Grey Spots on the White of the Eye: Causes, Concerns, and Treatments
Uncover the causes, implications, and management of grey spots on the sclera to safeguard your ocular health.
Grey Spots on the White of the Eye: What You Should Know
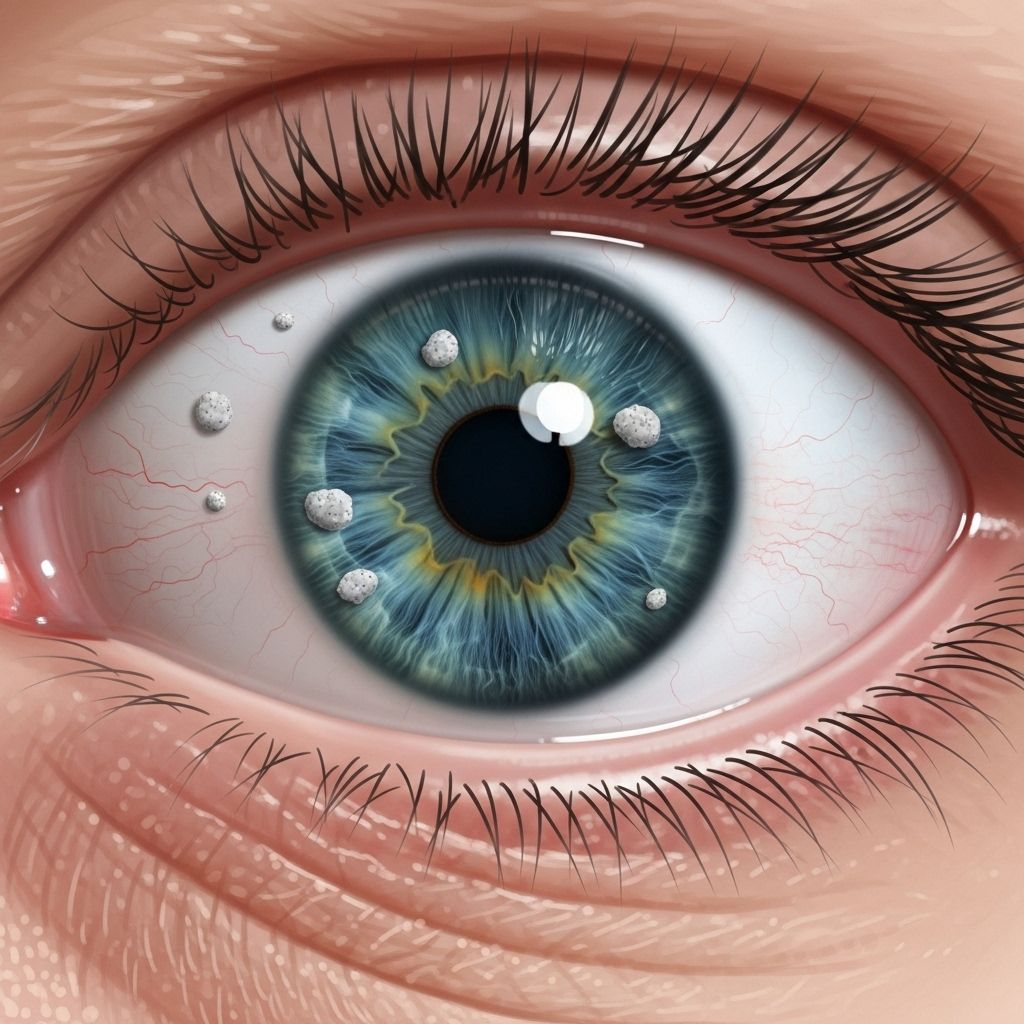
A greyish spot on the white of the eye—the sclera—can be startling when first noticed. While some causes are harmless, others may signal underlying eye health issues requiring attention. Understanding the potential origins and implications of these spots is vital for protecting your ocular health.
Recognizing a Grey Spot on the Sclera
When the sclera, which is normally white, develops a grey or slate-colored spot, it may arise due to a range of benign or more serious conditions. Some key points include:
- Spots may be congenital (present from birth) or acquired later in life.
- Locations: The spot can appear anywhere on the visible white of the eye.
- Changes in appearance: If the spot changes in size, shape, elevation, or color, medical attention is advised.
Spots may not cause symptoms, but new or evolving ones should be professionally evaluated to ensure proper care.
Common Causes of Grey Spots on the White of the Eye
Several distinct conditions can lead to the appearance of a grey spot on the sclera. Below are some of the most frequent causes, how they present, and their implications for eye health.
1. Scleral Melanocytosis
Scleral melanocytosis is a benign condition involving an accumulation of melanocytes (pigment cells) within the sclera. It most often appears as a blue-grey patch, commonly present from birth but may become more visible over time.
- Appears as a flat, non-elevated grey or blue spot.
- Frequently affects people of Asian or African descent.
- Generally harmless but should be monitored for changes.
Although typically benign, any change in appearance warrants examination to rule out rare progression to more serious conditions.
2. Senile Scleral Plaques
In older adults, senile scleral plaques are a common, benign cause of grey spots. These plaques appear as oblong, slate-grey patches, most often found near the outer edge of the iris (posterior to the limbus but anterior to the horizontal rectus muscle insertions).
- Tend to affect people over 70, more common in women.
- Often discovered during routine eye exams as they usually cause no symptoms.
- Due to hyaline degeneration (age-related tissue change) of the sclera, exposing underlying pigmented tissue.
3. Conjunctival Melanosis
Conjunctival melanosis refers to increased pigmentation on the conjunctiva (the thin tissue over the sclera). Types include:
- Racial conjunctival melanosis: Benign, most prevalent in individuals with darker skin tones. Usually present from an early age and rarely changes over time.
- Acquired conjunctival melanosis: May arise later in life and can, rarely, represent a risk for malignant transformation, particularly if the spot changes or grows.
Regular monitoring is advised, especially if there are notable changes in the pigmented area.
4. Primary Acquired Melanosis (PAM)
PAM is a unilateral, flat, brown or grey patch that develops later in life. While most cases are benign, some with atypical features can progress to conjunctival melanoma.
- May slowly increase in size or change in pigmentation.
- Professional monitoring and sometimes biopsy are necessary to assess cancer risk.
5. Oculodermal (Nevus of Ota) Melanocytosis
This rare, congenital condition is characterized by blue-grey pigmentation of both the eye and the skin around the eye.
- Pigmentation usually involves the sclera, conjunctiva, uveal tract, and surrounding skin.
- People with this disorder have an increased risk of glaucoma and uveal melanoma.
6. Other Pigmented Lesions
Less commonly, a greyish spot may indicate ocular nevi (benign moles of the eye) or, very rarely, melanomas. Ocular melanoma, although uncommon, is the most frequent primary cancer of the eye in adults and requires urgent attention.
- Most nevi do not change over time.
- Melanoma is typically associated with rapid change, irregular borders, or elevation.
Symptoms Accompanying Grey Spots
While many grey spots do not result in symptoms, the following can warrant immediate or prompt evaluation:
- Changes in vision, such as blurring or greyed-out visual fields.
- Pain or discomfort in the eye.
- Redness, swelling, or tenderness.
- Sensation of a foreign body or irritation.
Presence of any of these symptoms, or changes in the appearance of a spot, should prompt an eye care professional’s review.
When to Seek Medical Advice
- If the grey spot is new, expanding, raised, or changing color.
- Accompanied by symptoms such as pain, vision loss, or eye redness.
- Personal or family history of eye cancers or pigmented lesions.
Benign spots are typically harmless, but regular monitoring helps distinguish them from conditions that require treatment.
Diagnosing Grey Spots on the Eye
An ophthalmologist or optometrist can usually diagnose the cause of a grey spot through a thorough eye examination and history. Steps include:
- Detailed medical and ocular history.
- Visual inspection using slit lamp examination.
- Photography or measurement for tracking changes.
- Advanced imaging (OCT, ultrasound, or biopsy) when malignancy or rare disorders are suspected.
The precise diagnosis guides management—whether observation, further testing, or treatment is required.
Treatment Options for Grey Spots on the Sclera
Many grey spots are benign and do not require treatment beyond observation. However, management varies depending on the underlying cause:
- Benign Melanocytosis and Plaques: No treatment necessary unless significant change occurs; regular eye exams suffice.
- Pigmented Lesions with Change: Lesions that grow, change color, or become raised may need biopsy to rule out melanoma, with oncology referral if confirmed.
- Complications (e.g., Glaucoma): In cases of oculodermal melanocytosis increasing risk for glaucoma, intraocular pressure monitoring and treatment may be needed.
- Associated discomfort: Lubricating eye drops or anti-inflammatory medications if irritation is present.
Rare But Serious Scenarios
- Ocular melanoma: May require surgery, radiotherapy, or other cancer-specific therapies.
- Foreign bodies: Embedded objects may require removal and antibiotic prophylaxis.
Prevention and Eye Health Tips
While not all grey spots can be prevented, several steps help maintain ocular health and minimize risks:
- Wear high-quality sunglasses to block ultraviolet (UV) light, reducing pigment changes from sun exposure.
- Schedule regular eye examinations, particularly if you have risk factors for melanoma or other eye conditions.
- Avoid rubbing eyes vigorously, especially if you notice new spots.
- Report any persistent or changing eye changes to an eye care professional promptly.
Frequently Asked Questions (FAQs)
Q: Why do I have a grey spot on the white of my eye?
A grey spot may result from harmless pigment accumulations, such as scleral melanocytosis, or be due to benign conjunctival nevi. Less commonly, it could be a sign of underlying inflammation, age-related plaque, or, rarely, melanoma. Any new or changing spot should be evaluated by an eye specialist to ensure it is not a sign of a more serious condition.
Q: Is a grey spot on my eye a sign of cancer?
Most grey spots are benign, but rarely, a pigmented spot may represent ocular melanoma or another malignancy, especially if it grows or changes appearance. Eye professionals can differentiate benign from malignant lesions with proper examination and recommend monitoring or treatment as necessary.
Q: Are there risk factors for developing pigmented eye spots?
Having darker skin, a family history of pigmented lesions, frequent UV exposure, or congenital syndromes may increase the likelihood of developing benign spots. Oculodermal melanocytosis, a rare congenital condition, can elevate the risk of eye cancer and glaucoma.
Q: Can I prevent grey spots on my sclera?
While most grey spots are not preventable, UV protection with sunglasses and regular eye exams can help lower risks of UV-induced changes and catch early signs of concerning conditions.
Q: What should I do if the spot is growing or changing?
Seek prompt evaluation by an ophthalmologist. Changes in size, color, elevation, or associated symptoms require a thorough assessment to rule out concerning pathology.
Summary Table: Key Causes of Grey Spots on the Sclera
| Condition | Description | Common Age | Symptoms | Treatment |
|---|---|---|---|---|
| Scleral Melanocytosis | Benign blue-grey pigment in sclera | Children, persists lifelong | None, visible discoloration only | Observation |
| Senile Scleral Plaque | Age-related, oblong grey area | 70+ | None | None needed |
| Conjunctival Melanosis | Pigmentation in conjunctiva | Any (racial); adults (acquired) | None, rarely changes | Observation, monitor for changes |
| Oculodermal Melanocytosis | Congenital, also affects facial skin | Birth | None, but risk of glaucoma/cancer | Monitoring, glaucoma/cancer screening |
| Melanoma | Cancerous growth | Adults | Growth, shape/color change, visual symptoms | Surgical/oncologic therapy |
Takeaway: Partnering with Your Eye Care Provider
If you observe a grey spot on the white of your eye, do not panic. While most lesions are harmless, only an ophthalmologist can distinguish benign conditions from rare but serious disorders. Regular eye exams and prompt attention to changes remain the best way to preserve your ocular health and peace of mind.
References
- https://mycorneacare.com/eye-health-and-wellness/grey-spot-on-white-of-eye/
- https://www.healthline.com/health/eye-health/white-spot-in-eye
- https://www.medicalnewstoday.com/articles/319490
- https://www.allaboutvision.com/conditions/related/brushfield-spots/
- https://my.clevelandclinic.org/health/symptoms/leukocoria
- https://www.medicalnewstoday.com/articles/319887
Read full bio of Sneha Tete












