Understanding Heart Failure with Preserved Ejection Fraction (HFpEF)
Exploring causes, diagnosis, symptoms, treatment, and outlook for heart failure with preserved ejection fraction (HFpEF).
Heart Failure with Preserved Ejection Fraction (HFpEF): A Complete Guide
Heart failure with preserved ejection fraction (HFpEF) is a form of heart failure that accounts for roughly 50% of all heart failure cases. Despite its prevalence, HFpEF is complex, often misunderstood, and poses unique challenges for diagnosis and management. This comprehensive guide unpacks the causes, symptoms, diagnostic approach, treatment strategies, and outlook for those affected by HFpEF.
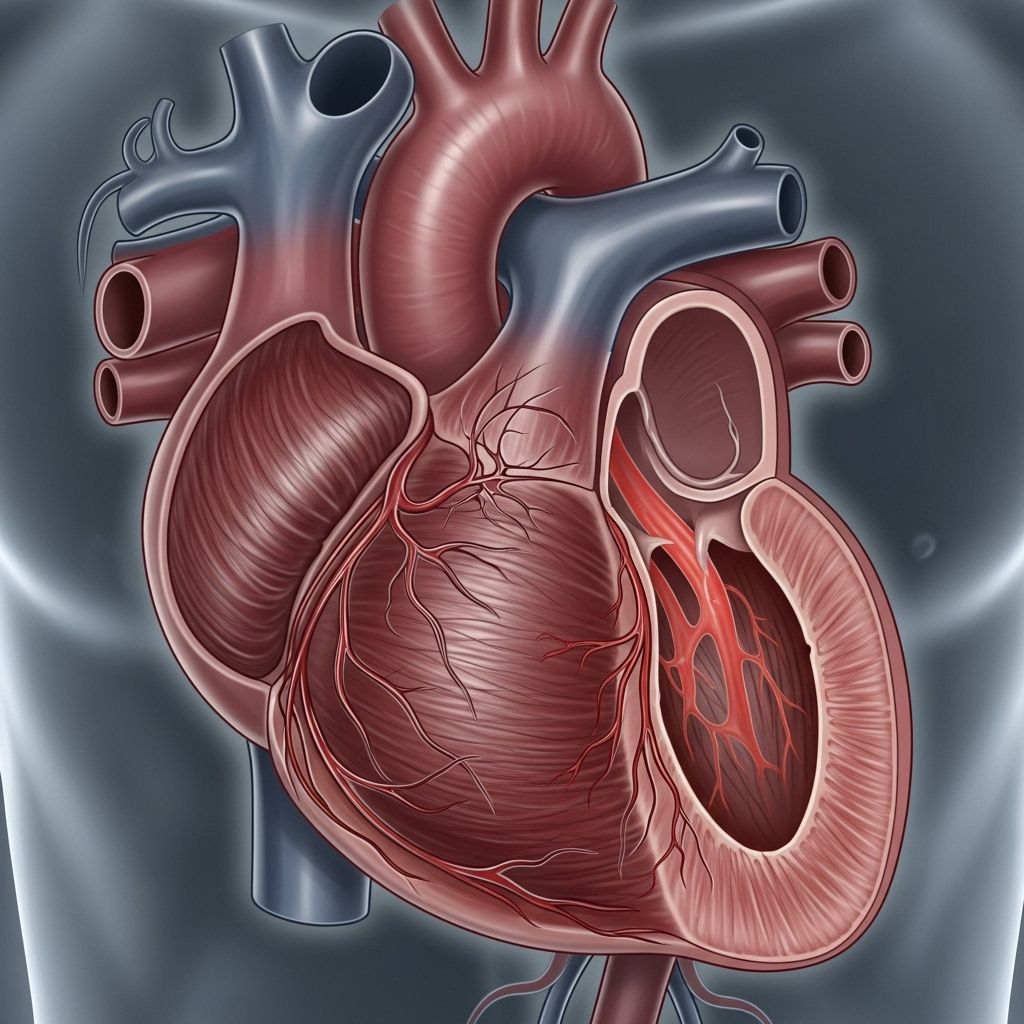
What is Heart Failure with Preserved Ejection Fraction?
Heart failure with preserved ejection fraction (HFpEF) is a condition where the heart muscle loses its ability to relax and fill properly during diastole. Despite this, the heart maintains a normal or near-normal ejection fraction (typically defined as ≥50%), meaning the percentage of blood pumped out of the ventricles with each contraction appears preserved. This distinct profile differentiates HFpEF from heart failure with reduced ejection fraction (HFrEF), where the heart’s pumping ability is markedly diminished.
- Ejection Fraction (EF): Represents the proportion of blood ejected from the heart with each beat. Normal EF is typically 50%-70%.
- HFpEF: Heart failure with EF ≥50%. The heart contracts normally but relaxes abnormally.
- HFrEF: Heart failure with EF < 40%, primarily due to weak contractions.
Understanding the Mechanism of HFpEF
Unlike HFrEF, HFpEF is primarily a result of diastolic dysfunction—the left ventricle (main pumping chamber) becomes stiff or hypertrophied (thickened), resulting in elevated pressure during filling. This stiffness means the heart cannot relax properly, reducing its capacity to fill with blood between beats. The preserved ejection fraction may mask underlying issues, making the condition challenging to identify and manage.
- Diastolic Dysfunction: The main culprit, involving stiffening of the heart muscle.
- Elevated Filling Pressures: Because the ventricle is stiff, higher pressure is needed to fill the chamber, leading to symptoms.
- Subtle Systolic Abnormalities: Some systolic (contractile) dysfunction may be present, especially apparent during exertion.
Prevalence and Risk Factors
HFpEF is becoming increasingly common, with rising incidence attributed to an aging population and higher prevalence of chronic conditions such as hypertension, obesity, and diabetes.
- Age: The most significant risk factor. HFpEF is far more prevalent in older adults.
- Sex: Occurs more frequently in women than men, though the reasons remain under study.
- Chronic conditions: Especially hypertension, diabetes, chronic kidney disease, and obesity.
- Other risk factors: Sedentary lifestyle, atrial fibrillation, and valvular heart disease.
Main Causes of HFpEF
HFpEF seldom stems from a single cause; rather, a combination of factors contributes to its onset. Notable underlying causes and comorbid conditions include:
- Age-related changes in heart muscle structure and function
- Longstanding high blood pressure (hypertension)
- Atrial fibrillation (irregular heartbeat)
- Coronary artery disease and myocardial ischemia
- Valvular heart diseases
- Chronic kidney disease
- Obesity or significant weight gain
- Uncontrolled diabetes mellitus
- Chronic inflammation
- Sedentary lifestyle
Symptoms of HFpEF
People with HFpEF frequently exhibit symptoms indistinguishable from other forms of heart failure. Often, these symptoms develop gradually and can worsen over time.
- Shortness of breath (dyspnea), especially with activity or when lying down
- Marked fatigue and reduced exercise tolerance
- Swelling (edema) in the legs, ankles, feet, or abdomen
- Persistent cough or wheezing
- Rapid or irregular heartbeat
- Frequent urination or reduced output
- Orthopnea (difficulty breathing when lying flat)
- Paroxysmal nocturnal dyspnea (waking at night with shortness of breath)
- Abdominal discomfort, anorexia, or unintentional weight gain
Is HFpEF Different from HFrEF?
Although both HFpEF and HFrEF share many clinical symptoms of heart failure, they differ in their underlying mechanisms, response to therapy, and patient demographics.
| Feature | HFpEF | HFrEF |
|---|---|---|
| Ejection Fraction | ≥ 50% (preserved) | < 40% (reduced) |
| Main Dysfunction | Diastolic (filling problem) | Systolic (pumping problem) |
| Common Patients | Older adults, women, hypertensive, obese | Broad demographic, often history of heart attack |
| Therapy Response | Limited evidence | Strong evidence for certain medications |
How is HFpEF Diagnosed?
Diagnosing HFpEF is challenging. Unlike HFrEF, which is primarily defined by a low ejection fraction, HFpEF requires a broader assessment. A careful evaluation typically includes:
- Patient history and physical examination
- Characteristic symptoms and signs of heart failure
- Echocardiography: To measure ejection fraction, assess diastolic function, chamber size, wall thickness, and filling pressures
- Biomarkers: Blood tests such as B-type natriuretic peptide (BNP) or NT-proBNP may indicate heart strain
- Other tests: ECG, chest X-ray, stress testing, or cardiac MRI may be ordered to rule out alternative causes or clarify the diagnosis
The diagnosis requires the combination of symptomatic heart failure, preserved ejection fraction (≥50%), and objective evidence of diastolic dysfunction or increased filling pressures. No single test is definitive—often, it’s the aggregate of findings that confirms HFpEF.
Complications of HFpEF
HFpEF increases the risk of complications across multiple organ systems. Common and serious complications include:
- Arrhythmias, especially atrial fibrillation
- Thromboembolic events (stroke, pulmonary embolism)
- Worsening chronic kidney disease
- Pulmonary hypertension (high pressure in the lungs), raising morbidity and mortality
- Liver congestion and dysfunction due to systemic fluid buildup
- Muscle wasting and weakness
Treatment Options for HFpEF
There is currently no cure for HFpEF, and management focuses on relieving symptoms, improving quality of life, and addressing underlying causes. Unlike HFrEF, for which several medications have robust evidence for improving survival, proven therapies for HFpEF are more limited.
Lifestyle Modifications
- Adopt a low-sodium (salt) diet to help control fluid retention
- Engage in regular physical activity tailored to ability
- Sustain a healthy weight
- Stop smoking and avoid excessive alcohol intake
- Monitor and control blood pressure, blood sugar, and cholesterol
Medical Therapies
- Diuretics: Mainstay of symptom control, reducing fluid overload and relieving edema and shortness of breath
- Blood pressure medications: Like ACE inhibitors, ARBs, and beta-blockers, may help in blood pressure management and possibly slow disease progression
- SGLT2 inhibitors: These diabetes medications have recently shown benefit in reducing hospitalizations in some patients with HFpEF
- Mineralocorticoid receptor antagonists: Sometimes used for symptom relief and reducing hospitalizations
- Medications for Atrial Fibrillation or other comorbidities: Managing concurrent arrhythmias or risk factors is critical
Monitoring and Interventions
- Regular follow-ups with a cardiologist or heart failure specialist
- Home monitoring of weight and symptoms for early detection of worsening fluid retention
- Device therapies in certain cases (e.g., pacemaker for arrhythmias)
Treatment should always be individualized. Many patients benefit from cardiac rehabilitation, which offers personalized exercise and education programs.
Living with HFpEF
People diagnosed with HFpEF can continue to lead fulfilling lives. Adherence to treatment regimens, ongoing symptom monitoring, and lifestyle adjustments are central to optimal outcomes. With proper management, many individuals experience improved well-being and fewer hospitalizations.
- Track symptoms and daily weight
- Communicate promptly with healthcare providers about new or worsening signs
- Keep up-to-date with vaccinations (influenza, COVID-19, pneumococcus) to reduce risk of respiratory complications
- Seek support through heart failure education programs, caregiver networks, and mental health resources
Prognosis and Outlook
Although HFpEF is a chronic and progressive condition, outcomes vary depending on age, sex, comorbidities, and adherence to treatment. HFpEF has a significant impact on quality of life and carries an increased risk for hospitalization and mortality, especially in people with multiple coexisting illnesses. Most deaths are due to non-cardiac causes, highlighting the importance of managing the full spectrum of health concerns.
Frequently Asked Questions (FAQs)
What is the main difference between HFpEF and HFrEF?
HFpEF involves a preserved ejection fraction (the heart pumps normally) but with impaired relaxation and filling (diastolic dysfunction). HFrEF is defined by a reduced ejection fraction due to impaired pumping (systolic dysfunction). Both share similar symptoms but differ in underlying mechanisms and, to some extent, in treatment approaches.
Who is at highest risk for developing HFpEF?
Older adults, women, and those with chronic high blood pressure, obesity, diabetes, atrial fibrillation, or kidney disease are at greatest risk. Lifestyle factors and lack of physical activity also play a role.
How is HFpEF diagnosed?
A thorough history, physical examination, echo-based heart function assessment, and lab tests are required. A combination of symptoms, preserved ejection fraction, and objective evidence of diastolic dysfunction secures the diagnosis.
Is HFpEF curable?
No cure currently exists, but symptoms can be managed and complications reduced with lifestyle modification, targeted treatments, and careful follow-up.
Can people with HFpEF live a normal life?
Yes, with consistent treatment and symptom monitoring, many can lead active, satisfying lives. Ongoing medical care and healthy living are crucial.
Key Takeaways
- HFpEF is a common type of heart failure marked by preserved ejection fraction but impaired filling (diastolic dysfunction).
- Risk increases with age, female sex, hypertension, obesity, and related chronic diseases.
- The main symptoms (breathlessness, swelling, fatigue) mirror those of other forms of heart failure.
- Diagnosis is complex and requires integrated assessment.
- Management focuses on lifestyle, symptom relief, and comorbidity control.
If you or a loved one has been diagnosed with HFpEF, ongoing dialogue with your healthcare team and proactive symptom management are the foundation of successful long-term care.
References
- https://www.tgh.org/institutes-and-services/conditions/heart-failure-preserved-ejection-fraction
- https://www1.racgp.org.au/ajgp/2019/july/heart-failure-with-preserved-ejection-fraction
- https://www.thecardiologyadvisor.com/ddi/hfpef-heart-failure-with-preserved-ejection-fraction/
- https://www.mayoclinic.org/medical-professionals/cardiovascular-diseases/news/heart-failure-with-preserved-ejection-fraction-hfpef-more-than-diastolic-dysfunction/mac-20430055
- https://my.clevelandclinic.org/health/diseases/22950-diastolic-heart-failure
- https://www.aafp.org/pubs/afp/issues/2017/1101/p582.html
- https://www.ncbi.nlm.nih.gov/books/NBK599960/
- https://www.mayoclinic.org/diseases-conditions/heart-failure/symptoms-causes/syc-20373142
- https://www.uchicagomedicine.org/conditions-services/heart-vascular/heart-failure/hfpef-clinic
Read full bio of Sneha Tete












