Understanding Heart Murmurs and Hypertrophic Cardiomyopathy: Symptoms, Diagnosis, and Management
A comprehensive guide to heart murmurs and hypertrophic cardiomyopathy, from key symptoms and risk factors to diagnosis, treatment, and living well.
Heart Murmur and Hypertrophic Cardiomyopathy: What You Need to Know
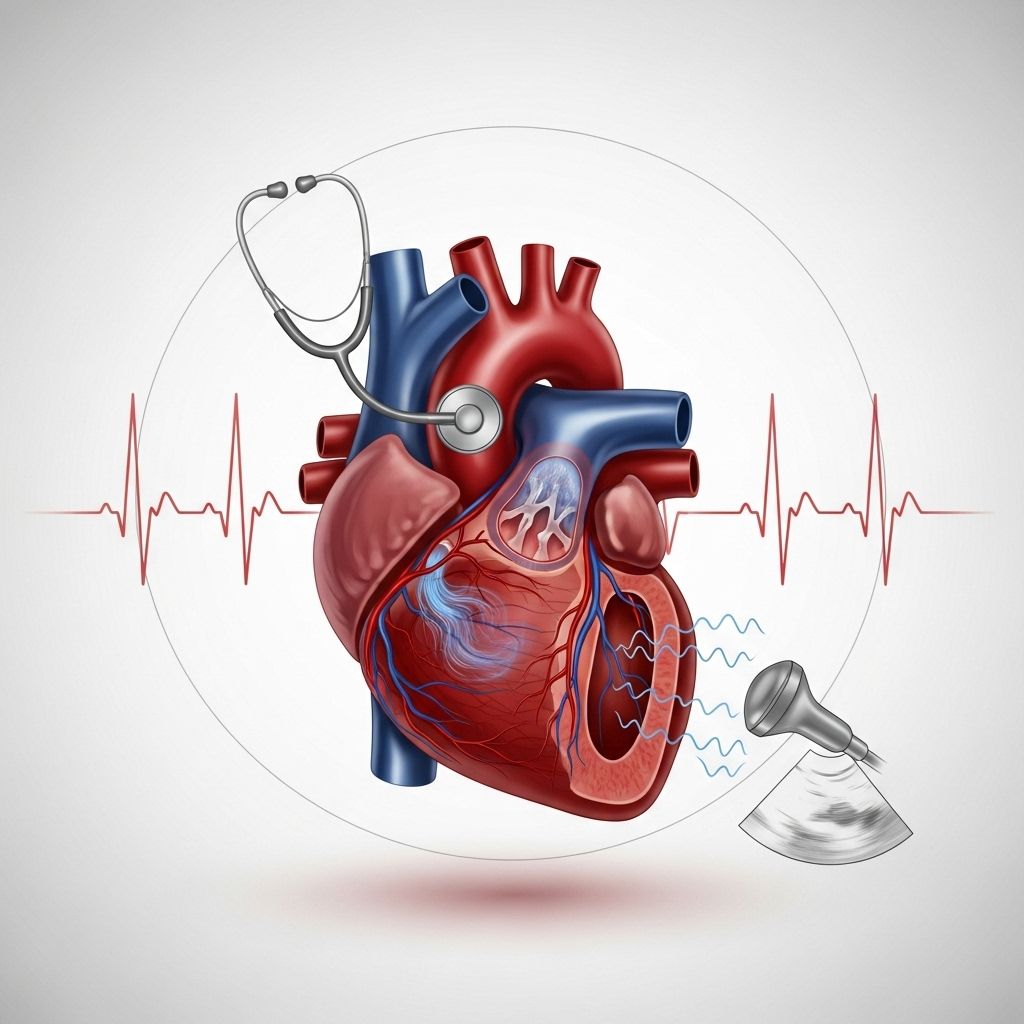
Heart murmurs and hypertrophic cardiomyopathy (HCM) are closely connected conditions that may affect the heart’s structure and function. HCM is a genetic or acquired disease often characterized by the thickening of the heart muscle, most commonly the septum that separates the heart’s left and right chambers. This thickening can give rise to a heart murmur—an unusual sound heard during a heartbeat. Understanding the relationship between murmurs and HCM, as well as the symptoms, diagnostic methods, and treatment options, is essential for early intervention and maintaining heart health.
What Is a Heart Murmur?
A heart murmur is an extra or unusual sound heard during the heartbeat cycle. It is produced by turbulent blood flow within the heart or its surrounding vessels. From a clinical perspective, heart murmurs are not diseases themselves but may signal underlying heart problems, like HCM, valvular abnormalities, or congenital heart defects.
- Some murmurs are harmless (innocent) and cause no health issues.
- Others are abnormal, associated with structural changes or problems, including conditions like HCM.
What Is Hypertrophic Cardiomyopathy?
Hypertrophic cardiomyopathy is a common, often inherited, heart disease. It is marked by the thickening (hypertrophy) of the heart muscle, particularly the muscle wall (septum) between the left and right ventricles.
- The most frequently affected area is the left ventricle, the heart’s primary pumping chamber.
- This thickening can obstruct blood flow and affect the heart’s electrical system.
- HCM is found in about 1 in 500 people and can affect individuals of all ages, often presenting during adolescence or young adulthood but sometimes later.
Many people with HCM experience no symptoms and may not realize they have the condition until it is identified via routine checkup or diagnostic testing. Others develop symptoms that can significantly affect quality of life or even lead to severe complications.
Symptoms of HCM: More Than Just a Murmur
The presentation of HCM varies widely, ranging from being completely asymptomatic to causing severe symptoms and complications. The most common symptoms include:
- Chest pain, especially during exercise or physical exertion
- Shortness of breath, often triggered by activity
- Fatigue and reduced tolerance for exercise
- Palpitations (fluttering, pounding, or irregular heartbeat)
- Fainting or dizziness, particularly with exertion or sudden posture changes
- Heart murmur detected during physical exam
- Swelling in the ankles, feet, legs, abdomen, or neck (less common)
It is important to note that:
- Symptoms may worsen over time and, in some people, lead to limitations in daily activities.
- HCM is a leading cause of sudden cardiac arrest in young athletes, though this outcome is rare.
- Some people never develop symptoms, while others may first experience them in adulthood.
How Heart Murmurs Are Related to HCM
Heart murmurs in HCM usually result from turbulent blood flow caused by the thickened heart walls and/or abnormalities in the mitral valve. The murmur may:
- Be heard best with a stethoscope placed over the left side of the chest.
- Change in intensity or timing with certain maneuvers (e.g., standing, squatting, or the Valsalva maneuver).
- Accompany symptoms like fatigue, palpitations, or dizziness.
Not every murmur means HCM is present. However, a new or unexplained murmur—especially with a family history of heart disease—should always be evaluated to rule out serious causes like hypertrophic cardiomyopathy.
Causes and Risk Factors for HCM
The primary causes and risk factors for HCM include:
- Genetic mutations: Roughly 40% of HCM cases are linked to inherited mutations that affect heart muscle structure and function.
- Family history of HCM or sudden cardiac death increases the risk.
Other possible contributors:
- High blood pressure (especially with age)
- Certain chronic conditions affecting the heart muscle
HCM is diagnosed across all ages but is especially concerning in younger people and athletes due to its association with dangerous arrhythmias.
How Is Hypertrophic Cardiomyopathy Diagnosed?
Accurate diagnosis of HCM begins with a thorough clinical assessment and is confirmed with a combination of tests. Your doctor may recommend the following:
- Physical examination: Listening for heart murmurs or abnormal rhythms via stethoscope.
- Echocardiogram (Echo): The primary test for HCM, it uses ultrasound waves to produce images, measure the thickness of the heart muscle, and assess blood flow.
- Electrocardiogram (ECG or EKG): Records the heart’s electrical signals and helps detect abnormal rhythms or patterns.
- Cardiac MRI: Provides detailed images to assess areas of muscle thickening and overall heart structure.
- Genetic testing: Identifies hereditary forms of HCM, often in conjunction with genetic counseling.
- Stress testing: Assesses how the heart performs during exercise.
- Holter monitor: A wearable device that tracks electrical activity and rhythm over 24-48 hours during daily activity.
- Coronary angiography: Uses X-rays and contrast dye to examine for blockages in the coronary arteries (done in select situations).
Early diagnosis of HCM is crucial, especially with a family history or warning symptoms, as it allows for more effective risk management and monitoring.
Potential Complications of Hypertrophic Cardiomyopathy
HCM is a chronic condition that can lead to the following complications:
- Atrial fibrillation: An irregular and often rapid heart rate, raising the risk of stroke and blood clots.
- Heart failure: Caused when the thickened heart muscle impairs pumping ability.
- Sudden cardiac arrest: Usually due to malignant arrhythmias (life-threatening abnormal rhythms); although rare, it is a primary cause of sudden death in young athletes.
- Valve disease: Thickened muscle can cause the mitral valve to leak (regurgitation), which may worsen symptoms.
When to See a Doctor
Several common yet serious symptoms should prompt immediate medical evaluation:
- Sudden chest pain or discomfort
- Shortness of breath at rest or with activity
- Palpitations
- Fainting spells or lightheadedness—especially during or after exertion
- Any new or unexplained heart murmur
If any of these symptoms are severe or occur suddenly, especially with a family history of cardiac disease or sudden death, call emergency services right away.
Treatment Options for Hypertrophic Cardiomyopathy
Treatment of HCM aims to relieve symptoms, prevent complications, and improve quality of life. A personalized care plan often includes a combination of the following approaches:
1. Medications
- Beta blockers and calcium channel blockers (slow the heart rate and reduce muscle contractility, helping symptoms and blood flow).
- Antiarrhythmic medications for rhythm control.
- Anticoagulants in patients at risk for blood clots (e.g., those with atrial fibrillation).
2. Procedures and Surgical Interventions
- Septal myectomy: Surgical removal of a portion of thickened heart muscle, improving blood flow and reducing symptoms.
- Alcohol septal ablation: Injection of alcohol to destroy part of the septum, reducing obstruction.
- Implantable cardioverter-defibrillator (ICD): For those at high risk of life-threatening arrhythmias or sudden cardiac death.
- Mitral valve repair or replacement: Used if the valve is leaky due to muscle thickening.
3. Lifestyle and Monitoring
- Activity modifications: Avoid intense competitive sports or high-intensity exercise if advised, given higher risk of arrhythmias.
- Regular follow-up with a cardiologist experienced in HCM.
- Heart-healthy diet, avoiding excess salt and alcohol.
- Monitoring and controlling other cardiovascular risk factors (blood pressure, diabetes).
Living with HCM: What Are the Prognosis and Outlook?
For many individuals, HCM is manageable with appropriate treatment and lifestyle adjustments. Most people live normal or near-normal lives, especially when the diagnosis occurs early and symptoms are well controlled.
- Regular follow-up and monitoring are vital, as HCM is a chronic condition that can evolve over time.
- Family members may also need screening or genetic counseling—early identification of inherited HCM can be lifesaving.
Frequently Asked Questions About Heart Murmurs and HCM
What’s the difference between a heart murmur and hypertrophic cardiomyopathy?
A heart murmur is a sound heard with a stethoscope and is not a disease in itself. Hypertrophic cardiomyopathy is a structural heart disease that often causes an abnormal murmur because of turbulent blood flow due to thickened heart walls.
Can you have a heart murmur without having HCM?
Yes. Heart murmurs can be caused by many conditions, some benign (innocent murmurs), others related to different heart valve or structural problems. Only a comprehensive evaluation can determine the cause.
Is HCM always inherited?
No, but HCM often results from genetic changes that can be inherited. About 40% of cases are clearly linked to gene mutations. Even when not inherited, family screening is often recommended if HCM is diagnosed.
What are the warning signs of serious problems with HCM?
Warning signs include fainting, chest pain, shortness of breath during exercise, rapid or irregular heartbeat, and a family history of sudden cardiac death. These signs require prompt evaluation and care.
Do people with HCM need to avoid all sports?
Not necessarily. Many people with HCM can safely participate in low-intensity activities, but competitive and high-intensity sports may be restricted due to the risk of dangerous arrhythmias. Individual recommendations will be based on symptoms, risk assessment, and doctor’s advice.
Prevention and Family Screening
As HCM can be familial, family members of a diagnosed individual are usually advised to undergo screening. This may include:
- Clinical evaluation (medical and family history)
- ECG and echocardiogram
- Genetic counseling and, if appropriate, genetic testing
While HCM itself can’t always be prevented, early detection and management help avoid severe complications and offer the best possible quality of life.
Plan Your Heart Health
If you, a family member, or your child have symptoms such as chest pain, palpitations, a heart murmur, fainting, or a family history of heart problems, see your doctor for early evaluation. With advances in genetic testing, imaging, and cardiac care, people with HCM can live long, active, and fulfilling lives.
FAQs
What causes a heart murmur in hypertrophic cardiomyopathy?
The thickened heart muscle and/or elongated mitral valve found in HCM often cause turbulent blood flow, leading to the characteristic murmur heard during examination.
Is hypertrophic cardiomyopathy life-threatening?
Most people with HCM live normal lives, but some are at risk of dangerous arrhythmias and sudden cardiac arrest, especially if left undiagnosed and untreated. Regular evaluation and management greatly reduce this risk.
What age does HCM usually appear?
It can appear at any age, but symptoms often develop in adolescence or young adulthood. Sometimes, it is not discovered until later in adulthood during routine exams.
Can children develop HCM?
Yes, HCM can affect children, particularly if there is a strong family history. Pediatric screening is important in such cases.
Can HCM be cured?
There is no cure for HCM, but symptoms and risks can be effectively managed with medications, procedures, and lifestyle adaptations based on each individual’s unique situation.
References
- https://www.pennmedicine.org/conditions/hypertrophic-cardiomyopathy
- https://nyulangone.org/conditions/hypertrophic-cardiomyopathy/diagnosis
- https://www.heart.org/en/health-topics/cardiomyopathy/what-is-cardiomyopathy-in-adults/hypertrophic-cardiomyopathy
- https://www.mayoclinic.org/diseases-conditions/hypertrophic-cardiomyopathy/symptoms-causes/syc-20350198
- https://my.clevelandclinic.org/health/diseases/17116-hypertrophic-cardiomyopathy
- https://www.mayoclinic.org/diseases-conditions/hypertrophic-cardiomyopathy/diagnosis-treatment/drc-20350204
- https://www.aafp.org/pubs/afp/issues/2022/0200/p207.html
- https://www.ncbi.nlm.nih.gov/books/NBK430788/
Read full bio of Sneha Tete












