, and prevention strategies can optimize outcomes and help you live a full, active life following treatment.
References
- https://www.mayoclinic.org/diseases-conditions/heart-valve-disease/diagnosis-treatment/drc-20353732
- https://www.healthline.com/health/heart/heart-valve-blockage-treatment
- https://www.healthline.com/health/heart-valve-disease-treatment-without-surgery
- https://medlineplus.gov/heartvalvediseases.html
- https://my.clevelandclinic.org/health/diseases/17639-what-you-need-to-know-heart-valve-disease
- https://www.webmd.com/heart-disease/heart-valve-disease
- https://www.nhlbi.nih.gov/health/heart-valve-diseases/treatment
- https://www.medicalnewstoday.com/articles/237191
- https://www.cedars-sinai.org/newsroom/healthline-therapy-vs-antidepressants–which-is-best-for-people-with-heart-disease/
- https://www.heart.org/en/health-topics/heart-attack/treatment-of-a-heart-attack
Read full bio of medha deb












