Heart Attack vs. Heart Failure: Understanding Key Differences, Symptoms, and Treatments
Distinguish between heart attack and heart failure, their symptoms, risk factors, and effective management for better cardiovascular health.
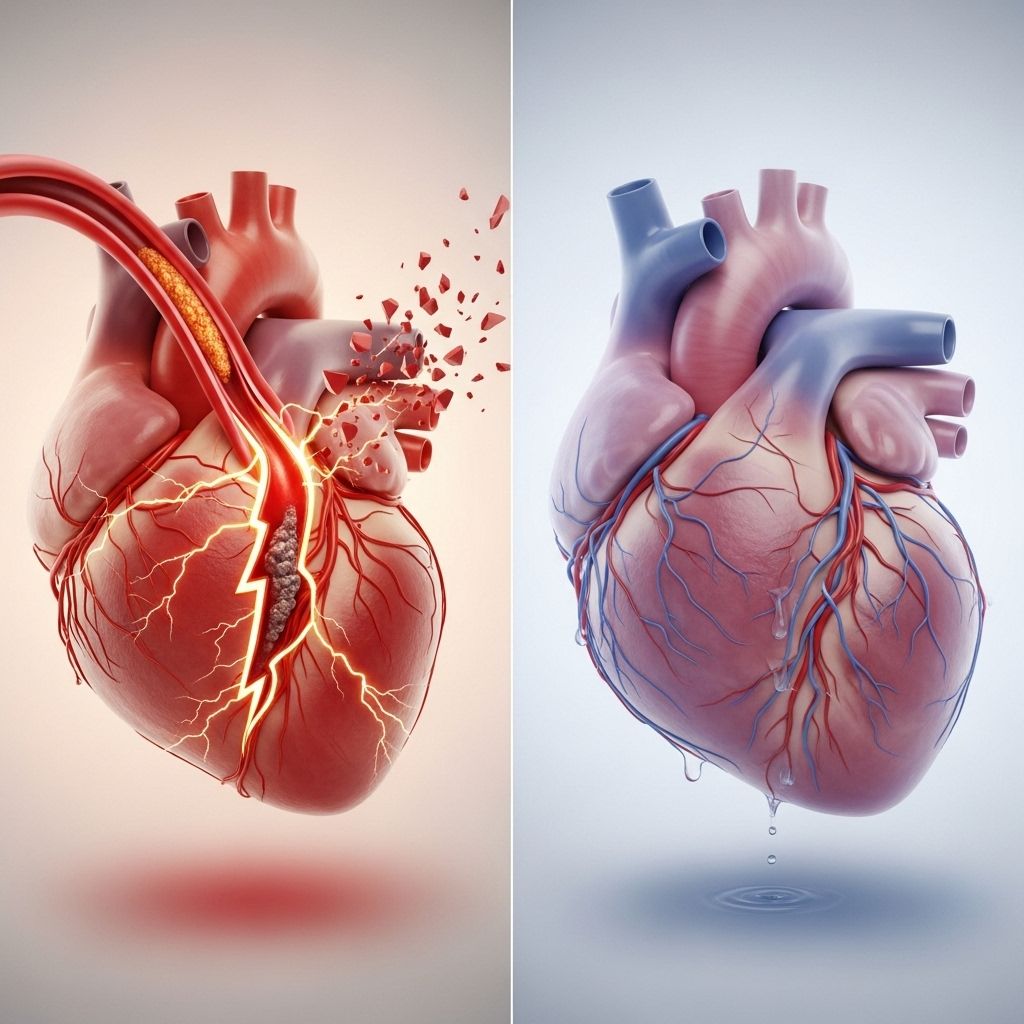
Heart Attack vs. Heart Failure: What You Need to Know
Heart health is crucial to overall wellbeing, yet many people often confuse the terms heart attack and heart failure. Though they’re both serious heart conditions, their causes, symptoms, and treatments differ significantly. Understanding these differences is essential for prevention, timely response, and effective management.
What Is a Heart Attack?
A heart attack (medically known as myocardial infarction) occurs when blood flow to part of the heart muscle becomes blocked. This blockage is typically due to a build-up of fatty deposits, cholesterol, or clots in the coronary arteries. Without sufficient oxygen-rich blood, heart muscle tissue can quickly become damaged or die.
During a heart attack, the heart continues to beat, but part of its tissue is starved of blood and oxygen, posing a potentially life-threatening emergency that requires immediate medical intervention.
What Is Heart Failure?
Heart failure is a chronic condition where the heart is unable to pump blood effectively to meet the body’s needs. This ineffectiveness leads to fluid build-up and prevents organs and tissues from receiving adequate oxygen and nutrients. Heart failure usually develops over time as the heart muscle becomes weakened or stiff due to conditions like high blood pressure or coronary artery disease.
- Left-sided heart failure: Affects the ability of the heart to send blood from the lungs to the rest of the body.
- Right-sided heart failure: Impacts blood flow from the body to the lungs.
- Biventricular heart failure: Involves both sides of the heart, compounding symptoms.
Key Differences at a Glance
| Feature | Heart Attack | Heart Failure |
|---|---|---|
| Primary cause | Blocked coronary arteries | Weakening or stiffening of heart muscle |
| Onset | Sudden (acute event) | Gradual (chronic condition) |
| Main symptoms | Chest pain, shortness of breath, nausea | Shortness of breath, fatigue, fluid retention |
| Treatment urgency | Emergency (call 911) | Long-term management |
| Outcome without treatment | Potentially fatal in minutes to hours | Deteriorates over months/years |
Symptoms: How Do Heart Attack and Heart Failure Manifest?
While there may be overlap in some symptoms, certain signs are characteristic of each condition. Recognizing these can aid in seeking the right care, fast.
Heart Attack Symptoms
- Chest pain or discomfort: Often described as pressure, squeezing, fullness, or pain. Pain may radiate to the arms, shoulders, back, neck, or jaw.
- Shortness of breath: Even at rest or during mild exertion.
- Cold sweats: Sudden, intense sweating.
- Dizziness or lightheadedness: Feeling faint or weak.
- Nausea or vomiting: Particularly common in women.
- Unusual fatigue: Extreme tiredness, sometimes with no other classic symptoms of chest pain.
- Pain in other areas: Upper body pain or discomfort, not just the chest.
Unique Considerations
Some people, such as women and individuals with diabetes, may experience atypical symptoms (e.g., fatigue, weakness) and may not have classic chest pain.
Heart Failure Symptoms
- Shortness of breath: Especially when exercising, lying down, or sleeping. May worsen over time.
- Fatigue or weakness: Tiredness that’s persistent with minimal activity.
- Swelling (edema): Particularly in the feet, ankles, legs, and sometimes abdomen.
- Coughing or wheezing: More pronounced during physical activity or while lying flat.
- Rapid or irregular heartbeat: May feel like a fluttering or pounding in the chest.
- Confusion or trouble concentrating: Due to inadequate blood flow to the brain.
- Weight gain: From fluid retention.
- Other signs: Blue-tinted fingernails or lips, loss of appetite, abdominal pain, and frequent urination (especially at night).
Causes and Risk Factors
Understanding the root causes and key risk factors helps reduce the likelihood of experiencing either condition.
Heart Attack Causes and Risk Factors
- Coronary artery blockage: Typically via atherosclerosis (fatty plaques), cholesterol, or blood clots.
- High blood pressure
- Diabetes
- High cholesterol
- Obesity
- Smoking
- Family history: Genetics play an important role.
- Age: Risk increases after age 45 (men) and age 55 (women).
Heart Failure Causes and Risk Factors
- Coronary artery disease: The most common cause of heart failure.
- Previous heart attacks: Can weaken heart muscle function.
- High blood pressure: Puts extra strain on the heart.
- Diabetes
- Valve disorders: Malfunctioning valves impair heart’s ability to pump efficiently.
- Cardiomyopathy: Disease of the heart muscle.
- Obesity and inactivity
- Older age
- Men: Slightly higher risk of heart failure compared to women.
Diagnosis
Both heart attack and heart failure require medical diagnosis. Immediate evaluation is critical for a heart attack, while heart failure is usually diagnosed and managed over time.
Diagnosing Heart Attack
- Electrocardiogram (ECG): Shows heart rhythm and signs of muscle damage.
- Blood tests: Detect markers released during heart tissue injury.
- Coronary angiography: Identifies blocked arteries.
- Imaging: Echocardiogram or chest X-ray may confirm diagnosis.
Diagnosing Heart Failure
- Physical examination: Evaluates symptoms and signs such as swelling.
- Imaging: Echocardiogram assesses heart function and structure.
- ECG and blood tests: May also be used to detect underlying causes and monitor progression.
- Chest X-ray: Can reveal fluid buildup in the lungs.
Treatment Options
Treatment approaches depend significantly on the condition, its severity, and patient circumstances.
Managing and Treating Heart Attack
- Immediate action: Call 911. Early intervention saves lives.
- Emergency treatments:
- Aspirin: Blood-thinning to reduce clotting.
- Nitroglycerin: Helps improve blood flow.
- Oxygen therapy: If required.
- Medical procedures:
- Percutaneous coronary intervention (PCI): Balloon angioplasty to open blocked artery, often with stent placement.
- Coronary artery bypass grafting (CABG): Uses healthy vessels to reroute blood around blockage.
- Long-term medications:
- Blood pressure drugs
- Cholesterol-lowering medications
- Medications to prevent future clots
- Lifestyle modifications: Diet, exercise, tobacco cessation, and stress management.
Managing and Treating Heart Failure
- Underlying cause: Treatment focuses on addressing what led to heart failure (e.g., managing blood pressure, diabetes).
- Medications: Diuretics to remove excess fluid, ACE inhibitors or beta-blockers to improve heart function.
- Medical devices: Implantable devices (e.g., pacemakers, defibrillators) help regulate abnormal heart rhythms.
- Lifestyle modifications:
- Low-sodium diet
- Weight management
- Monitored exercise plans
- Regular monitoring: Frequent medical check-ups to track progression and adjust treatments.
Complications
- Heart attack: Can lead to heart failure if a significant part of the heart muscle is damaged and no longer pumps effectively.
- Heart failure: Increases risk for arrhythmias, fluid buildup in lungs (pulmonary edema), kidney damage, and other organ dysfunction.
Long-Term Outlook and Prevention
Living with heart disease means prioritizing prevention, early diagnosis, and ongoing management.
- Prevention strategies: Healthy diet, regular physical activity, avoiding tobacco, managing blood pressure and cholesterol, monitoring blood sugar, routine check-ups.
- Prognosis: Many heart attack survivors recover well with modern treatments, but risk of future attacks remains. Heart failure requires lifelong management.
- Emergency preparedness: Easy access to emergency numbers, knowing CPR and heart attack warning signs can save lives.
Frequently Asked Questions (FAQs)
What is the main difference between a heart attack and heart failure?
A heart attack is an acute event caused by blocked blood flow to the heart muscle, while heart failure is a chronic condition where the heart cannot pump blood effectively.
Can a heart attack lead to heart failure?
Yes. Severe damage from a heart attack may weaken the heart muscle and ultimately result in heart failure.
Are the symptoms of heart attack and heart failure the same?
Some symptoms overlap, such as shortness of breath and fatigue. However, chest pain is more characteristic of a heart attack, while swelling and fluid retention are signs of heart failure.
How can heart attack and heart failure be prevented?
Adopting healthy lifestyle habits like eating well, regular exercise, avoiding tobacco, and managing chronic conditions can reduce your risk for both.
When should I seek medical help for heart symptoms?
Call 911 right away if you have chest pain, severe breathlessness, fainting, or other sudden symptoms. Timely treatment is critical, especially for heart attack.
Conclusion
Distinguishing between heart attack and heart failure empowers patients and families to seek timely care and improve outcomes. While heart attack strikes suddenly due to arterial blockage, heart failure emerges gradually as the heart’s pumping ability declines. Recognizing key symptoms—chest pain for heart attack, swelling and persistent shortness of breath for heart failure—can be lifesaving. Ultimately, prevention and appropriate medical management form the cornerstone of heart health for adults of all ages.
References
- https://www.healthline.com/health/heart/heart-attack-vs-heart-failure
- https://www.baptisthealth.com/blog/heart-care/the-difference-between-heart-attack-heart-failure-cardiac-arrest
- https://www.goodrx.com/conditions/heart-attack/heart-attack-vs-heart-failure
- https://www.webmd.com/heart-disease/heart-failure/heart-attack-vs-heart-failure
- https://www.mountcarmelhealth.com/blog-articles/heart-attack-vs-cardiac-arrest-vs-heart-failure
- https://www.cedars-sinai.org/blog/heart-attack-cardiac-arrest-and-heart-failure.html
- https://www.youtube.com/watch?v=JV60tPRJMXQ
- https://www.heart.org/en/health-topics/heart-attack/about-heart-attacks/heart-attack-or-sudden-cardiac-arrest-how-are-they-different
Read full bio of medha deb












