Heart Failure and Edema: Understanding the Connection, Symptoms, and Treatments
Explore the link between heart failure and edema, including causes, symptoms, treatment options, and patient care strategies.
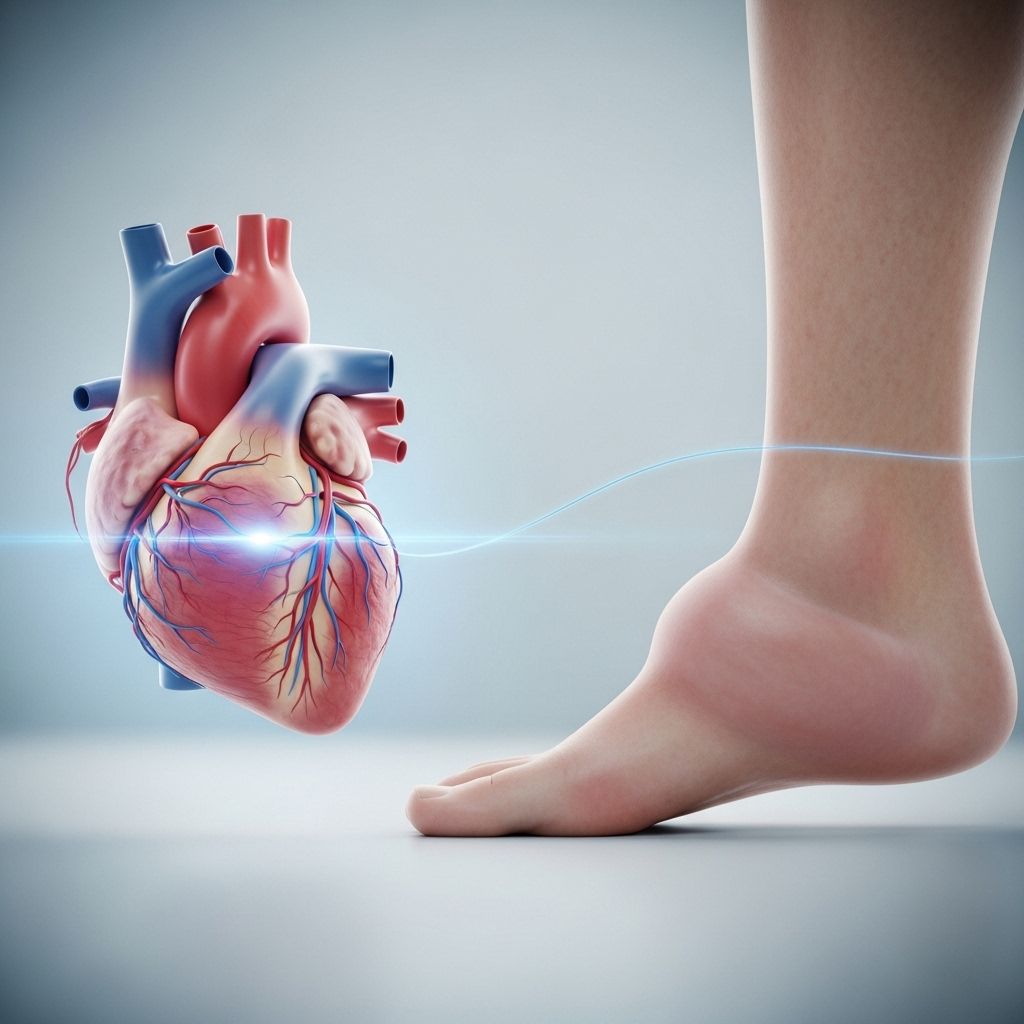
Edema, or swelling caused by fluid retention, often serves as a visible and significant indicator of underlying medical conditions. Among these, heart failure is a leading culprit, frequently resulting in excess fluid accumulating in tissues throughout the body. Recognizing and managing edema related to heart failure is critical for improving patient outcomes and quality of life.
Table of Contents
- What Is the Connection Between Heart Failure and Edema?
- How Does Edema Occur in Heart Failure?
- Symptoms and Types of Edema
- Types of Heart Failure
- Diagnosing Heart Failure and Edema
- Current Treatment Options for Edema in Heart Failure
- Self-Monitoring and Lifestyle Strategies
- Frequently Asked Questions
What Is the Connection Between Heart Failure and Edema?
Heart failure is a chronic condition in which the heart is unable to pump blood efficiently to meet the body’s needs. This impairment in cardiac function often leads to edema, a medical term for swelling caused by abnormal fluid buildup in the body’s tissues.
Edema in heart failure may develop because:
- The heart muscle weakens and struggles to circulate blood adequately.
- Blood pressure increases, causing fluid to back up and leak from blood vessels.
- Valvular heart disease (such as a leak in a heart valve) leads to fluid retention.
In essence, the body’s inability to return blood efficiently to the heart results in fluid seeping from capillaries into various tissues, especially the lower extremities. Edema is so closely linked to heart failure that, in many cases, it serves as either an early warning sign or an indicator of disease progression.
How Does Edema Occur in Heart Failure?
For the circulation system to work efficiently, the heart must generate enough pressure to keep blood moving through arteries and veins. In heart failure, the following processes are often at play:**
- The weakened heart can’t pump effectively, reducing circulation back to the heart and lungs.
- Higher blood pressure in the veins increases fluid pressure inside capillaries.
- This pressure drives fluid out of blood vessels and into surrounding tissues, especially in gravity-dependent areas like the lower legs, ankles, and feet.
Extensive fluid buildup manifests as swelling and sometimes as rapid, unexplained weight gain. Edema can progress to involve the abdomen (ascites) or lungs (pulmonary edema), triggering serious symptoms and necessitating urgent intervention.
Symptoms and Types of Edema
Edema resulting from heart failure is not uniform; it can present in different forms and locations depending on the severity and stage of the disease.
Common Signs and Symptoms
- Swelling in the feet, ankles, or legs (most frequent)
- Abdominal swelling (ascites)
- Rapid weight gain over a short period
- Shortness of breath, especially when lying flat
- Fatigue and decreased ability to exercise
- Feeling of suffocation or pressure in the chest
- Frequent need to urinate at night
- Swelling of the hands or arms (less common)
Types of Edema in Heart Failure
| Type | Description | Common Causes |
|---|---|---|
| Peripheral edema | Swelling in legs, feet, or ankles | Right-sided heart failure, chronic heart failure |
| Pulmonary edema | Fluid in the lungs, causing respiratory symptoms | Acute decompensated left-sided heart failure |
| Abdominal edema (ascites) | Swelling in the abdominal cavity | Chronic heart failure, especially with liver congestion |
Peripheral edema often develops gradually, while pulmonary edema may occur suddenly and constitute a medical emergency. Recognizing the differences is crucial for timely and appropriate management.
Types of Heart Failure Associated with Edema
Heart failure can be classified based on which part of the heart is affected and the underlying mechanisms at play. The connection between heart failure and edema varies depending on these types:
- Left-sided heart failure: Fails to deliver blood adequately to the body; most often leads to pulmonary edema.
- Right-sided heart failure: Fails to return blood from the body to the heart effectively; commonly results in peripheral (leg and abdominal) edema.
- Congestive heart failure: Involvement of both sides of the heart, typically causing both peripheral and pulmonary edema.
In practical terms, left-sided failure more often manifests with symptoms like shortness of breath and coughing, while right-sided failure is more likely to trigger swelling in the legs and abdomen.
Diagnosing Heart Failure and Edema
Diagnosing edema in the context of heart failure involves a combination of physical examination, patient history, and diagnostic testing. Proper assessment helps distinguish cardiac edema from swelling caused by other disorders, such as kidney disease, liver disease, or venous insufficiency.
Diagnostic Steps and Tests
- Physical Exam: Inspection of swollen limbs, pressing to check for ‘pitting’ (indentation remains after pressure), and assessment of heart and lung sounds.
- Patient Medical History: Questions about shortness of breath, recent weight gain, fatigue, or new limitations on activity.
- Blood Tests: Evaluation for factors such as anemia, kidney function, and B-type natriuretic peptide (BNP, elevated in heart failure).
- Imaging: Echocardiogram (ultrasound of the heart), chest X-ray, and less frequently, CT or MRI scans to assess heart structure and fluid accumulation.
- Electrocardiogram (EKG/ECG): Checks for abnormal heart rhythms or signs of prior injury.
- Urinalysis: Helps rule out kidney or metabolic contributors to edema.
Sometimes, more specialized tests are required to rule out other causes or understand the extent of heart failure progression.
Current Treatment Options for Edema in Heart Failure
Effective management of edema associated with heart failure focuses on treating the underlying cardiac dysfunction, as well as providing symptom relief from fluid accumulation. Treatment approaches may span lifestyle modifications, medications, and advanced interventions. The following options are commonly used:
Medications for Heart Failure and Edema
- Diuretics: Often referred to as “water pills,” these drugs help the body eliminate excess fluid by increasing urination. They are essential in reducing swelling and controlling blood pressure.
- ACE inhibitors, ARBs, or ARNI: These medications promote vessel relaxation, improving blood flow and lowering the heart’s workload.
- Beta blockers and Ivabradine: Both help slow the heart rate and decrease the heart’s demand for oxygen, making pumping more efficient.
- Mineralocorticoid Receptor Antagonists (MRAs): Can reduce salt retention and lower the risk of further cardiac events.
- SGLT2 Inhibitors: Originally developed for diabetes, these medications have proven beneficial in managing certain types of heart failure.
In severe cases—where medication and lifestyle modifications are insufficient—medical devices or surgical approaches may be required:
- Implantable pumps or defibrillators: Devices that support or regulate heart function.
- Heart transplant: Considered for advanced, end-stage heart failure when all other interventions fail.
Therapies and Physical Interventions
- Compression stockings: Increase pressure in lower legs to move blood back toward the heart and reduce swelling.
- Physical activity: Gentle exercise, as recommended by a physician, can support muscle action that moves fluid out of swollen tissues.
- Elevation: Raising the swollen area (e.g., legs) above the level of the heart can facilitate fluid return to central circulation.
Management of edema due to heart failure is often a lifelong, multidimensional process that may require periodic adjustments based on symptom fluctuations and routine monitoring.
Self-Monitoring and Lifestyle Strategies
Since heart failure is chronic, patients must take an active role in monitoring and managing their symptoms daily. Key lifestyle changes and self-care strategies include:
- Avoid alcohol and smoking: Both can worsen heart function and fluid retention.
- Adopt a heart-healthy diet: Focus on low-sodium, low-fat, high-fiber meals. Limit processed foods that may contain hidden salt.
- Follow an appropriate exercise routine: Engage in low-impact, physician-approved physical activity to maintain healthy circulation and heart strength.
- Weight management: Work with your healthcare provider to achieve and maintain a healthy body weight.
- Stress management: Utilize techniques such as mindfulness, breathing exercises, or counseling to reduce psychological strain, which can aggravate symptoms.
- Daily weight checks: Monitor and record your body weight each morning before breakfast to catch early signs of fluid retention.
- Keep all follow-up appointments and tests: Regular check-ups are crucial for medication adjustments and monitoring progress.
Active self-monitoring can help detect early warning signs of deteriorating heart function—such as sudden weight gain or increased leg swelling—allowing for timely medical intervention.
Frequently Asked Questions (FAQs)
What is edema and how is it linked to heart failure?
Edema refers to swelling from fluid leakage into tissues. In heart failure, the heart’s limited pump function causes blood to back up, raising pressure in the veins and forcing fluid into surrounding tissues, leading to swelling—often in the legs, ankles, feet, or abdomen.
What are the early signs of edema related to heart failure?
Early signs include swelling of the lower legs, rapid unexplained weight gain, feeling of tight shoes or socks, and, in some cases, shortness of breath that worsens when lying down.
Can edema be treated or reversed?
Yes. Effective management of the underlying heart failure—through medication, lifestyle modification, and sometimes devices or surgery—can decrease or even resolve edema. Prompt detection and intervention are essential for the best outcomes.
Is edema always a sign of heart failure?
No. Swelling (edema) may be caused by a range of disorders, including kidney disease, liver disease, certain medications, and venous insufficiency. A thorough medical assessment is needed to determine the cause.
What lifestyle changes can help reduce edema?
- Adhere to a low-sodium diet
- Exercise regularly within safety guidelines
- Elevate your legs when sitting or lying down
- Take medications as prescribed
- Avoid standing still for long periods
When should you seek immediate medical attention?
Seek emergency medical help if you experience:
- Suddent onset or severe shortness of breath
- Pain or pressure in the chest
- Swelling accompanied by confusion, fainting, or rapid heartbeat
These can be signs of acute pulmonary edema or worsening heart failure, which require urgent care.
How can patients living with heart failure monitor their condition at home?
- Track daily body weight to catch fluid buildup early
- Monitor swelling and shortness of breath
- Stay alert for any new or worsening symptoms and report them promptly to your healthcare provider
By understanding the linkage between heart failure and edema, recognizing symptoms, and adhering to recommended treatment and self-care strategies, patients can take control of their health and improve their overall quality of life.
References
- https://www.healthline.com/health/heart-failure/heart-failure-edema
- https://pubmed.ncbi.nlm.nih.gov/23319101/
- https://www.rwjbh.org/treatment-care/heart-and-vascular-care/diseases-conditions/cardiac-edema/
- https://www.mayoclinic.org/diseases-conditions/edema/symptoms-causes/syc-20366493
- https://my.clevelandclinic.org/health/diseases/17069-heart-failure-understanding-heart-failure
- https://www.mayoclinic.org/diseases-conditions/heart-failure/symptoms-causes/syc-20373142
- https://my.clevelandclinic.org/health/diseases/12564-edema
- https://www.nhs.uk/conditions/heart-failure/treatment/
- https://www.webmd.com/heart-disease/heart-failure/edema-overview
Read full bio of Sneha Tete












