Heart Perfusion Scan: Purpose, Procedure, and What to Expect
Explore the uses, preparation, risks, and process of a heart perfusion scan to understand your cardiac health and treatment options.
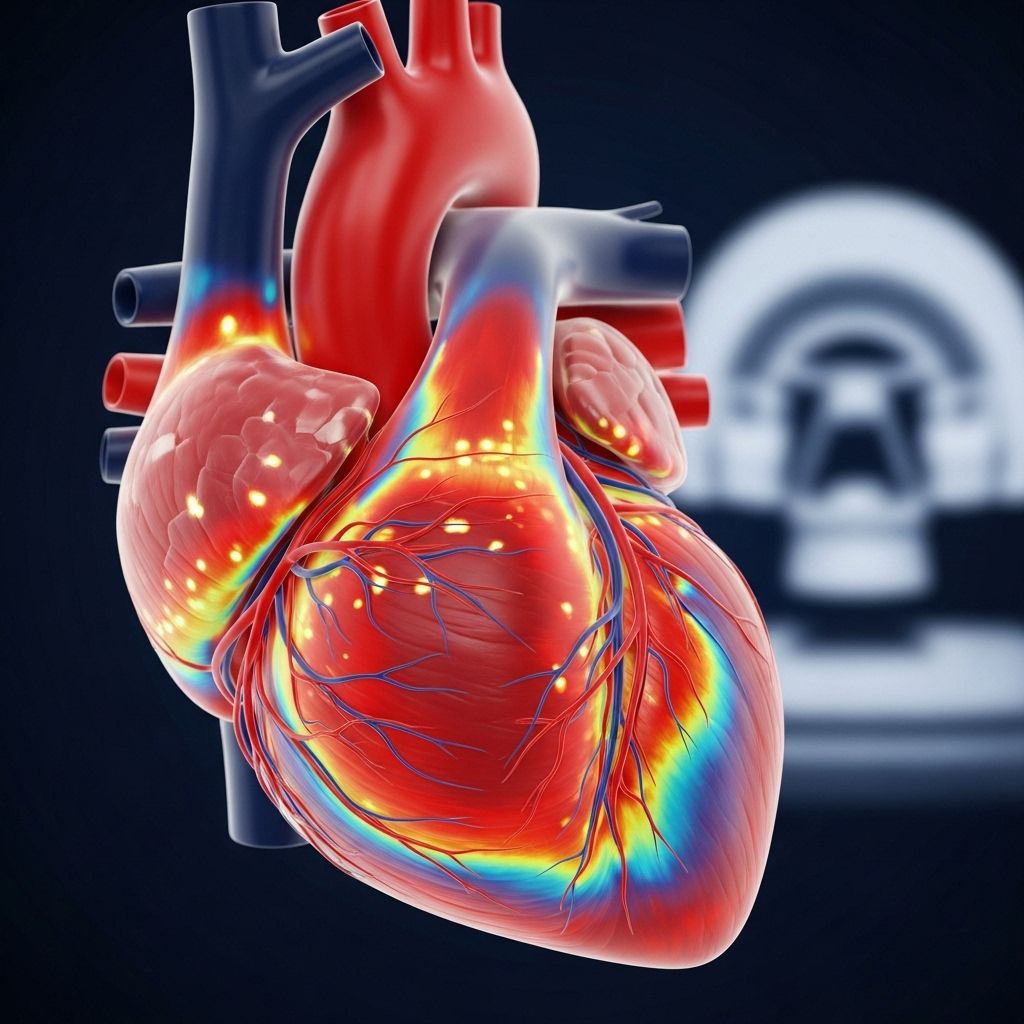
A heart perfusion scan, also known as myocardial perfusion imaging (MPI), is a specialized noninvasive test that provides vital insights into your heart’s blood flow and performance. Doctors often use this test to help diagnose heart conditions, guide treatment, and monitor recovery after cardiac events. Understanding each step—from preparation to results—can help you feel more confident and informed about your cardiac health journey.
What Is a Heart Perfusion Scan?
A heart perfusion scan is an imaging test that measures the flow of blood through the heart muscle (myocardium). It helps determine how effectively your heart is pumping and whether all regions of the heart are receiving enough blood. A radioactive tracer is injected into your bloodstream, allowing specialized cameras to capture detailed images of your heart at rest and/or during stress.
- Also called: Myocardial perfusion scan or scan, SPECT scan, PET scan.
- Diagnostic purpose: Spotting areas with poor blood flow, identifying damage after a heart attack, and evaluating the effectiveness of treatments.
- Type of procedure: Noninvasive, with radioactive tracer injection and external imaging (no incisions).
Why Do Doctors Use a Heart Perfusion Scan?
Your doctor may recommend a heart perfusion scan for several reasons. These include diagnosing heart problems, assessing their severity, guiding treatment, and monitoring progress over time.
Common Reasons for a Heart Perfusion Scan
- Evaluating chest pain: To check if chest pain (angina) is due to poor blood flow from conditions like coronary artery disease (CAD).
- Diagnosing coronary artery disease: Determining the presence, extent, and severity of blockages or narrowing in the heart’s arteries.
- Identifying ischemia: Discovering areas of the heart muscle that aren’t getting enough blood during stress or activity.
- Assessing damage after a heart attack: Mapping injured heart muscle or scarring, which helps with long-term recovery planning.
- Evaluating treatment effectiveness: Checking if coronary interventions like stenting or bypass surgery are restoring blood flow.
- Preoperative evaluation: Assessing cardiac risk before major surgery or invasive procedures, especially for those at higher risk of heart complications.
- Monitoring chronic heart conditions: Keeping track of disease progression or response to ongoing treatment in people with known heart diseases.
How Does a Heart Perfusion Scan Work?
At the core of a heart perfusion scan is the use of radioactive tracers and specialized imaging equipment. These components work together to reveal blockages, reduced blood supply, and heart muscle damage.
Imaging Techniques Used
- SPECT (Single Photon Emission Computed Tomography): Uses tracers like thallium-201 or technetium-99m. A gamma camera rotates around the body to build cross-sectional images.
- PET (Positron Emission Tomography): Uses different radiotracers and detectors, offering high sensitivity but is less commonly used for perfusion scans overall due to availability.
Role of Radioactive Tracer
A radioactive tracer (like technetium or thallium) is injected into your bloodstream. As your blood circulates, this tracer travels to your heart muscle. Areas with healthy blood flow absorb the tracer well and appear “bright” on the images. Regions with reduced blood flow absorb less tracer, appearing “dim” or “cold.”
Stress and Rest Phases
The scan is typically done in two parts:
- Resting scan: Images are captured while your body is at rest.
- Stress scan: Images are captured after your heart is ‘stressed’—either by exercise (treadmill or stationary bike) or by medications that simulate the effect of exercise in those unable to exert themselves.
Comparing rest and stress images helps your doctor find areas of the heart muscle that only struggle during activity (reversible ischemia) or are always affected (scar or infarct).
Who Needs a Heart Perfusion Scan?
This scan is recommended for people with, or suspected of having, heart problems, and those with risk factors for coronary artery disease. You may be a candidate for this test if you have:
- Unexplained chest pain or shortness of breath
- Established coronary artery disease
- History of heart attack or cardiac interventions (bypass, stent)
- Risks factors: diabetes, hypertension, high cholesterol, family history of heart disease
- Scheduled for major surgery (as part of preoperative assessment)
How Do You Prepare for a Heart Perfusion Scan?
Proper preparation helps ensure accurate results and your comfort during the procedure. Your healthcare team will give you clear instructions tailored to your specific test.
Common Preparation Guidelines
- Medication review: Inform your doctor about all your medications, including over-the-counter drugs and supplements. You may need to stop certain medications (like beta-blockers and calcium channel blockers) before the scan, as directed by your doctor.
- Dietary restrictions: Avoid food, caffeine, and nicotine for at least 4 hours—or as instructed—prior to the test. These substances can affect your heart’s response during the scan.
- Appropriate clothing: Wear comfortable, loose-fitting clothes and suitable footwear, especially if you’ll be exercising.
- Special considerations: Inform your healthcare provider about asthma, COPD, allergies, or pregnancy prior to the procedure.
Always follow any specific instructions from your care team, as preparation can vary depending on your health and the center’s protocol.
What Happens During a Heart Perfusion Scan?
The scan takes a few hours in total but is done in stages. Here’s what to expect at each step:
1. Arrival and Check-In
- Your personal information, vital signs, and medical history will be reviewed.
2. Resting Phase
- A radioactive tracer is injected through a vein in your arm.
- You rest quietly for a set period to allow the tracer to circulate.
- Images of your heart at rest are captured by a gamma camera. This requires lying still with your arms above your head for several minutes.
3. Stress Phase
- You are either asked to exercise (usually on a treadmill or bike), or given medication that increases your heart rate or dilates your heart’s blood vessels—simulating physical exertion.
- At the peak of your stress or shortly after, a second dose of tracer may be given.
- Images are captured again, showing your heart during ‘stress.’
Doctors monitor your heart rhythm and blood pressure throughout, ready to stop the test or offer reversal medications if needed.
Understanding the Results
After the scan, a nuclear medicine specialist or cardiologist analyzes your images, looking for areas of normal and abnormal blood flow.
| Parameter | Interpretation |
|---|---|
| Perfusion defect | Site, severity, reversibility, size |
| Global heart function | Normal, mildly to severely reduced |
| Wall motion | Normal, single or multiple regional abnormalities |
| Ischemia | Reversible (seen with stress), or fixed (same at rest and stress, indicating scar tissue) |
| ECG findings | No ischemia, borderline, mild to strong ischemia |
Your doctor will discuss what the scan revealed and what it means for your treatment plan. If abnormalities are detected, further testing or changes in management may be recommended.
Risks and Considerations
Heart perfusion scans are generally safe, but—as with any medical procedure—there are potential risks and side effects to be aware of:
- Tracer risks: Very small risk of allergic reaction to the tracer. Exposure to low levels of radiation, typically considered safe for adults.
- Stress test risks: Rare chances of irregular heartbeat, chest pain, wheezing (especially in people with asthma or COPD), or, in extremely rare cases, heart attack.
- Other complications: Dizziness, nausea, or reactions to medications used during the scan, but these are usually short-lived and managed promptly.
Always tell your doctor about any underlying conditions, especially respiratory issues (asthma, COPD), allergies, or if you are pregnant or breastfeeding.
Recovery and Aftercare
Most people return to their normal activities shortly after the scan. The tracer loses radioactivity quickly and is naturally eliminated in urine and stool. Drinking extra fluids can speed up this process. Your care team may advise you on any specific aftercare if needed.
How Heart Perfusion Scan Results Affect Your Treatment
The results from a heart perfusion scan help guide your medical care. They contribute to decisions about:
- Starting or changing medications
- Planning procedures such as stent placement or bypass surgery
- Assessing recovery after interventions
- Long-term follow-up and prevention strategies
Repeat scans may be needed over time to monitor changes or evaluate the effectiveness of ongoing treatment.
Frequently Asked Questions (FAQs)
Q: Is a heart perfusion scan painful?
A: The scan itself is not painful. You may feel a minor pinch from the injection and potential brief discomfort if you undergo an exercise stress test.
Q: How long does the scan take?
A: The entire process often takes several hours, but the actual imaging time after each tracer injection is typically 15–30 minutes.
Q: Is the radioactive material safe?
A: The amount of radiation is carefully controlled and considered very low—far less than most X-rays or CT scans. Reactions are rare but always inform the staff about allergies and health conditions.
Q: Can I drive myself home after the scan?
A: Most people can drive home after a heart perfusion scan. However, check with your doctor if you experienced any side effects, required sedative medications, or have specific health concerns.
Q: What are the alternatives to a perfusion scan?
A: Other options may include echocardiography, cardiac CT or MRI, or invasive coronary angiography. The choice depends on your health and diagnostic needs.
Key Points to Remember
- A heart perfusion scan offers critical, detailed information about blood flow and heart muscle health.
- It’s a safe, widely used tool to diagnose, monitor, and guide treatment for various heart conditions.
- Preparation, test steps, and potential risks will be explained to you beforehand by your healthcare team.
- Results empower informed decision-making about ongoing cardiac care and risk management.
Takeaway
A heart perfusion scan is a proven, essential diagnostic method for exploring heart health, uncovering hidden risks, and crafting individualized treatment plans. If you have concerns about your heart or are scheduled for an MPI scan, talk openly with your healthcare provider about what to expect and how this test fits into your care.
References
- https://www.medicalnewstoday.com/articles/heart-perfusion-imaging-scan
- https://www.ncbi.nlm.nih.gov/books/NBK539772/
- https://www.healthline.com/health/v-q-mismatch
- https://www.heart.org/en/health-topics/heart-attack/diagnosing-a-heart-attack/myocardial-perfusion-imaging
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3548424/
- https://www.ahajournals.org/doi/10.1161/CIRCIMAGING.120.011984
- https://www.medicalnewstoday.com/articles/265579
Read full bio of Sneha Tete












